Category: Critical Care
Keywords: analgosedation, sedation, intubation, (PubMed Search)
Posted: 8/23/2022 by Kami Windsor, MD
Click here to contact Kami Windsor, MD
Deep sedation in the ED has previously been associated with longer duration of mechanical ventilation, longer lengths of stay, and higher mortality.1 Current guidelines recommend light sedation, consistent with a goal RASS of -2 to 0, for most critically-ill patients in the ICU.2
The ED-SED3 multicenter, pragmatic, before-and-after feasibility study implemented an educational initiative (inservices, regular reminders, laminated sedation charts) to help target lighter sedation depths in newly-intubated adult patients without acute neurologic injury or need for prolonged neuromuscular blockade.
After educational intervention:
Even with the caveats of the confounding and bias that can exist in before-and-after studies, these results are consistent with prior sedation-related studies and offer more evidence to support for avoiding deep sedation in our ED patients. The study also demonstrates the importance of nurse-driven sedation in achieving sedation goals.
Bottom Line: Our initial care in the ED matters beyond initial stabilization and compliance with measures and bundles. Avoid oversedating intubated ED patients, aiming for a goal RASS of -2 to 0.
Category: Pediatrics
Keywords: COVID, kids, masking, school (PubMed Search)
Posted: 8/19/2022 by Jenny Guyther, MD
(Updated: 2/1/2026)
Click here to contact Jenny Guyther, MD
This was a multistate, prospective, observational cohort of children and teachers attending in person schools in kindergarden through 12th grade where the school districs had the ability to perform contact tracing and determine primary vs secondary infections. During the study period (6/21-12/21) 46 districts had universal masking policies and 6 districts had optional masking policies.
Districts that optionally masked had 3.6x the rate of secondary transmission compared to universally masked school districts. Optionally masked districts had 26.4 cases of secondary transmission per 100 community acquired cases compared to only 7.3 cases in universally masked districts.
Bottom line: Universial masking was associated with reduced secondary transmission of SARS-CoV2 compared with optional masking policies.
Boutzoukas AE, Zimmerman KO, Inkelas M, et al. School Masking Policies and Secondary SARS-CoV-2 Transmission. Pediatrics. 2022;149 (6):e2022056687.
Category: Critical Care
Keywords: Calcium, Cardiac Arrest, ACLS, Code Blue (PubMed Search)
Posted: 8/16/2022 by Mark Sutherland, MD
Click here to contact Mark Sutherland, MD
We previously posted on the COCA trial, which looked at empiric calcium administration in cardiac arrest. They studied 391 adult Danish cardiac arrest patients. The immediate and 30 day outcomes showed no benefit, and in fact strongly trended towards calcium being WORSE than placebo. This article provides the 6 month and 1 year follow up data. Surprise, surprise... calcium is still not looking good.
At 6 months survival non-significantly favored the placebo group, and at 1 year it significantly favored the placebo group. Neurologic outcome for those who survived was also no better, and perhaps slightly worse, in the calcium group.
Importantly, the trial excluded patients with "traumatic cardiac arrest, known or suspected pregnancy, prior enrollment in the trial, adrenaline prior to possible enrollment, and clinical indication for calcium at the time of randomization."
Bottom Line: The evidence continues to not support the routine empiric administration of calcium in cardiac arrest. Patients in whom there is an indication to give calcium (e.g. known ESRD, suspected hyperkalemia, etc) are excluded from these trials, and should likely still receive empiric calcium, but in undifferentiated cardiac arrest you can probably skip the calcium.
Vallentin MF, Granfeldt A, Meilandt C, Povlsen AL, Sindberg B, Holmberg MJ, Iversen BN, Mærkedahl R, Mortensen LR, Nyboe R, Vandborg MP, Tarpgaard M, Runge C, Christiansen CF, Dissing TH, Terkelsen CJ, Christensen S, Kirkegaard H, Andersen LW. Effect of calcium vs. placebo on long-term outcomes in patients with out-of-hospital cardiac arrest. Resuscitation. 2022 Jul 30;179:21-24. doi: 10.1016/j.resuscitation.2022.07.034. Epub ahead of print. PMID: 35917866.
Category: Orthopedics
Keywords: Dislocation, reduction, AVN (PubMed Search)
Posted: 8/13/2022 by Brian Corwell, MD
Click here to contact Brian Corwell, MD
The hip joint is a very strong and stable structure requiring great force to produce a dislocation
Most hip dislocations are posterior (80-90%)
Mechanism: MVC generating force onto an adducted flexed hip (most commonly)
Associated injuries occur both locally (acetabular fx) and distant (knee bone and ligamentous)
Significant associated injuries in >70%
The hip joint has a very precarious blood supply.
One of the risk factors for AVN is total dislocation time
<6 hours - 5% incidence
>6 hours – up to 53% incidence
Examine the sciatic nerve carefully with posterior dislocations (10% incidence)
Motor – EHL/ankle dorsiflexion
Sensory – sensation dorsum of foot
There are many reduction maneuvers including the East Baltimore Lift technique
https://www.youtube.com/watch?v=1zvelGbVn04
Demonstrated at 30 seconds in above video
Place patient supine with affected leg flexed to 90 degrees at knee and hip. 2 providers position themselves on opposite sides of the patient and each places their arm under the patient’s calf/popliteal region and their hand on the opposite providers shoulder. A 3rd person is required to stabilize the pelvis. Axial traction is generated by the providers slowly standing up. Gentle internal and external rotation can facilitate successful reduction
Category: Critical Care
Posted: 8/9/2022 by Mike Winters, MBA, MD
(Updated: 2/1/2026)
Click here to contact Mike Winters, MBA, MD
Diastolic Blood Pressure
Hernandez G, et al. Invasive arterial pressure monitoring: much more than mean arterial pressure! Intensive Care Med. 2022. Published online ahead of print.
Category: Pediatrics
Keywords: pediatric trauma, tranexamic acid (PubMed Search)
Posted: 8/5/2022 by Rachel Wiltjer, DO
Click here to contact Rachel Wiltjer, DO
Bottom line: There is not clear evidence for efficacy, but trends are positive and the documented rates of adverse effects in this population are low. It is reasonable to give, especially in patients requiring massive transfusion or who are critically ill.
Eckert MJ, Wertin TM, Tyner SD, et al. Tranexamic acid administration to pediatric trauma patients in a combat setting: the pediatric trauma and tranexamic acid study (PED-TRAX). J Trauma Acute Care Surg. 2014;77(6):852-858.
Hamele M, Aden JK, Borgman MA. Tranexamic acid in pediatric combat trauma requiring massive transfusions and mortality. J Trauma Acute Care Surg. 2020;89(2S Suppl 2):S242-S245.
Nishijima, DK, VanBuren, JM, Linakis, SW, et al. Traumatic injury clinical trial evaluating tranexamic acid in children (TIC-TOC): A pilot randomized trial. Acad Emerg Med. 2022; 29: 862– 873.
Category: Critical Care
Keywords: Hemodynamics, Intubation, RSI, Shock (PubMed Search)
Posted: 8/3/2022 by Lucas Sjeklocha, MD
Click here to contact Lucas Sjeklocha, MD
Hemodynamic instability and cardiac arrest are major complications following endotracheal intubation. The mantra “resuscitate before you intubate” has prompted several studies of how to prevent this.
The PREPARE II trial is a multicenter ICU-based trial studying the effect of 500cc of crystalloid versus no crystalloid pre-emptively to prevent hypotension following endotracheal intubation. The study enrolled 1067 critically ill patients in United States ICUs. Some 60% of patient were intubated for respiratory failure and 20% were already on vasopressor. The primary induction drugs we etomidate and rocuronium. Importantly, urgent intubation was an exclusion. There were no differences in multiple endpoints including hypotension, new need for vasopressors, cardiac arrest, or 28-day mortality.
This was in some ways this in not unexpected and patients already in an ICU setting have typically received some form of fluid loading already. Being ICU based and primarily a more smoldering medical population this has limited application to more emergent and undifferentiated settings, but study underscores the need for a broad and nuanced view of what “resuscitate” means. Positive pressure may exacerbate hypovolemia, but the patient’s underlying disease, the effect of anesthetic drugs both by direct action via relief of pain, discomfort, or dyspnea may predominate if you think the patient is euvolemic.
Remember to dose anesthetics/sedatives/RSI drugs with an eye toward hemodynamics and consider starting vasopressors prior to intubation
Bottom Line:
-In a broad well-conducted ICU-based study a 500cc peri-intubation bolus doesn’t prevent hypotension
-Have a broad view of what resuscitation for intubation might entail
-Having fluid ready for intubation is helpful, hemodynamic dosing of drugs and having a plan for vasopressors might be even more helpful
-Applicability to ED environments is limited in this ICU-based trial
JAMA. 2022;328(3):270-279. doi:10.1001/jama.2022.9792
Category: Critical Care
Keywords: Awareness, mechanical ventilation, Emergency Department, Rocuronium (PubMed Search)
Posted: 7/26/2022 by Quincy Tran, MD, PhD
(Updated: 2/1/2026)
Click here to contact Quincy Tran, MD, PhD
Have you ever wonder what patients feel after being intubated in the ED?
The study " Awareness With Paralysis Among Critically Ill Emergency Department Patients: A Prospective Cohort Study" aimed at answering just that.
Settings: Emergency Departments from 3 hospitals; This was a secondary analysis of a prospective trial.
Patients:
Patients who received neuromuscular blockade in ED
Intervention: None.
Comparison: None.
Outcome: Primary outcome was Awareness while paralyzed, secondary outcome was Perceived threat, which is considered the pathway for PTSD.
Study Results:
The study evaluated 388 patients. There were 230 (59%) patients who received rocuronium.
Patients who received rocuronium (5.5%, 12/230) were more likely to experience awareness than patients receiving other neuromuscular blockade (0.6%, 1/158).
Patients who experienced awareness during paralysis had a higher threat perception score that those who did not have awareness (15.6 [5.8] vs. 7.7 [6.0], P<0.01).
A multivariable logistic regression, after adjustment for small sample size, showed that Rocuronium in the ED was significantly associated with awareness (OR 7.2 [1.39-37.58], P = 0.02).
Discussion:
With the increasing use of rocuronium for rapid sequence intubation in the ED, clinicians should start to pay more attention to the prevalence of awareness during paralysis. According to the study, patients reported pain from procedures, being restrained, and worst of all feelings of impending death.
One of the risk factors for awareness during paralysis would be the long half-life of rocuronium, compared to that of succinylcholine. Therefore, clinicians should consider prompt and appropriate dosage of sedatives for post-intubation sedation. Previous studies showed that a mean time from intubation till sedatives was 27 minutes (2), and propofol was started at a low dose of 30 mcg/kg/min for ED intubation (3).
Conclusion:
Approximately 5.5% of all patients or 4% of survivors of patients who had invasive mechanical ventilation in the ED experienced awareness during paralysis. They also were at high risk for PTSD.
1. Fuller BM, Pappal RD, Mohr NM, Roberts BW, Faine B, Yeary J, Sewatsky T, Johnson NJ, Driver BE, Ablordeppey E, Drewry AM, Wessman BT, Yan Y, Kollef MH, Carpenter CR, Avidan MS. Awareness With Paralysis Among Critically Ill Emergency Department Patients: A Prospective Cohort Study. Crit Care Med. 2022 Jul 22. doi: 10.1097/CCM.0000000000005626. Epub ahead of print. PMID: 35866657.
2. Watt JM, Amini A, Traylor BR, Amini R, Sakles JC, Patanwala AE. Effect of paralytic type on time to post-intubation sedative use in the emergency department. Emerg Med J. 2013 Nov;30(11):893-5. doi: 10.1136/emermed-2012-201812. Epub 2012 Nov 8. PMID: 23139098.
3. Korinek JD, Thomas RM, Goddard LA, St John AE, Sakles JC, Patanwala AE. Comparison of rocuronium and succinylcholine on postintubation sedative and analgesic dosing in the emergency department. Eur J Emerg Med. 2014 Jun;21(3):206-11. doi: 10.1097/MEJ.0b013e3283606b89. PMID: 23510899.
Category: Orthopedics
Keywords: AVN, wrist pain, lunate (PubMed Search)
Posted: 7/23/2022 by Brian Corwell, MD
(Updated: 2/1/2026)
Click here to contact Brian Corwell, MD

Kienbock’s disease: collapse of the lunate due to avascular necrosis and vascular insufficiency.
Occurs most commonly in young adults aged 20 to 40 years.
Cause is unknown but believed to be due to remote trauma or repetitive microtrauma in at risk individuals.
On exam, limited range of motion, decreased grip strength and passive dorsiflexion of the 3rd digit produces pain.
Dx: plain film in the ED and with MRI as an outpatient.
Tx: Wrist immobilization with splint and refer to orthopedics as treatment is individualized.
Category: Critical Care
Posted: 7/19/2022 by Caleb Chan, MD
(Updated: 2/1/2026)
Click here to contact Caleb Chan, MD
Tachyarrhythmias in the setting of high-dose vasopressors due to septic shock are not uncommon. Aside from amiodarone, some providers may not know of alternative therapeutic options in the setting of septic shock. In addition, some may view the use of a beta-blocker as counter-intuitive or counter-productive in the setting of norepinephrine usage.
However, there have been multiple smaller studies evaluating using esmolol (and other short-acting beta-blockers) in the setting of tachycardia, septic shock and pressors. Outcomes regarding the theoretical benefits of beta-blockade in sepsis (i.e. decreased mortality/morbidity 2/2 decreased sympathetic innervation, inflammation, myocardial demand etc.) have been varied. However, esmolol has been demonstrated multiple times to be effective at reducing heart rate without significant adverse outcomes (i.e. no sig diff in mortality, refractory shock, or time on vasopressors).
Caveats/pitfalls
-most of the studies discuss “adequate resuscitation” prior to initiation of esmolol
-not studied in patients that also had significant cardiac dysfunction
-be aware that esmolol gtts can be a lot of volume and pts can become volume overloaded if boarding in the ED for an extended period of time
Cocchi MN, Dargin J, Chase M, et al. Esmolol to treat the hemodynamic effects of septic shock: a randomized controlled trial. Shock. 2022;57(4):508-517.
Morelli A, Ertmer C, Westphal M, et al. Effect of heart rate control with esmolol on hemodynamic and clinical outcomes in patients with septic shock: a randomized clinical trial. JAMA. 2013;310(16):1683.
Rehberg S, Joannidis M, Whitehouse T, Morelli A. Landiolol for managing atrial fibrillation in intensive care. European Heart Journal Supplements. 2018;20(suppl_A):A15-A18.
Zhang J, Chen C, Liu Y, Yang Y, Yang X, Yang J. Benefits of esmolol in adults with sepsis and septic shock: An updated meta-analysis of randomized controlled trials. Medicine. 2022;101(27):e29820.
Category: Pediatrics
Keywords: trauma informed care, pediatric resuscitation (PubMed Search)
Posted: 7/15/2022 by Jenny Guyther, MD
(Updated: 2/1/2026)
Click here to contact Jenny Guyther, MD
Beaulieu-Jones BR, Bingham S, Rhynhart KK, Croitoru DP, Singleton MN, Rutman MS, Baertschiger RM. Incorporating a Trauma-Informed Care Protocol Into Pediatric Trauma Evaluation: The Pediatric PAUSE Does Not Delay Imaging or Disposition. Pediatr Emerg Care. 2022 Jan 1;38(1):e52-e58. doi: 10.1097/PEC.0000000000002278. PMID: 33181796.
Category: Critical Care Literature Update
Keywords: balanced crystalloid, saline, resuscitation, kidney injury (PubMed Search)
Posted: 7/14/2022 by William Teeter, MD
Click here to contact William Teeter, MD
Balanced crystalloids: So Hot Right Now
Brief Read:
The use of balanced crystalloids has been the subject of several RCTs with conflicting results. However, recent post-hoc and meta-analyses of these same trials suggest that balanced crystalloids may be the best choice initially. See nice summary at: https://www.atsjournals.org/doi/full/10.1164/rccm.202203-0611ED.
Long Read:
While I had thought about summarizing the recently published data on EPR from the CRITICAL trial in Japan, JournalFeed today covered the recent post-hoc analysis of the BaSICS trial originally seen on CC Pearls back in August 31, 2021 by Dr. Sjelocha. This subject is as important as it is confusing. There are large and relatively well done RCTs that point in opposite and sometimes strange directions. However, as the authors of the SMART trial summarized, even an NNT of 94 in this population could be a huge number of patients!
The use of balanced crystalloids (e.g. Plasmalyte) has been the subject of several previous RCTs (SMART and SALT-ED) with conflicting results. Recently the PLUS RCT and BaSICS trials seemed to push the literature towards to concluding there was no difference, but there are caveats for both trials now in the literature:
This paper makes a nice point which I think is important for us in the ED: the evidence is suggesting a commonality in many critical care concepts, which is that decisions made in early resuscitation may have an outsized impact on patient outcomes. However, this will not be the last we hear on this subject, but for the time being, I agree with Dr. Lacy that “It might not matter as much what fluids you choose when patients are on their third, fourth, or fifth liter of fluid – but especially for the sickest patients, it sure seems like the initial resuscitation fluid makes a difference.”
BaSICS post hoc: https://www.atsjournals.org/doi/full/10.1164/rccm.202111-2484OC (See JournalFeed post from today and the accompanying editorial)
BASICS: https://jamanetwork.com/journals/jama/fullarticle/2783039 (summary stolen from Dr. Sjeklocha’s August 31, 2022 CC Pearl)
PLUS: https://www.nejm.org/doi/10.1056/NEJMoa2114464
SMART: https://www.nejm.org/doi/full/10.1056/nejmoa1711584
SALT-ED: https://www.nejm.org/doi/full/10.1056/nejmoa1711586
https://journalfeed.org/article-a-day/2022/back-to-basics-first-fluid-choice-matters-a-reanalysis-of-the-basics-rct/
Category: Orthopedics
Keywords: Hand nodules, contractures (PubMed Search)
Posted: 7/9/2022 by Brian Corwell, MD
Click here to contact Brian Corwell, MD

Dupuytren disease/contracture: nodular thickening and resultant contraction of the palmer fascia.
Increased in those of Northern European discent
Increased risk over age 50
Increased frequency in those with diabetes and cigarette smoking
One or more painful nodules located near the distal palmer crease.
Over a variable amount of time, the nodule progresses to form a taught fibrous cord
This extends from the palm to the digits, generally ulnar sided and typically the ring finger
Can cause flexion contracture of digit at MCP joint
Sensation is normal.
No imaging necessary
Tx: padded gloves and activity modification for mild disease, steroid injection for moderate disease and surgery when contracture present
Category: Pharmacology & Therapeutics
Keywords: insulin, hyperkalemia, hypoglycemia (PubMed Search)
Posted: 7/4/2022 by Ashley Martinelli
Click here to contact Ashley Martinelli
Prior studies have found that patients are at an increased risk for hypoglycemia when administered insulin for the acute management of hyperkalemia when they have renal dysfunction. A new single-center, retrospective study investigated the risk of hypoglycemia and the overall effect of potassium lowering in patients with renal dysfunction and stratified outcomes based on the CKD level.
Patients were included if they were ordered insulin for hyperkalemia using a hospital driven order set and had CKD stages 3a, 3b, and 4. They were excluded if they had dialysis within 6h of insulin administration, had DKA, or no repeat labs. The hospital order set encourages 5 units of insulin instead of 10 when “renal failure” is present without clear guidance.
377 patients were included: 186 received 5 units and 191 received 10 units. The average age was 65 years old, predominantly male, weighing 90 kg. In the 5 unit group, significantly more patients had CKD stage 4 (60% v 30%) and in the 10 unit group, significantly more patients were CKD stage 3a (p<0.001). The baseline serum potassium was 6 in each group.
The hypoglycemia incidence was not different between groups, with severe hypoglycemia occurring twice per group. All patients received dextrose according to the protocol.
There was a significant difference in the reduction of serum potassium between the 5 and 10 unit groups: -0.63 mmol/L vs -0.9 mmol/L (p 0.001).
Bottom line: Hypoglycemia occurred even with insulin dose reduction. Potassium lowering was higher in patients who received the 10 unit dose.
Finder SN, McLaughlin LB, Dillon RC. 5 versus 10 units of intravenous insulin for hyperkalemia in patients with moderate renal dysfunction.
Category: Pediatrics
Keywords: pediatric trauma, ultrasound, FAST (PubMed Search)
Posted: 7/1/2022 by Rachel Wiltjer, DO
(Updated: 2/1/2026)
Click here to contact Rachel Wiltjer, DO
Bottom line: A positive FAST warrants further workup and may be helpful in the hemodynamically unstable pediatric trauma patient, but a negative FAST does not exclude intraabdominal injury and evidence for performing FAST in hemodynamically stable pediatric patients is limited.
Guyther, J. Advances in Pediatric Abdominal Trauma: What’s New is Assessment and Management. Trauma Reports 2016; 17: 1-15.
Holmes JF, Kelley KM, Wootton-Gorges SL, Utter GH, Abramson LP, Rose JS, Tancredi DJ, Kuppermann N. Effect of Abdominal Ultrasound on Clinical Care, Outcomes, and Resource Use Among Children With Blunt Torso Trauma: A Randomized Clinical Trial. JAMA. 2017 Jun 13;317(22):2290-2296.
Category: Critical Care
Keywords: Insulin infusion, diabetes mellitus, diabetic ketoacidosis, DKA, subcutaneous, long-acting (PubMed Search)
Posted: 6/29/2022 by Kami Windsor, MD
(Updated: 9/21/2022)
Click here to contact Kami Windsor, MD
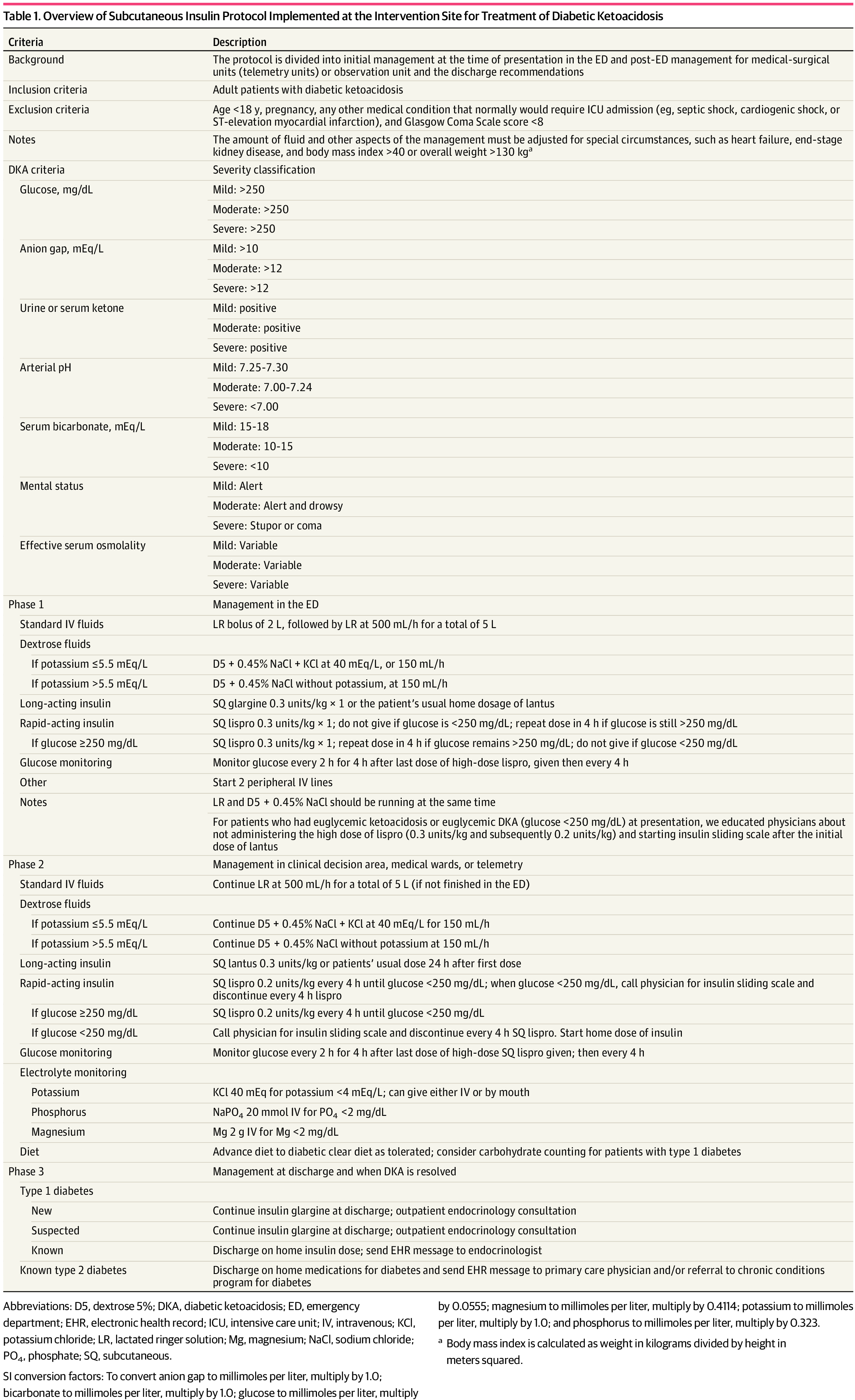
Background: It is classically taught that the tenets of DKA management are IV fluids, electrolyte repletion, and an insulin infusion that is titrated until approximately 2 hours after anion gap closure, when long-acting subcutaneous insulin is administered if the patient is tolerating oral intake. It has been previously found that earlier administration of subcutaneous long-acting insulin can shorten the time to anion gap closure, while other small studies have noted similar efficacy in subcutaneous insulin compared to IV in mild/moderate DKA.
A recent JAMA article presents a retrospective evaluation of a prospectively-implemented DKA protocol (see "Full In-Depth" section) utilizing weight-based subcutaneous glargine and lispro, rather than IV regular insulin, as part of initial and ongoing floor-level inpatient treatment.
When compared to the period before the DKA protocol:
The only exclusion criteria were age <18 years, pregnancy, and presence of other condition that required ICU admission.
Bottom Line: Not all DKA requires IV insulin infusion.
At the very least, we should probably be utilizing early appropriate-dose subcutaneous long-acting insulin. With ongoing ICU bed shortages and the importance of decreasing unnecessary resource use and hospital costs, perhaps we should also be incorporating subcutaneous insulin protocols in our hospitals as well.
As a part of the DKA protocol, patients:
Elevated BMI was not included in exclusion criteria, however the authors note that their DKA protocol has been amended to exclude patients >166kg due to concerns regarding insulin absorption.
Rao P, Jiang S, Kipnis P, et al. Evaluation of Outcomes Following Hospital-Wide Implementation of a Subcutaneous Insulin Protocol for Diabetic Ketoacidosis. JAMA Netw Open. 2022;5(4):e226417. doi:10.1001/jamanetworkopen.2022.6417
Houshyar J, Bahrami A, Aliasgarzadeh A. Effectiveness of Insulin Glargine on Recovery of Patients with Diabetic Ketoacidosis: A Randomized Controlled Trial. J Clin Diagn Res. 2015 May;9(5):OC01-5. doi: 10.7860/JCDR/2015/12005.5883.
Mohamed A, Ploetz J, Hamarshi MS. Evaluation of Early Administration of Insulin Glargine in the Acute Management of Diabetic Ketoacidosis. Curr Diabetes Rev. 2021;17(8):e030221191986. doi: 10.2174/1573399817666210303095633.
Karoli R, Fatima J, Salman T, Sandhu S, Shankar R. Managing diabetic ketoacidosis in non-intensive care unit setting: Role of insulin analogs. Indian J Pharmacol. 2011 Jul;43(4):398-401. doi: 10.4103/0253-7613.83109.
Ersöz HO, Ukinc K, Köse M, Erem C, Gunduz A, Hacihasanoglu AB, Karti SS. Subcutaneous lispro and intravenous regular insulin treatments are equally effective and safe for the treatment of mild and moderate diabetic ketoacidosis in adult patients. Int J Clin Pract. 2006 Apr;60(4):429-33. doi: 10.1111/j.1368-5031.2006.00786.x.
Category: Orthopedics
Keywords: Radial nerve compression, peripheral nerve injury, wrist drop (PubMed Search)
Posted: 6/25/2022 by Brian Corwell, MD
(Updated: 2/1/2026)
Click here to contact Brian Corwell, MD
The radial nerve is susceptible to compressive neuropathy against the spiral grove of the humerus which can lead to neuropraxia.
When the upper arm is compressed against a chair back or bar edge sometimes from a lost battle with alcohol: Saturday night palsy.
When another individual sleeps on someone’s arm overnight compressing the radial nerve: Honeymoon palsy
From nerve compression from improper technique with crutches: Crutch palsy
If diagnosis not clear from history, DDx includes other entities that can also present with isolated wrist, thumb/finger drop
Horses: Radial verve palsy, CVA, C7 compression
Zebras: Lead toxicity, acute porphyrias (often polyneuropathy but upper extremity before lower and frequently distal extensors
Careful history and exam important in differentiating
In cases of peripheral compression against the spital groove the triceps maintains strength.
The distal extensors lose strength (wrist and fingers)
Including the thumb abduction (abductor pollicis longus is radial-innervated)
AND so will the brachioradialis
The brachioradialis (despite being a forearm flexor) has dual innervation from the radial nerve in 80% of people.
Brachioradialis strength is often preserved in a central lesion.
Best tested with arm supported on a surface in mid pronation/supination (hammer curl position) and have patient flex against resistance and evaluate muscle strength and bulk.
Category: Critical Care
Keywords: Vasopressors, Hypotension, Shock, Sepsis (PubMed Search)
Posted: 6/21/2022 by Mark Sutherland, MD
(Updated: 2/1/2026)
Click here to contact Mark Sutherland, MD
Although it is well-documented that there is no true "maximum" dose of vasopressor medications, further blood pressure support as doses escalate to very high levels tends to be limited. As such, debate has raged in Critical Care as to when is the "right" time to start a second vasoactive medication. The VASST trial (Russell et al, NEJM, 2008) is considered to be the landmark trial in this area, and found a trend towards improvement with early addition of vasopressin to norepinephrine, but no statistically significant difference, and may have been underpowered.
Partly as a result of VASST, the pendulum has tended to swing towards maximizing a single vasoactive before adding a second over the past decade. The relatively high cost of vasopressin in the US has also driven this for many institutions. However, more recently a "multi-modal" approach, emphasizing an earlier move to second, or even third, vasoactive medication, is increasingly popular. Although cost is often prohibitive for angiotensin-2 given controversial benefits, many now advocate for targeting adrenergic receptors (e.g. with norepinephrine or epinephrine), vasopressin receptors (e.g. with vasopressin or terlipressin) and the RAAS system (e.g. with angiotensin 2) simultaneously in patients with refractory shock. A recent review by Wieruszewski and Khanna in Critical Care (see references) outlines this approach well.
Bottom Line: When to add a second vasoactive medication (e.g. vasopressin) for patients with refractory shock after a first vasoactive is controversial and not known. Current practice is trending towards earlier addition of a second (or third) agent, especially if targeting different receptors, but there is limited high-quality evidence to support this approach. Many practicioners (including this author) still follow VASST and consider vasopressin once doses of around 5-15 micrograms/min (non-weight based) of norepinephrine are reached.
Wieruszewski PM, Khanna AK. Vasopressor Choice and Timing in Vasodilatory Shock. Crit Care. 2022 Mar 22;26(1):76. doi: 10.1186/s13054-022-03911-7. PMID: 35337346; PMCID: PMC8957156.
Russell JA, Walley KR, Singer J, Gordon AC, Hébert PC, Cooper DJ, Holmes CL, Mehta S, Granton JT, Storms MM, Cook DJ, Presneill JJ, Ayers D; VASST Investigators. Vasopressin versus norepinephrine infusion in patients with septic shock. N Engl J Med. 2008 Feb 28;358(9):877-87. doi: 10.1056/NEJMoa067373. PMID: 18305265.
Early addition of Terlipressin: Article Title (ijccm.org)
Category: Pediatrics
Keywords: PNA, pediatrics, duration of treatment (PubMed Search)
Posted: 6/17/2022 by Jenny Guyther, MD
(Updated: 2/1/2026)
Click here to contact Jenny Guyther, MD
Williams DJ, Creech CB, Walter EB, Martin JM, Gerber JS, Newland JG, Howard L, Hofto ME, Staat MA, Oler RE, Tuyishimire B, Conrad TM, Lee MS, Ghazaryan V, Pettigrew MM, Fowler VG Jr, Chambers HF, Zaoutis TE, Evans S, Huskins WC; The DMID 14-0079 Study Team. Short- vs Standard-Course Outpatient Antibiotic Therapy for Community-Acquired Pneumonia in Children: The SCOUT-CAP Randomized Clinical Trial. JAMA Pediatr. 2022 Mar 1;176(3):253-261. doi: 10.1001/jamapediatrics.2021.
Category: Critical Care
Posted: 6/14/2022 by Mike Winters, MBA, MD
Click here to contact Mike Winters, MBA, MD
Vasopressor Tips in the Critically Ill
Legrand M, et al. Ten tips to optimize vasopressor use in the critically ill patient. Intensive Care Med. 2022; online ahead of print.
