Category: EMS
Keywords: CPR, pediatric, T-CPR, dispatch, public safety (PubMed Search)
Posted: 2/18/2026 by Jenny Guyther, MD
Click here to contact Jenny Guyther, MD
Bottom line: Education to the public is needed to help to improve the information relayed to telecommunicators in an emergency. Further telecommunicator education can help to overcome the barriers within their control, such as the recognition of agonal breathing.
An important step in the chain of survival in cardiac arrest is recognition of an emergency. When a person calls 911, the telecommunicator needs to be able to obtain the necessary information to direct the right resource to the right patient and be able to deliver directions for CPR if required.
This study looked at 911 calls for pediatric patients who were in cardiac arrest on EMS arrival in Denmark over a 3 year period and identified 3 barriers to the recognition of the arrest by the telecommunicator.
Prolonged conversations focused on the cause of the child's condition as opposed to assessmening consciousness and breathing.
Assessing breathing when the patient has irregular or agonal breaths
Callers who were unable to communicate or follow instructions from the telecommunicator.
Kragh AR, Kjærholm SH, de Claville Holland Flarup L, Juul Grabmayr A, Borch-Johnsen L, Folke F, Tjørnhøj-Thomsen T, Hassager C, Malta Hansen C. Barriers for Responding to Pediatric Out-of-Hospital Cardiac Arrest During Emergency Medical Calls: A Qualitative Study. J Am Heart Assoc. 2025 Jan 7;14(1):e035636. doi: 10.1161/JAHA.124.035636. Epub 2024 Dec 18. PMID: 39692033; PMCID: PMC12054490.
Category: Critical Care
Keywords: Sodium, ICP, neurocritical care, sodium bicarbonate, bicarb, hyperosmolar (PubMed Search)
Posted: 2/17/2026 by Zachary Wynne, MD
Click here to contact Zachary Wynne, MD
Bottom Line: Hypertonic sodium bicarbonate (8.4%) can be used judiciously as an alternative hyperosmolar therapy in the setting of increased intracranial pressure (ICP) or cerebral edema with impending herniation, particularly in setting of concomitant metabolic acidosis. Two 50 mL ampules of hypertonic sodium bicarbonate is the equivalent of approximately 200 mL of 3% sodium chloride (hypertonic saline).
Scenario:
The CT scan on your patient presenting with altered mental status shows a large intraparenchymal hemorrhage with 8 mm of midline shift. Suddenly, the patient becomes bradycardic with irregular respirations. Examination shows aniscoria with a non reactive right pupil. You call for 3% sodium chloride (hypertonic saline) and mannitol but neither will arrive from pharmacy for the next 10 minutes. What can you do in the meantime?
Background:
Sodium bicarbonate (commonly known as baking soda, NaHCO3) is a salt that acts as a weak base when dissolved in water. Clinically, it comes in two forms: hypertonic sodium bicarbonate (8.4% in 50 mL ampules) and isotonic sodium bicarbonate (1.3%, made with 3 ampules of hypertonic bicarbonate in one liter of D5 water).
Hyperosmolar therapy is often used to temporize patients in the setting of cerebral edema/increased ICP with concern for herniation syndrome (Cushing triad, aniscoria with non reactive pupil, posturing). This therapy will temporize patients for CT imaging and definitive management. Usual choices include 3% hypertonic saline or mannitol. The administration of these agents increases intravascular osmolality and theoretically causes solute drag to pull water out of organs, such as the brain, decreasing edema.
Hypertonic sodium bicarbonate can also function in this manner. To compare osmolality:
Hypertonic sodium bicarbonate can be given by two 50 mL ampules given in rapid succession in the setting of elevated ICP. This is the osmotic equivalent to giving approximately 200 mL of 3% hypertonic saline. Hypertonic sodium bicarbonate is often found in code carts in the emergency department and can sometimes be easier to access quickly in case of an acute clinical change like our above scenario. Hypertonic sodium bicarbonate can also be considered in patients that have received multiple rounds of hypertonic saline and thus have developed a hyperchloremic metabolic acidosis. There is limited data from the Neurocritical Care literature that has shown decreased ICP in the setting of TBI with hypertonic sodium bicarbonate administration (references below).
Hypertonic sodium bicarbonate side effects include metabolic alkalosis which can be detrimental in the patient with elevated ICP; normocapnea/normocarbia is critical to maintain cerebral blood flow and excess sodium bicarbonate administration should be avoided in patients that already have a metabolic alkalosis. Additionally, the metabolic alkalosis from sodium bicarbonate can also precipitate hypocalcemia if a patient is at risk. Additionally, hypertonic sodium bicarbonate can also cause some irritation to peripheral veins.
References:
Category: Ultrasound
Keywords: POCUS, trauma, optic ultrasound (PubMed Search)
Posted: 2/16/2026 by Alexis Salerno Rubeling, MD
(Updated: 2/18/2026)
Click here to contact Alexis Salerno Rubeling, MD
Bottom Line: Left Optic Disc Elevation was found to be an independent predictor of mortality and need for surgical intervention for patients with head trauma.
A recent study aimed to compare the diagnostic and prognostic performance of optic nerve sheath diameter (ONSD) and optic disc elevation (ODE) in patients with head trauma.
A total of 257 patients were included; 51.4% were hospitalized, 12.5% required surgical intervention, and 8.2% experienced in?hospital mortality.
Left ODE was identified as an independent predictor of mortality, with an adjusted hazard ratio (HR) of 4.25 (95% CI, 1.48–12.1; p = 0.007). (Left ODE 1.3 mm with IQR of 0.7 in mortality group). It also demonstrated improved diagnostic performance for predicting the need for surgical intervention.
To measure ODE:
Measure the distance between the anterior peak of the optic disc and its junction with the posterior scleral surface.
To measure ONSD:
Measure 3 mm posterior to the papilla, placing calipers on the outer borders of the hyperechoic rim surrounding the optic nerve sheath.
Ahmet S, Nazire BA, Ramazan K. The test characteristics of ONSD and ODE tests in predicting the prognosis of patients with traumatic brain injury. AJEM in press 2026 doi: doi.org/10.1016/j.ajem.2026.02.015
Category: Trauma
Keywords: aajt, tourniquet (PubMed Search)
Posted: 2/4/2026 by Robert Flint, MD
(Updated: 2/14/2026)
Click here to contact Robert Flint, MD
A case report on use of the abdominal aortic and junctional tourniquet in a 27 year old female with hemorrhagic shock secondary to a pelvic fracture after a 10 meter fall demonstrated improved blood pressure and stabilized vasopressor use prior to operative intervention. This device has been used in battlefield situations, however very few reports of civilian use exist. Much more data is needed, however, it is a device to be aware of for future use.
From the manufacture's website:
"The AAJTS is an Abdominal Aortic Junctional Tourniquet that is designed to stop non-compressible hemorrhages wherever they occur on the body. FDA Certified for abdominal, axilla, inguinal and pelvic fractures, the AAJTS is battlefield tested and proven to be quick, easy, and effective to deploy.

1. Honnef, G., Freidorfer, D., Puchwein, P. et al. Bleeding control in catastrophic blunt pelvic trauma using the abdominal aortic and junctional tourniquet in a civilian level I trauma center: A case report. Scand J Trauma Resusc Emerg Med 34, 2 (2026). https://doi.org/10.1186/s13049-025-01517-w
2.https://www.life-assist.com/products/details/2848/abdominal-aortic-junctional-tourniquet/
Category: Orthopedics
Keywords: arthrocentesis, septic arthritis (PubMed Search)
Posted: 2/14/2026 by Brian Corwell, MD
Click here to contact Brian Corwell, MD
BOTTOM LINE: Modify WBC threshold for diagnosing septic arthritis is patients who received recent antibiotics (24h to 2 weeks).
The ISDA 2024 guidelines use a WBC synovial fluid count of greater than 50,000 cells/mm to suggest septic arthritis.
A study of 81 patients with culture proven septic arthritis found the average leukocyte count was 40,408 ± 29,433 cells/µL in those who received antibiotics prior to arthrocentesis vs 93,824 ± 73,875 cells/µL in those who received no antibiotics for two weeks prior.
This is a greater than 50% reduction in mean WBC count!
A retrospective study of 383 patients found that patients who received IV or oral abx within 2 weeks before arthrocentesis had an optimal synovial WBC cutoff of > 16,000 (sensitivity 82%, specificity 76%), compared to >33,000 cells/µL (sensitivity 96%, specificity 95%) in the control group who had not received antibiotics within 2 weeks.
Conclusion:
When a patient has received antibiotics before arthrocentesis, a diagnostic value of >16,000 synovial leukocytes may be considered to guide treatment of septic arthritis. Additionally, in this one study, a diagnostic value of >33,000 synovial WBCs yields the highest accuracy for diagnosis of septic arthritis in patients who have not been given antibiotics before arthrocentesis.
Massey PA, et al. Optimal Synovial Fluid Leukocyte Count Cutoff for Diagnosing Native Joint Septic Arthritis After Antibiotics: A Receiver Operating Characteristic Analysis of Accuracy. The Journal of the American Academy of Orthopaedic Surgeons. 2021.
Category: Pediatrics
Keywords: Pediatrics, vomiting, ondansetron, emesis (PubMed Search)
Posted: 2/13/2026 by Kathleen Stephanos, MD
(Updated: 2/18/2026)
Click here to contact Kathleen Stephanos, MD
BOTTOM LINE: It is generally safe and effective to discharge vomiting pediatric patients with a prescription for ondansetron, and a recent study supported this common practice.
While it has become common practice to prescribe ondansetron to children with emesis, a 2025 randomized controlled study showed that a prescription for ondansetron decreased the risk of moderate to severe gastroenteritis in the following 7 days.
This study compared children 6 months to 18 years of age who received either ondansetron or placebo. They found a rates of moderate to severe gastroenteritis to be 5.1% in the ondansetron group versus 12.5% in the placebo group.
*Note that ondansetron is NOT approved for children under 6 months of age or in those with prolonged QT.
Freedman SB, Williamson-Urquhart S, Plint AC, Dixon A, Beer D, Joubert G, Pechlivanoglou P, Finkelstein Y, Heath A, Zhang JZ, Wallace A, Offringa M, Klassen TP; Pediatric Emergency Research Canada Innovative Clinical Trials Study Group. Multidose Ondansetron after Emergency Visits in Children with Gastroenteritis. N Engl J Med. 2025 Jul 17;393(3):255-266. doi: 10.1056/NEJMoa2503596. PMID: 40673584.
Category: Pharmacology & Therapeutics
Keywords: Andexxa, andexanet alfa, withdrawn, Kcentra, 4F-PCC (PubMed Search)
Posted: 2/11/2026 by Wesley Oliver
(Updated: 2/12/2026)
Click here to contact Wesley Oliver
Take Home Point: Andexxa (andexanet alfa) was voluntarily withdrawn from the US market effective December 22, 2025, due to safety concerns. 4-Factor Prothrombin Complex Concentrate (4F-PCC/Kcentra) remains the standard of care for reversing apixaban and rivaroxaban in life-threatening bleeding.
Why was it pulled? AstraZeneca, in consultation with the FDA, discontinued the manufacturing and sale of Andexxa after the ANNEXA-I post-marketing trial showed that the drug's risks outweigh its benefits. The trial compared Andexxa to usual care (primarily 4F-PCC) in intracranial hemorrhage and found a significant safety signal:
Clinical Action Items:
------------------------------------------------------------------------------------------------------------
Institutional Note: You may recall that our institution (like many others) never added Andexxa to the formulary. We cited the lack of high-quality survival data and cost-benefit concerns as our primary reasoning. Consequently, this market withdrawal requires no change to our local practice. We will continue to use 4F-PCC as our standard for Factor Xa inhibitor reversal, a practice now validated by the FDA's safety findings.
FDA Safety Communication: Update on the Safety of Andexxa by AstraZeneca. December 18, 2025. Link
Category: Critical Care
Posted: 2/10/2026 by Mike Winters, MBA, MD
Click here to contact Mike Winters, MBA, MD
Diagnostic Errors in the Critically Ill
Valentin A, et al. Exploring the dark side of the moon: diagnostic errors in critically ill patients. Intensive Care Med. 2025; 51:2422-5.
Category: Obstetrics & Gynecology
Posted: 2/9/2026 by Jennifer Wang, MD
Click here to contact Jennifer Wang, MD
Well, it depends on who you ask - ACOG defines it as greater or equal to 1000ml of blood loss within that first 24 hours, but most research articles define it as greater or equal to 500ml, while they define severe postpartum hemorrhage as greater or equal to 1000ml. But what is it actually?
The World Health Organization decided to tackle this question to look at what level of blood loss is the most clinically relevant in a meta-analysis from last year. They reviewed 12 different databases and over 300000 patients to look at levels of blood loss and when that was associated with mortality/severe morbidity. They found that the standard 500ml cutoff was actually only around 75% sensitive, but when they dropped those levels to 300/400/450, they lost a lot of specificity. So, what they did is they came up with their own rules and re-evaluated them based on their data to see how sensitive and specific they were.
What they found with a sensitivity of 87% and a specificity of 66-76% was:
Consider someone as having CLINICALLY SIGNIFICANT blood loss if they had EITHER:
OR
So look at the vitals + the blood loss together, and use those to guide your clinical actions!
Gallos I, Williams CR, Price MJ, et al. Prognostic accuracy of clinical markers of postpartum bleeding in predicting maternal mortality or severe morbidity: a WHO individual participant data meta-analysis. Lancet. 2025;406(10514):1969-1982. doi:10.1016/S0140-6736(25)01639-3
Category: Vascular
Keywords: popliteal artery injury review (PubMed Search)
Posted: 2/4/2026 by Robert Flint, MD
(Updated: 2/8/2026)
Click here to contact Robert Flint, MD
Popliteal artery injuries are very rare (4% of all vascular injuries).
The majority of injuries are secondary to penetrating injury (70+%)
Blunt mechanism of injury has the higher rate of amputation.
Prolonged ischemia time (from injury to repair greater than 6 hours) leads to higher rates of amputation
Hard signs of vascular injury should prompt X-ray imaging of the knee, femur, and lower extremity and transfer to an operating room for repair.
Soft signs ("a history of significant bleeding which has ceased, nonexpanding hematomas, and the presence of an Ankle-Brachial Index of less than 0.9") and shotgun injury should prompt CT angiogram to evaluate arterial injury.
Asensio, Juan A. MD, PhD, DABS, FACS, FCCM, FRCS (England), FSVS, FAIM, FISS, KM; Ceron, Santiago A. MD; Inyang, Ime D. BA; Johnson, Sarah E. DHSc, MS; Williams, Mallory MD, MPH, FACS, FICS, FCCP, FCCM; Velasco, Jose M. MD, FACS, FCCM. Popliteal artery injuries: What you need to know. Journal of Trauma and Acute Care Surgery 100(2):p 162-172, February 2026. | DOI: 10.1097/TA.0000000000004752
Category: Trauma
Keywords: ICh, risk factor head injury, geriatric (PubMed Search)
Posted: 2/4/2026 by Robert Flint, MD
(Updated: 2/7/2026)
Click here to contact Robert Flint, MD
In a metanalysis of studies looking at intercranial hemorrhage in fall patients older than 65 years, the following were unadjusted odds ratio risk factors for finding an ICH in this patient population:
suspected open or depressed skull fracture , signs of basal skull fracture ), reduced baseline Glasgow Coma Scale score , focal neurologic signs , seizure , vomiting , amnesia , loss of consciousness , headache ), external sign of head trauma , male sex , chronic kidney disease , preinjury single antiplatelet , and dual antiplatelet medication .
Preinjury anticoagulant was not a significant risk factor.
When looking at adjusted odds rations only focal neurologic signs , external sign of head trauma , loss of consciousness , and male sex were found to be associated with intercranial hemorrhage.
Dubucs, Xavier et al.
Annals of Emergency Medicine, Volume 87, Issue 2, 181 - 191
Category: Toxicology
Keywords: medetomadine, withdrawal (PubMed Search)
Posted: 2/4/2026 by Robert Flint, MD
(Updated: 2/5/2026)
Click here to contact Robert Flint, MD
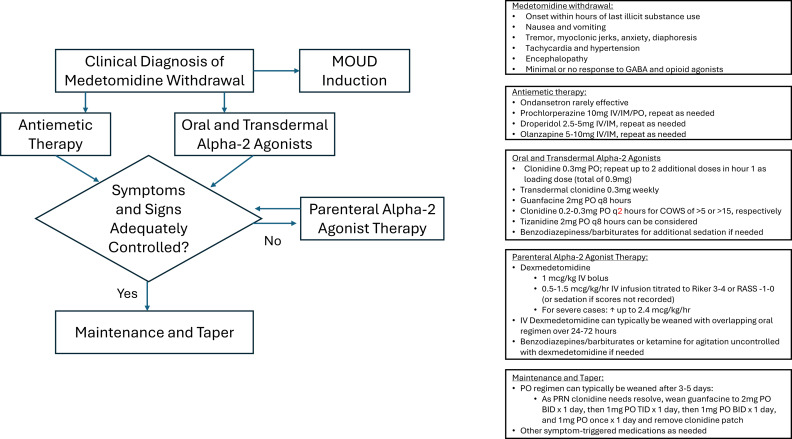
The US drug supply has been found to contain medetomidine as an adulterant to heroine/fentanyl. It is a potent tranquilizer used in animals. It is an alpha 2 blocker (similar pharmacology to clonidine and xylazine). Exposure to this drug can induce withdrawal symptoms to include anxiety, tremor, diaphoresis, nausea, vomiting, agitation, sympathetic hyperactivity, and delirium. Withdrawal can start within 4-6 hours of last use.
Treatment for withdrawal is outlined in this diagram.
Category: Toxicology
Keywords: toxins, misperceived for edible, food containers (PubMed Search)
Posted: 2/4/2026 by Kathy Prybys, MD
Click here to contact Kathy Prybys, MD

Poisonings due to storage in a secondary container reported to the National Poison Data System, 2007–2017. Carpenter J., Murray B. et al., Clinical Toxicology, 2021.59(6), 521–527.
Poisoning following exposure to chemicals stored in mislabelled or unlabelled containers: a recipe for potential disaster. Millard YC, Slaughter RL, et al. New Zealand Med J. 26 September 2014, Vol 127 No 1403.
Unintentional poisoning from decanted toxic household chemicals. Von Fabeck K, Boulamery A, et al. Clin Toxicol (Phila). 2023 Mar;61(3):186-189.
Antifreeze on a freezing morning: ethylene glycol poisoning in a 2-year-old. Hann G, Duncan D, et al. BMJ Case Rep. 2012 Mar
Epidemiology of Accidental Poisoning Caused by Storage of Non-Food Substances in Food Containers and unmarked Bottles/Containers. Geller RJ, Kezirian R, Bangar P, Strong D, Carlson T. Children’s Hospital Central California; California Poison Control System (CPCS). https://www.tandfonline.com/doi/pdf/10.1080/15563650903076924
Category: Critical Care
Posted: 2/2/2026 by Jessica Downing, MD
(Updated: 2/18/2026)
Click here to contact Jessica Downing, MD
Etomidate is often a go-to agent for RSI because it is considered relatively hemodynamically neutral. However, lab studies have shown an association with transient adrenal suppression, and some observational studies and meta-analyses have suggested that patients intubated with etomidate face higher risk of cardiovascular collapse and in-hospital mortality than those intubated with ketamine.
The RSI trial was a pragmatic open-label multi-center randomized control trial conducted in 6 EDs and 8 ICUs across the US and compared induction with ketamine 1-2mg/kg versus etomidate 0.2-0.3mg/kg for RSI of critically ill adults (excluding trauma patients). They found no significant difference in overall 28 day hospital mortality across the cohort. They found an increased risk of cardiovascular collapse during intubation in the ketamine group. This increased risk was more pronounced in patients with sepsis or septic shock and patients with APACHE II ?20.
Some details:
Overall - this was a well conducted randomized control trial that - at the very least - suggests that etomidate is likely as safe (if not safer) than ketamine with respect to 28d mortality and peri-intubation cardiovascular collapse, even among patients with critical illness or septic shock.
Casey JD, Seitz KP, Driver BE, Gibbs KW, Ginde AA, Trent SA, Russell DW, Muhs AL, Prekker ME, Gaillard JP, Resnick-Ault D, Stewart LJ, Whitson MR, DeMasi SC, Robinson AE, Palakshappa JA, Aggarwal NR, Brainard JC, Douin DJ, Marvi TK, Scott BK, Alber SM, Lyle C, Gandotra S, Van Schaik GW, Lacy AJ, Sherlin KC, Erickson HL, Cain JM, Redman B, Beach LL, Gould B, McIntosh J, Lewis AA, Lloyd BD, Israel TL, Imhoff B, Wang L, Spicer AB, Churpek MM, Rice TW, Self WH, Han JH, Semler MW; RSI Investigators and the Pragmatic Critical Care Research Group. Ketamine or Etomidate for Tracheal Intubation of Critically Ill Adults. N Engl J Med. 2025 Dec 9:10.1056/NEJMoa2511420. doi: 10.1056/NEJMoa2511420. Epub ahead of print. PMID: 41369227; PMCID: PMC12711137.
Category: Ultrasound
Keywords: POCUS, resident education, ultrasound guided nerve blocks (PubMed Search)
Posted: 2/1/2026 by Alexis Salerno Rubeling, MD
(Updated: 2/2/2026)
Click here to contact Alexis Salerno Rubeling, MD
Ultrasound Guided Nerve Blocks (UGNBs) provides targeted analgesia that can effectively alleviate pain from injuries or painful procedures while reducing opioid use.
In 2021, ACEP issued a policy statement affirming that ultrasound-guided regional anesthesia is within the scope of EM physicians and is a core component of multimodal pain management pathways in the ED. However, EM residencies have not uniformly defined nerve block requirements, resulting in a wide range of graduating resident skill levels. Recent ACGME updates may help standardize expectations and address this gap.
A recent review of the National Ultrasound-Guided Nerve Block Registry (NURVE) looked at the impact of operator training level on the analgesic effectiveness of ED-performed UGNBs. The most commonly performed block among attendings was the erector spinae block, while for residents it was the fascia iliaca block. Both resident and attending performed blocks showed a reduction in pain but there was an 80.7% meaningful pain reduction in attendings as compared to 63.4% for residents. Out of the 1595 nerve block cases reviewed there were only 2 complications which included transient episode of LAST and respiratory difficulty from suspected diaphragmatic hemiparesis.
These findings highlight the importance of experience while supporting the safety and effectiveness of UGNBs performed by supervised residents in the training environment.
Macias M, Driver L, Riscinti M, Dreyfuss A, et al. Training level and analgesic outcomes of ultrasound-guided nerve blocks in the emergency department: An analysis from the NURVE block registry, The American Journal of Emergency Medicine, 2026 doi.org/10.1016/j.ajem.2026.01.050.
Category: Trauma
Keywords: Hypothermia, fall, height, injury (PubMed Search)
Posted: 1/31/2026 by Robert Flint, MD
(Updated: 2/1/2026)
Click here to contact Robert Flint, MD
An English study describes 30 patients that jumped from a single bridge of 30 meters (98 feet) over the course of 12 years. Twenty six landed in the water. The injury pattern for those landing in water was described as “Hypothermia was the most common presentation (n = 23), followed by pneumothoraces (n = 14), rib fractures (n = 10), thoracic vertebral fractures (n = 9) and lung contusions (n = 8). Lower water temperatures at the time of the incident (p = 0.008) and lower patient body temperatures on arrival to hospital (p = 0.002) were significantly associated with increased 30-day mortality.”
The small group landing on land had more pelvic and extremity fractures than the water group and none had hypothermia.
Remember to start aggressive rewarming in patients who fall into water!
Harvey T, Nottingham T, Owen P, Hannah J, Plumb J. Injury patterns and clinical outcomes following falls from a medium-height bridge: A retrospective study. Trauma. 2025;28(1):44-53. doi:10.1177/14604086251404739
Category: Trauma
Keywords: Stab wound, chest radiograph, pneumothorax (PubMed Search)
Posted: 1/31/2026 by Robert Flint, MD
(Updated: 2/18/2026)
Click here to contact Robert Flint, MD
This small study from South Africa shows stab wounds to the chest with a pneumothorax less than 0.5 cm that were managed conservatively had completely resolved on 12 hour repeat chest X-ray. This could facilitate earlier discharge of these patients. It also supports conservative (non-tube placement) approach to asymptomatic small pneumothoraces from stab wounds.
Kong V, Cheung C, Lee D, et al. Defining the optimal timing of interval chest radiograph in conservatively managed small pneumothorax from thoracic stab wounds – a South African experience. Trauma. 2025;28(1):14-17. doi:10.1177/14604086251396434
Category: Geriatrics
Keywords: Tramadol, geriatrics (PubMed Search)
Posted: 1/29/2026 by Robert Flint, MD
(Updated: 2/18/2026)
Click here to contact Robert Flint, MD
Tramadol has been viewed as a safer alternative for pain control than opioids. This study says differently.
“Tramadol use was associated with increased risk of multiple ER utilizations, falls/fractures, CVD hospitalizations, safety event hospitalizations, and mortality (new users only) compared to nonuse.”
Musich S, Wang SS, Schaeffer JA, Slindee L, Kraemer S, Yeh CS. Safety Events Associated with Tramadol Use Among Older Adults with Osteoarthritis. Popul Health Manag. 2021 Feb;24(1):122-132. doi: 10.1089/pop.2019.0220. Epub 2020
Category: Administration
Keywords: Communication, Teamwork (PubMed Search)
Posted: 1/28/2026 by Mercedes Torres, MD
Click here to contact Mercedes Torres, MD
How well does your ED care team communicate? For some high yield strategies and reasons for improvement, read on…
To explore effective and ineffective communication in the ED and its impact of patient care, physician and nurses from several academic EDs completed an online anonymous survey, then attended focus group sessions. Responses highlighted the following themes:
1: Situations, built physical environment, and medium of communications all impact quality of communication.
2: Core elements of desired professional communication include respect, closed-loop communication, and attention, often conveyed through non-verbal behaviors.
3: Poor communication begets poor communication in later interactions
4: Effective communication is seen as fundamental to patient care but also has impacts beyond patient care
5: Clinician gender and gender dyads influence communication dynamics, age and experience dyads did not.
Do any of these themes resonate with you? What can you do within your department to improve physician-nurse communication and the care you provide?
Jones DC, Phillips J, Graveson A, et al. Emergency Physician and Emergency Nurse Communication in the Emergency Department: A Mixed-methods Study. West J Emerg Med. 2026;27(1)91–98.
Category: Critical Care
Keywords: OCHA, VF, ventricular fibrillation, cardiac arrest, shockable, Occult VF (PubMed Search)
Posted: 1/28/2026 by Kami Windsor, MD
(Updated: 2/18/2026)
Click here to contact Kami Windsor, MD
A crucial part of cardiac arrest management is identification of the underlying rhythm, with key aspects of management diverging depending whether shockable (pulseless ventricular tachycardia/pVT or ventricular fibrillation/VF) or unshockable (pulseless electrical activity/PEA or asystole).
A recent study prospectively evaluated adult atraumatic out-of-hospital-cardiac-arrests (OHCAs) presenting to the ED, to determine what percentage of cases had “Occult VF” – VF found point-of-care echocardiogram but not by ECG. The researchers only included cases with simultaneous ECG and echo assessments for the initial 3 pulse checks. Echo and ECG determinations for the study were adjudicated by research team members.
They found that:
Major limitations:
Bottom Line: Point-of-care echocardiogram continues to have value in the management of cardiac arrest, potentially changing management and affecting post-ROSC decisions. Ensuring high-quality CPR, with appropriate defibrillation and anti-arrhythmic strategies, remains paramount in management of shockable OHCA.
Gaspari R, Adhikari S, Gleeson T, et al. Occult Ventricular Fibrillation Visualized by Echocardiogram During Cardiac Arrest: A Retrospective Observational Study From the Real-Time Evaluation and Assessment for Sonography-Outcomes Network (REASON). J Am Coll Emerg Physicians Open. 2025;6(1):100028. doi: 10.1016/j.acepjo.2024.100028.
