Category: Orthopedics
Keywords: Steroids, Sciatica (PubMed Search)
Posted: 6/20/2015 by Michael Bond, MD
Click here to contact Michael Bond, MD
Steroid Use in the treatment of Acute Sciatica
Have you used oral steroids in the treatment of your patient with acute sciatica thought to be secondary to a herniated disk.
Well a recent randomizaed, double-blind, placebo-controlled trial from 2008 to 2013 in a large integrated health care system in Northern California enrolled 269 patients to look at whether steroids improved pain or function. The intervention arm (twice as large as placebo arm) received a tapering 15-day course of oral prednisone (5 days each of 60 mg, 40 mg, and 20 mg; total cumulative dose = 600 mg; n = 181).
In the end there were no differences in surgery rates at 52-week follow-up, and the steroid arm had a modest improvement in function but no improvement in pain. There were also more adverse events at 3-week follow-up in the prednisone group than in the placebo group.
Conclusion: Giving steroids for acute sciatica does not appear to improve the patients pain, only has a modest improvement in function, and was associated with more adverse events. Put another way there was minimal benefit and more harm.
You can check out the full article at http://jama.jamanetwork.com/article.aspx?doi=10.1001/jama.2015.4468
Goldberg H, Firtch W, Tyburski M, Pressman A, Ackerson L, Hamilton L, Smith W, Carver R, Maratukulam A, Won LA, Carragee E, Avins AL. Oral steroids for acute radiculopathy due to a herniated lumbar disk: a randomized clinical trial. JAMA. 2015 May 19;313(19):1915-23. doi: 10.1001/jama.2015.4468.
Category: Pediatrics
Keywords: migraine, sodium valproate, headache (PubMed Search)
Posted: 6/19/2015 by Jenny Guyther, MD
Click here to contact Jenny Guyther, MD
Sodium valproate (VPA) had been studied and found to be effective in the adult population for migraines, but not in the pediatric population. This article was a small (12 patient) retrospective study of pediatric migraine patients looking at pain scores before and after VPA administration. Prior to VPA, patients received NSAIDs, dopamine antagonists, IV fluids and narcotics. Mean pain reduction prior to VPA was 17%. After VPA, pain scores were reduced by an additional 36%.
Sheridan, D, Sun, B, O’Brien, BS, and Hansen, M. Intravenous Sodium Valproate for Acute Pediatric Headache. The Journal of Emergency Medicine. Article in Press. Accepted February 2015.
Category: Toxicology
Keywords: Synthetic cannabinoid, K2 (PubMed Search)
Posted: 6/18/2015 by Hong Kim, MD
(Updated: 2/2/2026)
Click here to contact Hong Kim, MD
Recently, there has been a surge in synthetic cannabinoid in the U.S., including the Baltimore area. According to U.S. poison control center data, there has been 229% increase in calls related to SC between January to May of 2015 compared to similar time period in 2014.
The most commonly reported adverse/clinical effects included:
End-organ injuries have been also reported in case reports, including AKI, seizure, MI, and CVA.
Synthetic cannabinoid includes a list of chemical compounds that are structurally different compared to THC – the active compound in marijuana. However, they possess full CB1 (cannabinoid) receptor agonism effect, unlike the THC, which is a partial CB1 receptor agonist.
These chemicals (particularly JWH series) were originally synthesized to study the effect of cannabinoid receptors. Overall, it is difficult to identify the compound and the dose within each packets of SC.
Commonly marketed names include: Spice, K2, K9, herbal highs, Scooby snax, WTF.
Table. Identified synthetic cannabinoids
| Chemical name | Chemical origin |
| JWH-018; JWH-073; JWH-250 | Laboratory of J.W. Huffman |
| CP47,497; CP47,497-C8; CP59,540; cannabicyclohexanol | Pfizer laboratory |
| HU-210 | Hebrew University laboratory |
| Oleamide | Fatty acid |
| UR-144 | CB2 receptor agonist |
| XLR-11, AKB-48, AM-2201, AM-694 |
|
Management: Majority of the patients with acute SC intoxication mostly requires supportive care, including benzodiazepine for acute agitation. However, ED providers should be mindful of potential end-organ injury.
Law R et al. Increase in reported adverse health effects related to synthetic cannabinoid use - United States, January - May 2015. MMWR 2015;64:618-619.
Weaver et al Designer drugs 2015: assessment and management. Addic Sci Clin Pract. 2015 Mar 25;10:8. doi: 10.1186/s13722-015-0024-7.
Takematsu M et al. A case of acute cerebral ischemia following inhalation of a synthetic cannabinoid. Clin Toxicol (Phila) 2014;59:973-975.
Buser GL et al. Acute kidney injury associated with smoking synthetic cannabinoid. Clin Toxicol 2014;52:664-73.
Category: International EM
Keywords: parasites, infectious diseases (PubMed Search)
Posted: 6/17/2015 by Jon Mark Hirshon, MPH, MD, PhD
(Updated: 2/2/2026)
Click here to contact Jon Mark Hirshon, MPH, MD, PhD
While most infections from parasites are associated with poor communities in low-income countries, there are still some important parasitic infections found in the United States.
The U.S. Centers for Disease Control and Prevention (CDC) has identified 5 parasitic diseases as priorities for public health action based upon:
These are
Bottom line:
Remember to keep your differential broad and maintain awareness of these generally unusual but important infections.
http://www.cdc.gov/parasites/npi/
Category: Critical Care
Keywords: Shock, hemodynamics, RIAD, Renal interlobar artery doppler, Resistive Index (PubMed Search)
Posted: 6/16/2015 by John Greenwood, MD
Click here to contact John Greenwood, MD
Renal Resuscitation using Renal Interlobar Artery Doppler (RIAD)
Shocked patient…. check! Adequate volume resuscitation…. check! Vasopressors.… check! Mean arterial pressure (MAP) > 65 mmHg….. check! Adequate urine output…. Wait, why isn’t my patient making urine?
As we begin to understand more about shock, hemodynamics, and the importance of perfusion over the usual macrocirculatory goals (MAP > 65), finding ways to assess regional blood flow is critical. A recent study examined the effect of fluid administration on renal perfusion using renal interlobar artery Doppler (RIAD) to assess the interlobar resistive index (RI). See how to perform a RIAD here.
They also recorded the fluid challenge’s effect on the traditional hemodynamic measurements of MAP and pulse pressure (PP) then observed the patient’s urine output (as a clinical marker of perfusion). The authors reported 3 key findings:
Bottom Line: The use of ultrasound to determine intrarenal hemodynamics is an interesting strategy to guide renal resuscitation in the shocked patient. There is mixed data on the use of RIAD, however this study could explain the findings of SEPSISPAM and also addresses the growing concern that traditional hemodynamic goals may be inadequate resuscitation targets.
References
For more critical care & resuscitation pearls, follow me on Twitter @JohnGreenwoodMD
Category: Visual Diagnosis
Posted: 6/15/2015 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
Patient presents with headache and papilledema. What's the diagnosis?
Hydrocephalus secondary to malfunctioning VP shunt.
The patient went to the operating room for a shunt repair and the CT after the repair is shown; although not dramatically different it does show an improvement of the hydrocephalus.
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Orthopedics
Keywords: Posterolateral Corner Injury, PCL, ACL, knee (PubMed Search)
Posted: 6/13/2015 by Brian Corwell, MD
Click here to contact Brian Corwell, MD
Hx: hyperextension injury (contact and non contact), varus directed blow to flexed knee, direct blow to anteriomedial knee. Report instability symptoms when knee is in full extension.
PE: Varus stress testing
Varus laxity at 0 indicate LCL and cruciate ligament (ACL/PCL) injury
Varus laxity at 30 indicates LCL injury
Dial test - inspects the external rotation at the knee joint/performed in both 30 and 90 knee flexion. The dial test inspects the external rotation at the knee joint
https://www.youtube.com/watch?v=pW4yv0zg4RY
Positive at 30 = > 10 external rotation asymmetry = isolated PCL injury
Positive at 30 & 90 = Posterior lateral corner injury and PCL injury
Category: Pediatrics
Posted: 6/12/2015 by Rose Chasm, MD
(Updated: 2/2/2026)
Click here to contact Rose Chasm, MD
Therapeutic Hypothermia after Out-of-Hospital Cardiac Arrest in Children. Mosler FW, et al. N Eng J Med 2015; 372:1898-1908. May 2015
Category: Toxicology
Keywords: aspirin, extracorporeal, salicylate, poisoning (PubMed Search)
Posted: 5/22/2015 by Bryan Hayes, PharmD
(Updated: 6/11/2015)
Click here to contact Bryan Hayes, PharmD
The Extracorporeal Treatments in Poisoning (EXTRIP) Workgroup has published their latest review, this time on extracorporeal treatment for salicylate poisoning. Here are their recommendations on when to dialyze:
Juurlink DN, et al. Extracorporeal Treatment for Salicylate Poisoning: Systematic Review and Recommendations From the EXTRIP Workgroup. Ann Emerg Med. 2015 May 8. [Epub ahead of print, PMID 25986310]
Follow me on Twitter (@PharmERToxGuy) or Google Plus (+bryanhayes13)
Category: Neurology
Keywords: Guidelines, intracerebral hemorrhage, ICH score, communication (PubMed Search)
Posted: 6/10/2015 by WanTsu Wendy Chang, MD
(Updated: 10/14/2015)
Click here to contact WanTsu Wendy Chang, MD
What is the ICH Score?
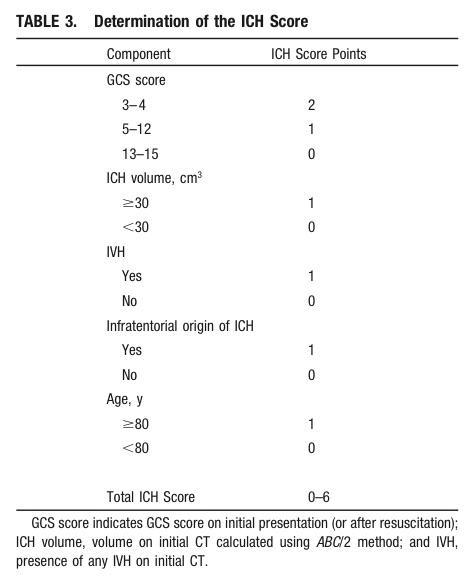
Take Home Point: Communicate the severity of your ICH patient by using either the composite ICH Score or by including details such as the patient's GCS, estimated volume of ICH, presence of IVH, and supra- vs. infratentorial origin.
1) Hemphill JC 3rd, Greenberg SM, Anderson CS, Becker K, Bendok BR, Cushman M, et al. Guidelines for the management of spontaneous intracerebral hemorrhage: A guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2015 May 28. [Epub ahead of print]
2) Hemphill JC 3rd, Bonovich DC, Besmertis L, Manley GT, Johnston SC. The ICH Score: A simple, reliable grading scale for intracerebral hemorrhage. Stroke. 2001;32(4):891-897.
Follow me on Twitter @EM_NCC
Category: Critical Care
Posted: 6/9/2015 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
Intraosseous (IO) placement is a rapid and reliable method for obtaining venous access in critically ill patients; previous studies demonstrated that everything from vasopressors to packed RBCs can be infused through it.
This prospective observational study compared the first-pass success rate and time to successful placement of IO versus landmark-based (i.e., not ultrasound guided) central-line placement (femoral or subclavian access) during medical emergencies (e.g., cardiac arrest) in an inpatient population.
The first pass success rate for IO was found to be significantly higher than the landmark technique (90% vs. 38%) and placement was significantly faster for IOs (1.2 vs. 10.7 minutes).
Despite the fact that this study did not directly compare IO to ultrasound guided line placement, this study demonstrates that IO is a rapid and effective means to obtain central access during patients with emergent medical conditions.
Bottom-line: Consider placing an IO line when rapid central access is necessary.
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Visual Diagnosis
Posted: 6/8/2015 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
The following clip is one of three findings found in Beck’s triad. Name all three findings and how often are all 3 signs present for patients with pericardial tamponade?

Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Pharmacology & Therapeutics
Keywords: obese, vancomycin, loading dose (PubMed Search)
Posted: 5/22/2015 by Bryan Hayes, PharmD
(Updated: 6/6/2015)
Click here to contact Bryan Hayes, PharmD
Vancomycin guidelines recommend an initial dose of 15-20 mg/kg based on actual body weight (25-30 mg/kg in critically ill patients). [1] The MRSA guidelines further recommend a max dose of 2 gm. [2]
But, what dose do you give for an obese patient that would require more than 2 gm?
A new study provides some answers to this question. [3] Obese-specific, divided-load dosing achieved trough concentrations of 10 to 20 g/mL for 89% of obese patients within 12 hours of initial dosing and 97% of obese patients within 24 hours of initial dosing.
Application to Clinical Practice
Caveats
The study used some more specific dosing calculations based on renal function and percentage above IBW. If patient's renal function is abnormal, consultation with a pharmacist is recommended.
Follow me on Twitter (@PharmERToxGuy) or Google Plus (+bryanhayes13)
Category: Toxicology
Posted: 6/5/2015 by Kishan Kapadia, DO
Click here to contact Kishan Kapadia, DO
Electronic cigarettes are battery-powered devices that deliver nicotine, flavorings, (e.g. fruit, mint, and chocolate), and other chemicals via an inhaled aerosol. E-cigarettes are currently not regulated by the FDA. In many states, there are no restrictions on the sale of e-cigarettes to minors.
Electronic cigarette exposures involving young children are rapidly increasing. Such exposures tend to involve patients aged < 5 years and occur by ingestion of the nicotine-containing liquid. There is a potential for acute nicotine toxicity (nausea, vomiting, pallor, diaphoresis, tachycardia, hypertenstion initially). Respiratory muscle weakness with respiratory arrest is the most likely cause of death.
To date, the overwhelming majority of pediatric ingestions have not resulted in serious medical outcomes. The most commonly reported adverse events were nausea and vomiting.
However, in May of 2014, the first pediatric case of toxicity from ingestion of e-cigarette nicotine liquid was reported. A 10-month old ingested an unknown amount of e-liquid and developed vomiting, tachycardia, grunting respirations, and ataxia. The symptoms resolved by 6 hours after ingestion without specific treatment.
(1) The figure above shows the number of calls to poison centers for cigarette or e-cigarette exposures, by month, in the United States during September 2010 February 2014. E-cigarette exposure calls per month increased from one in September 2010 to 215 in February 2014.
(1) Chatham-Stephens K, Law R, Taylor E, et al. MMWR Morb Mortal Wkly Rep 2014;63:292-293.
(2) LoVecchio F, Zoph O. Incidence of electronic cigarette exposure in children skyrockets in Arizona. Am J Emerg Med, epub, 2/25/15.
(3) Bassett RA, Osterhoudt K, Brabazon T. Nicotine Poisoning in an Infant. N Engl J Med 2014;370:2249-2250.
Category: International EM
Keywords: diarrhea, pediatrics, infectious diseases, global health (PubMed Search)
Posted: 6/3/2015 by Jon Mark Hirshon, MPH, MD, PhD
Click here to contact Jon Mark Hirshon, MPH, MD, PhD
Introduction:
As noted in the previous pearl (May 20, 2015), globally diarrheal diseases are the second leading cause of death for children under five- killing approximately 760,000 annually. What can be done to prevent and treat diarrhea, especially among young children?
Prevention of diarrheal illness:
Treatment of diarrheal illness:
Bottom Line
Diarrheal diseases kill hundreds of thousands of children in developing countries each year. Appropriate prevention measures (clean water, improved sanitation) can markedly decrease the burden of disease. Appropriate treatment (ORS) can save lives for pennies.
http://www.who.int/mediacentre/factsheets/fs330/en/
http://www.cdc.gov/healthywater/global/diarrhea-burden.html
http://emedicine.medscape.com/article/906999-clinical#a0217
Category: Critical Care
Keywords: HFNC, high flow, vapotherm, nasal cannula, respiratory failure, non invasive ventilation (PubMed Search)
Posted: 6/2/2015 by Feras Khan, MD
Click here to contact Feras Khan, MD
High Flow Nasal Cannula (HFNC) in acute respiratory hypoxemia
The Trial:
Results:
Bottom line:
Consider using HFNC prior to or while deciding on intubation in patients with hypoxemic respiratory failure usually due to pneumonia
Category: Neurology
Keywords: lumbar puncture, LP, obesity (PubMed Search)
Posted: 5/27/2015 by Danya Khoujah, MBBS
Click here to contact Danya Khoujah, MBBS
We all dread performing lumbar punctures on the obese patient. The traditional standard length spinal needle (9 cm) is becoming increasingly inadequate in reaching the subdural space in our overweight society.
Abe et al developed a formula for selecting the proper needle length to reach the middle of the spinal canal from the skin using retrospective CT data from 178 patients.
Length of needle (cm) = 1+ 17 x Weight (kg)/ Height (cm)
Given the average height of the American woman (163 cm or 5’4’’) our standard length spinal needle will FAIL to reach the mid-thecal space if a woman weighs more than 170 lb (75 kg)!!!
Paul Blart Mall Cop, and King of Queens star Kevin James (5’8’’, 285 lb) would require a 13.7 cm spinal needle. This means even our long spinal needles (12.7 cm) would FAIL by 1 cm.
Note that this formula resulted in selection of needles too small (6%) and too long (31%) of the time. Abe’s linear correlation had an R value of 0.81, (p<.001)
Bottom-Line: Consider use of a long spinal needle (12.7 cm) or IR guided LP in overweight /obese patients and the above formula to guide your depth of insertion
Category: Critical Care
Posted: 5/26/2015 by Mike Winters, MBA, MD
Click here to contact Mike Winters, MBA, MD
Stress-Induced Cardiomyopathy
Boland TA, et al. Stress-induced cardiomyopathy. Crit Care Med 2015; 43:868-93.
Category: Visual Diagnosis
Posted: 5/25/2015 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
Do you need to get stuff out of the thorax (like fluid or air) and don't want to place a HUGE chest tube? Consider a pigtail catheter; don't know how to place one? Well check out this video and learn how.
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Cardiology
Posted: 5/24/2015 by Semhar Tewelde, MD
Click here to contact Semhar Tewelde, MD
Reperfusion Ventricular Fibrillation
Ventricular fibrillation during reperfusion in STEMI is an infrequent, but serious complication.
Among ~4000 with STEMI between 2007-2012, 71 (1.9%) had reperfusion Vfib.
Increased risk for reperfusion Vfib is associated with: history of MI, aspirin and b-blocker use, Vfib before PCI, left main CAD, inferior MI, symptom-to-balloon time <360 minutes, maximal ST-segment elevation in a single lead >300 μV, and sum of ST-segment deviations in all leads >1,500 μV.
The sum of ST-segment deviations in all leads >1500 μV was an independent predictor of reperfusion Vfib.
Demidova M, Carlson J , et al. Am J Cardiol 2015;115:417e422
