Category: Neurology
Keywords: acute ischemic stroke, magnesium, neuroprotectant, IMAGES, FAST-MAG (PubMed Search)
Posted: 2/12/2015 by WanTsu Wendy Chang, MD
Click here to contact WanTsu Wendy Chang, MD
Magnesium, another failed neuroprotectant?
Stroke is a leading cause of adult disability and the second leading cause of death worldwide. Currently available therapies for acute ischemic stroke are based on restoring perfusion to the ischemic penumbra. However, they are only moderately effective.
A series of pathological cascades leading to neuronal death are triggered in acute ischemia. Thus it may be logical to suggest that if one can interrupt the propagation of these cascades, perhaps part of the brain tissue can be protected and salvaged.
Magnesium has been shown in various animal models to have pluripotent neuroprotective properties. It is also widely available, simple to administer, and has a favorable risk profile. A prior study of magnesium in acute ischemic stroke (IMAGES) did not show a benefit when the agent was administered a median 7.4 hours after symptom onset. However, a subgroup of patients treated within 3 hours of symptom onset showed possible benefit.
The Field Administration of Stroke Therapy - Magnesium (FAST-MAG) trial, funded by the NIH, looked at magnesium administered within 2 hours after symptom onset on the degree of disability at 90 days after stroke as measured by the modified Rankin scale.
Magnesium was not found to have any benefit in functional outcome at 90 days.
This study was unique in several ways:
However, despite this study being very well executed, demonstrating the feasibility of conducting a phase 3 trial with targeted intervention within the hyperacute window, it is another neuroprotective agent that failed to translate from the laboratory bench to the clinical realm.
Potential explanations for the discrepancies between preclinical and clinical outcomes of neuroprotective agents thus far include discrepancies on outcome measures, functional assessments, pre-morbid conditions, therapeutic windows, and drug-dosing schedules between animal studies and clinical trials.
Take Home Point: Magnesium does not have any clear benefit in acute ischemic stroke at this time.
Muir KW, Lees KR, Ford I, et al. Magnesium for acute stroke (Intravenous Magnesium Efficacy in Stroke trial): a randomised controlled trial. Lancet. 2004;363(9407):439-445.
Saver JL, Starkman S, Eckstein M, et al. Prehospital use of magnesium as neuroprotection in acute stroke. N Engl J Med. 2015;372(6):528-536.
Cheng YD, Al-Khoury L, Zivin JA. Neuroprotection for ischemic stroke: two decades of success and failure. NeuroRx. 2004;1(1):36-45.
Follow me on Twitter @EM_NCC
Category: Critical Care
Keywords: VAP, chlorhexidine baths, subglottic suctioning (PubMed Search)
Posted: 2/10/2015 by Feras Khan, MD
Click here to contact Feras Khan, MD
Updates in preventative strategies in the ICU
Preventing Ventilator Associated Pneumonia (VAP)
The trial
Bottom Line
Daily bathing with chlorhexidine does not reduce health care associated infections
The trial
Bottom Line
Category: Pharmacology & Therapeutics
Keywords: vancomycin, loading dose (PubMed Search)
Posted: 1/26/2015 by Bryan Hayes, PharmD
(Updated: 2/7/2015)
Click here to contact Bryan Hayes, PharmD
We know vancomycin should be dosed based on weight rather than the default 1 gm dose so many patients receive. A past Academic Life in EM post explores the nuances of proper vancomycin dosing. But do higher loading doses in the ED actually lead to more therapeutic trough levels?
New Data
A new randomized trial compared ED patients receiving 30 mg/kg initial doses vs. 15 mg/kg. [1] There was a significantly greater proportion of patients reaching target trough levels of 15 mg/L at 12 hours among the patients who received a 30 mg/kg loading dose as compared with a traditional 15 mg/kg dose (34% vs 3%, P < 0.01). This study did not use a max dose of 2 gm. They included patients up to 120 kg who received 3.6 gm loading doses! Patients with creatinine clearance < 50 mL/min were excluded. There was no difference in incidence of nephrotoxicity between the groups.
Application to Clinical Practice
Follow me on Twitter (@PharmERToxGuy) or Google Plus (+bryanhayes13)
Category: Toxicology
Keywords: Drug Screens, Drug Intervals (PubMed Search)
Posted: 2/5/2015 by Kishan Kapadia, DO
Click here to contact Kishan Kapadia, DO
| Performance Characteristics of Common Drug Abuse Screening Immunoassays | ||
| Drug/Class | Detection Interval (***) | Comments |
| Amphetamines | 1-2 days (2-4 days) | Decongestants, ephedrine,l-methamphetamine, selegilene & bupropion metabolites may give False (+) results; MDA & MDMA are variably detected |
| Barbiturates | 2-4 days | Phenobarbital may be detected for up to 4 weeks |
| Benzodiazepines | 1-30 days | Benzos vary in reactivityand potency; False (+) results may be seen with oxaprozin |
| Cannabinoids | 1-3 days (>1 month) | Screening assays detect inactive and active cannabinoids; Confirmatory assays detects inactive metabolite THCA (tetrahydrocannabinoic acid) |
| Cocaine | 2 days (1 week) | Screening & confirmatory assays detect inactive metabolite BE (benzoylecgonine); False (+) results are unlikely |
| Opiates | 1-2 days; 2-4 days (<1 week) | Semisynthetic opiates derived from morphine show variable cross-reactivity; Fully synthetic opioids (e.g., fentanyl, meperidine, methadone, propoxyphene, tramadol) have minimal cross reactivity; Quinolone may cross-react |
| Methadone | 1-4 days | Doxylamine may cross-react |
| Phencyclidine | 4-7 days (>1 month) | Dextromethorphan, diphenhydramine, ketamine, & venlafaxine may cross react |
| Propoxyphene | 3-10 days | Duration of positivity depends on cross reactivity of metabolite norpropoxyphene |
(***)Values are after typical use; values in parentheses are after heavy or prolonged use.
Adapted from Goldfrank's Toxicologic Emergencies, 9th ed; Table 6-10.
Category: International EM
Keywords: Measles, international, pediatrics, vaccination, public health (PubMed Search)
Posted: 2/4/2015 by Jon Mark Hirshon, MPH, MD, PhD
Click here to contact Jon Mark Hirshon, MPH, MD, PhD
From January 1st to January 30th, 2015, 102 people from 14 states were reported to have measles. This one month total is greater than the annual number of U.S. cases from 2002 to 2012. Most of these cases are related to a large outbreak from a Californian amusement park. Measles can spread in communities without adequate vaccination (low herd immunity). The majority of the people in the US who get measles are unvaccinated. However, measles remains common in many parts of the world.
Bottom Line:
As noted in the recent ACEP Fact Sheet, “A very high index of suspicion for Rubeola is necessary especially among patients with an exposure history, travel to foreign or domestic areas where disease is present, and those without adequate immunization. Immediate isolation of these patients should be considered in the ED or other outpatient healthcare setting.”
Category: Critical Care
Posted: 2/3/2015 by Mike Winters, MBA, MD
Click here to contact Mike Winters, MBA, MD
Hypertensive Emergency Pearls
Monnet X, Marik PE. What's new with hypertensive crisis? Intensive Care Med 2015; 41:127-130.
Category: Visual Diagnosis
Posted: 2/2/2015 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
Patient presents with right shoulder pain following minor trauma. What's the diagnosis....and what's the Cunningham technique?
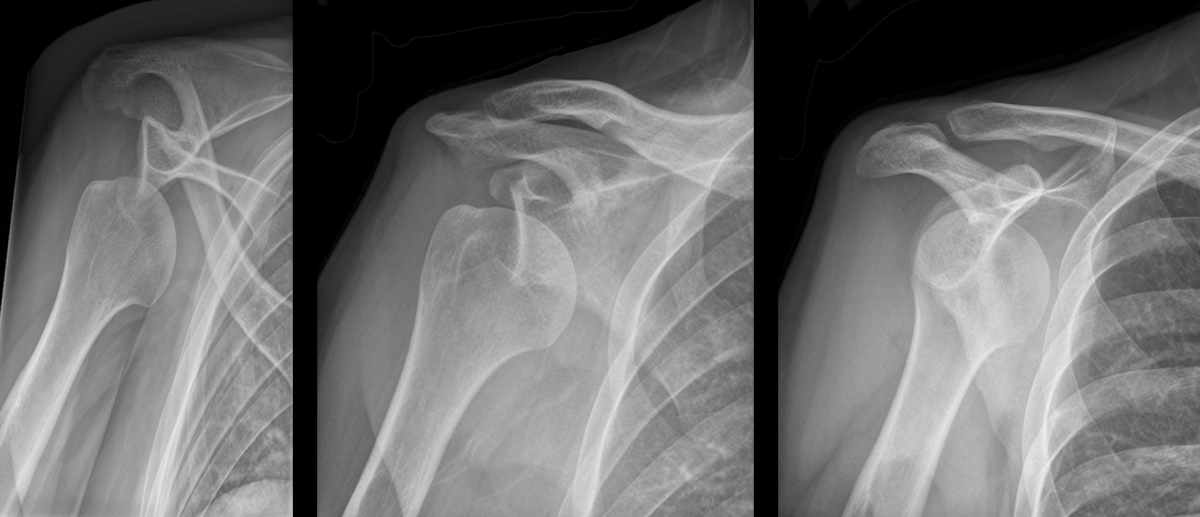
Anterior shoulder dislocation
Cunningham Technique
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Toxicology
Keywords: tetrodotoxin (PubMed Search)
Posted: 1/29/2015 by Fermin Barrueto
(Updated: 2/2/2026)
Click here to contact Fermin Barrueto
Tetrodotoxin is lethal poison that blocks sodium channels. A famous sushi called "Fugu" is cut from a puffer fish that contains this poison. The idea is to get just enough of the toxin to cause peri-oral paresthesia but not too much to get seizures, paralysis and cardiac dysrrhythmias. A recent outbreak in Minneapolis, Minnesota was just reported in the MMWR so it can really happen anywhere, its a great read - dried puffer was bought from a market in NYC.
http://www.cdc.gov/mmwr/preview/mmwrhtml/mm6351a2.htm
2-3 mg of the toxin is lethal to an adult human. No antidote exists though I would try hypertonic sodium bicarbonate for the cardiac dysrrhythmias and appropraite supportive. If the patient survives 24 hrs, the patient will do well without sequelae if appropriately supported.
Category: Neurology
Keywords: Myasthenia gravis, myopathy, iatrogenic (PubMed Search)
Posted: 1/29/2015 by Danya Khoujah, MBBS
Click here to contact Danya Khoujah, MBBS
Patients with myasthenia gravis (MG) may be seen in the emergency department for symptoms that are not related to their MG, such as an upper respiratory tract infection or chest pain, for example.
The emergency physician should be careful in prescribing new medications to patients with MG, as that can precipitate a myasthenic crisis (and therefore cause significant morbidity and mortality). Below is a list of medications that are commonly implicated; an extensive list can be found on www.myasthenia.org/docs/MGFA_medicationsandmg.pdf)
Sanders DB, Guptill JT. Myasthenia Gravis and Lambert-Eaton Myasthenic Syndrome. Continuum. 2014 Oct;20(5)
Category: Critical Care
Keywords: Methanol, toxicology, methanol toxicity, critical care (PubMed Search)
Posted: 1/20/2015 by John Greenwood, MD
(Updated: 1/30/2015)
Click here to contact John Greenwood, MD
Extracorporeal Treatment Strategies for Acute Methanol Poisoning (When to Dialyze)
Methanol toxicity is classically included in the differential for the intoxicated patient presenting to the ED. Add a negative EtOH level, anion/osmolar gap, blindness and you have yourself a slam dunk diagnosis. The goal is to stop the liver from metabolizing methanol to formic acid. Outside of fomepizole (or old school ethanol therapy), dialysis is often discussed, but when should you actually get the nephrologist on the phone?
This month the Extracorporeal Treatments in Poisoning Workgroup released a systematic review and consensus statement to help clinicians decide when to pull the HD trigger. Their suggestions are below.
When to start HD:
Which Modality: Intermittent HD (IHD) should be used over continuous renal replacement therapies (CRRT), as you can clear the toxin faster with higher HD flows.
When to stop HD: Extracorporeal treatment can be terminated when the methanol concentration is less than 200 mg/L or 6.2 mmol/L and a clinical improvement is observed.
Bottom Line: Consider early hemodialysis in most patients presenting with methanol toxicity. Clinical exam and routine lab testing will likely provide enough information to determine the need for IHD, but specific methanol levels can be helpful to guide adjunctive treatment options.
Reference
Roberts DM, Yates C, Megarbane B, et al. Recommendations for the Role of Extracorporeal Treatments in the Management of Acute Methanol Poisoning: A Systematic Review and Consensus Statement. Crit Care Med. 2015;43(2):461-472.
Follow me on Twitter @JohnGreenwoodMD
Category: Visual Diagnosis
Posted: 1/26/2015 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
Elderly male presents with the skin findings below. He is also on a medication for atrial fibrillation. What's the diagnosis?

Severe ecchymosis from coumadin overdose
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Cardiology
Posted: 1/26/2015 by Semhar Tewelde, MD
(Updated: 2/2/2026)
Click here to contact Semhar Tewelde, MD
Posterior Myocardial Infarctions (PMI)
- Posterior myocardial infarctions (PMI) are different than typical ST-elevation MI; the ECG findings include: septal & anterior ST-segment depression, dominant tall/broad R waves, and upright T waves.
- In a study among 117,739 subjects with STEMI, 824 with PMI were more likely to present with cardiac arrest, cardiogenic shock, and congestive heart failure.
- The median time from arrival ECG to revascularization with PCI was longer among subjects with PMI.
- The median time from arrival ECG to systemic thrombolysis was also longer among subjects with a PMI.
- Increased awareness and recognition of PMI is needed to improve reperfusion times among this subpopulation with STEMI.
Waldo S, et al. Reperfusion times and in-hospital outcomes among patients with an isolated posterior myocardial infarction. Am Heart J 2014;167:350-354.
Category: Orthopedics
Keywords: Heel pain, bone injury (PubMed Search)
Posted: 1/24/2015 by Brian Corwell, MD
Click here to contact Brian Corwell, MD
Overuse injury
Seen in runners, military recruits (marching), ballet dancers and in jumping sports (heavy landing).
Insidious onset of heel pain, that is worse with jumping then running then later with simple weight bearing.
Tenderness to palpation posteriorly (medially or laterally), and squeezing bilateral posterior calcaneus.
Testing:
XR: May not be positive for 2 to 4 weeks. Sclerotic appearance (vertically oriented) posterior calcaneus.
MRI: high signal T2 at fracture site.
DDx: plantar fasciitis.
Treatment: Reduction of activity if Sxs mild, for severe pain start a trial of non weight-bearing (boot or splint with crutches).
Stretching of calf, achilles, plantar fascia.
Category: International EM
Keywords: Tuberculosis, infectious disease, drug resistance, multidrug resistant tuberculosis (PubMed Search)
Posted: 1/21/2015 by Jon Mark Hirshon, MPH, MD, PhD
Click here to contact Jon Mark Hirshon, MPH, MD, PhD
As noted previously (UMEM Pearl of 1/7/2015), tuberculosis (TB) is a major infectious disease that occurs worldwide. Strains of tuberculosis can be resistant to one or more anti-tuberculosis medications. TB strains resistant to at least one medication have been found in all surveyed countries.
What is multidrug-resistant tuberculosis (MDR TB)?
Treatment of MDR TB
Bottom line:
As noted previously, in your emergency department have a high index of suspicion for TB and MDR TB in patients with an appropriate risk profile.
http://www.who.int/mediacentre/factsheets/fs104/en/
http://www.cdc.gov/tb/topic/drtb/default.htm
http://www.cdc.gov/tb/publications/factsheets/drtb/mdrtb.htm
Category: Critical Care
Posted: 1/20/2015 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Visual Diagnosis
Posted: 1/19/2015 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
60 year-old male presents with 6 months of weight loss,epistaxis, and increased headache when bending over. What's the diagnosis?
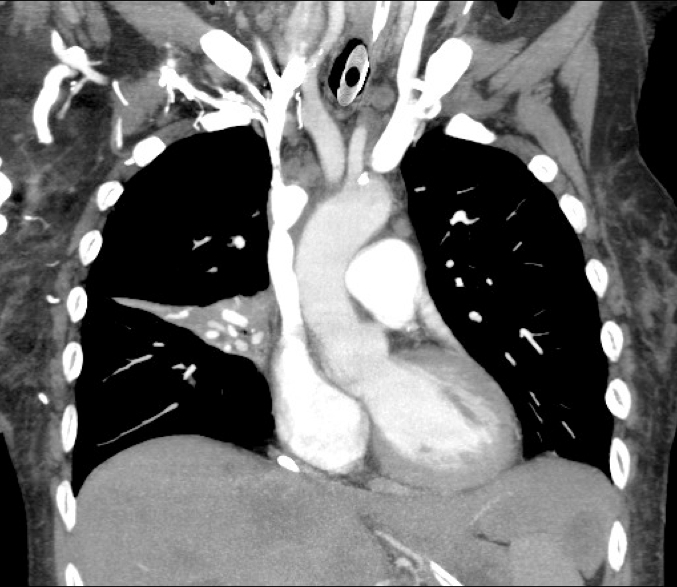
SVC Syndrome
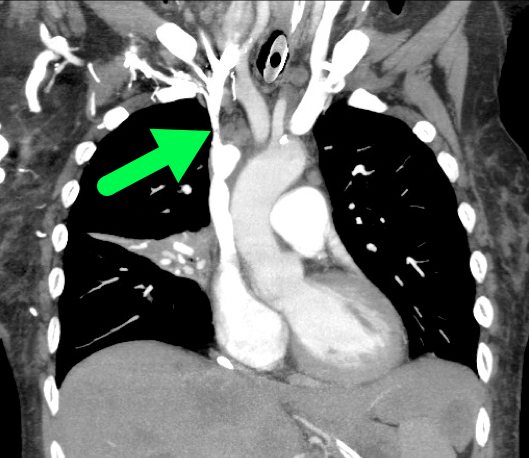
Rice TW, Rodriguez RM, Light RW. The superior vena cava syndrome: clinical characteristics and evolving etiology. Medicine (Baltimore). Jan 2006;85(1):37-42.
Nunnelee JD. Superior vena cava syndrome. J Vasc Nurs. Mar 2007;25(1):2-5
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Pediatrics
Keywords: Trauma, pelvic fractures, imaging (PubMed Search)
Posted: 1/19/2015 by Jenny Guyther, MD
Click here to contact Jenny Guyther, MD
Of pediatric patients who have anteroposterior (AP) pelvic xrays (XR), there is a 4.6% rate of pelvic fracture or dislocation, compared to 10% in adults.
This study is a sub analysis of a prospective observational cohort of children with blunt torso trauma conducted by PECARN. 7808 patients had pelvic imaging, with 65% of them having an AP XR. The XR sensitivity ranged from 64-82% (based on age groups) for detecting fractures. All but one patient with a pelvic fracture not detected on XR had a CT scan. The CT scan detected all but 2 fractures both of which were picked up later as healing fractures on repeat pelvic XR. Some of the patients who had a missed fracture on XR were hemodynamically unstable or wound up requiring operative intervention.
The authors support the following algorithm:
-With hemodynamically unstability children, obtain a pelvic XR
-For hemodynamically stable children when the physician is planning to get a CT, there is no indication for XR
Bottom line: Consider using AP pelvic radiographs in the hemodynamically stable patient with a high suspicion for fracture or dislocation who are not undergoing CT.
Kwok et al. Sensitivity of Plain Pelvis Radiography in Children with Blunt Torso Trauma. Annals of Emergency Medicine 2015; 65: 63-71.
Category: Cardiology
Posted: 1/18/2015 by Semhar Tewelde, MD
(Updated: 2/2/2026)
Click here to contact Semhar Tewelde, MD
Left Ventricular Hypertrophy & Arrhythmias: Any Association?
Associations between left ventricular hypertrophy (LVH) and both supraventricular (SVT)/ventricular arrhythmias (VT/VF) have previously been reported.
A recent review & meta-analysis of 10 studies (27,141 patients) revealed the following:
- Incidence of SVT was 11% with LVH compared to 1% without (p <0.001)
- LVH patients had 3.4-fold greater odds of developing SVT
- Incidence of VT/VF was 5.5% with LVH compared to 1.2% without (p <0.001)
- LVH patients has 2.8 greater odds of developing VT/VF
The reason for increased arrhythmogenicity in LVH is not clearly understood.
A consistently observed abnormality in LVH is non-uniform propagation of the action potential throughout the myocardium, which sets the stage for arrhythmias based on early or delayed afterdepolarizations.
Given the heterogeneity in this meta-analysis further research between LVH & sustained arrhythmias is needed to infer true causality.
Saurav C, Chirag B, et al. Meta-Analysis of Left Ventricular Hypertrophy and Sustained Arrhythmias. The American Journal of Cardiology. Volume 114, Issue 7, Pages 1049-1052 (1 October 2014).
Category: Orthopedics
Keywords: heel, pain, causes (PubMed Search)
Posted: 1/17/2015 by Michael Bond, MD
(Updated: 2/2/2026)
Click here to contact Michael Bond, MD
We often think of Plantar Fascitis as the cause of heel pain but there are a lot of other causes. Some of those include:
Category: Toxicology
Keywords: intraosseous, hydroxocobalamin, cyanide poisoning (PubMed Search)
Posted: 1/15/2015 by Hong Kim, MD
(Updated: 2/2/2026)
Click here to contact Hong Kim, MD
Hydroxocobalamin is an effective cyanide antidote when administered intravenously. Although intraosseous (IO) access is often used in critically ill patients with difficult or delayed IV access, the efficacy of IO administration has not been investigated until recently.
In a recent randomized animal study, acute cyanide toxicity was induced in two groups of swine where 150 mg/kg Hydroxocobalamin was administered via IV vs. IO. The survival rate, reversal of hypotension, and laboratory results were similar between the IV and IO group.
The finding of this study suggest that IO administration of Hydroxocobalamin is as efficacious as IV administration and its administration in acute cyanide toxicity should not be delayed due to lack of IV access when IO access is available.
Bebarta VS, Pitotti RL, Bondreau S and Tanen DA. Intraosseus versus intravenous infusion of hydroxocobalamin for the treatment of acute severe cyanide toxicity in a swine model. Academic Emergency Medicine. 2014; 21 (11): 1203-1211.
