Category: Toxicology
Keywords: take home naloxone, opioid overdose (PubMed Search)
Posted: 1/10/2019 by Hong Kim, MD
Click here to contact Hong Kim, MD
Take home naloxone (THN) programs have been expanded to help reduce the opioid overdose-related deaths. A study was done in Australia to characterize a cohort of heroin overdose deaths to examine if there was an opportunity for a bystander to intervene at the time of fatal overdose.
235 heroin-overdose deaths were investigated during a 2 year study period in Victoria, Australia.
Conclusion
Stam NC et al. Challenges with take-home naloxone in reducing heroin mortality: a review of fatal heroin overdose cases in Victoria, Australia. Clin Toxicol 2018 Nov 17:1-6. doi: 10.1080/15563650.2018.1529319. [Epub ahead of print]
Category: Neurology
Keywords: Intracerebral hemorrhage, ICH, volume, ABC/2 (PubMed Search)
Posted: 1/9/2019 by WanTsu Wendy Chang, MD
Click here to contact WanTsu Wendy Chang, MD
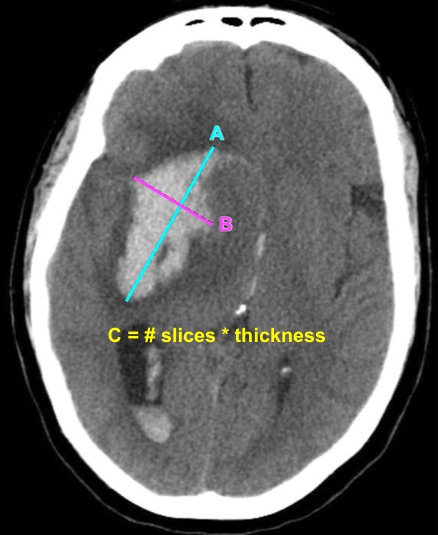
Bottom Line: EPs can reliably estimate ICH volume using the ABC/2 formula. Communicating ICH volume to neurosurgical and neurocritical care consultants can help direct treatment decisions.
Dsouza LB, Pathan SA, Bhutta ZA, et al. ABC/2 estimation in intracerebral hemorrhage: A comparison study between emergency radiologists and emergency physicians. Am J Emerg Med. 2018 Dec 19. [Epub ahead of print]
Follow me on Twitter @EM_NCC
Category: Critical Care
Posted: 1/8/2019 by Mike Winters, MBA, MD
(Updated: 2/2/2026)
Click here to contact Mike Winters, MBA, MD
Critically Ill Renal Transplant Patients
Darmon M, et al. Ten tips to manage renal transplant recipients. Intensive Care Med. 2019. epub ahead of print.
Category: Pharmacology & Therapeutics
Keywords: Flu, Treatment, Oseltamivir (PubMed Search)
Posted: 1/8/2019 by Wesley Oliver
(Updated: 2/2/2026)
Click here to contact Wesley Oliver
---Early antiviral treatment can shorten the duration of fever and illness symptoms, and may reduce the risk of some complications from influenza.
---Early treatment of hospitalized adult influenza patients with oseltamivir has been reported to reduce death in some observational studies.
---Clinical benefit is greatest when antiviral treatment is administered within 48 hours of influenza illness onset.
Antiviral treatment is recommended for patients with confirmed or suspected influenza who:
---are hospitalized;
---have severe, complicated, or progressive illness; or
---are at higher risk for influenza complications. (See below for in-depth information)
Oral oseltamivir is the recommended antiviral for patients with severe, complicated, or progressive illness who are not hospitalized, and for hospitalized influenza patients.
Treatment:
Doses: Oseltamivir 75 mg twice daily
Renal Impairment Dosing
CrCl >60 mL/minute: No dosage adjustment necessary
CrCl >30 to 60 mL/minute: 30 mg twice daily
CrCl >10 to 30 mL/minute: 30 mg once daily
ESRD undergoing dialysis: 30 mg immediately and then 30 mg after every hemodialysis session
Duration of Treatment:
Recommended duration for antiviral treatment is 5 days for oral oseltamivir. Longer daily dosing can be considered for patients who remain severely ill after 5 days of treatment.
People at higher risk for influenza complications recommended for antiviral treatment include:
---children younger than 2 years;
---adults 65 years and older;
---people with chronic pulmonary (including asthma), cardiovascular (except hypertension alone), renal, hepatic, hematological (including sickle cell disease), and metabolic disorders (including diabetes mellitus), or neurologic and neurodevelopment conditions (including disorders of the brain, spinal cord, peripheral nerve, and muscle, such as cerebral palsy, epilepsy [seizure disorders], stroke, intellectual disability, moderate to severe developmental delay, muscular dystrophy, or spinal cord injury);
---people with immunosuppression, including that caused by medications or by HIV infection;
---women who are pregnant or postpartum (within 2 weeks after delivery);
---people younger than 19 years old who are receiving long-term aspirin- or salicylate-containing medications
---American Indians/Alaska Natives;
---people who are extremely obese (i.e., body mass index is equal to or greater than 40); and
---residents of nursing homes and other chronic care facilities.
Centers for Disease Control and Prevention. Influenza antiviral medications: summary for clinicians. https://www.cdc.gov/flu/professionals/antivirals/summary-clinicians.htm (Accessed on January 8, 2019).
Category: Critical Care
Posted: 1/1/2019 by Mike Winters, MBA, MD
Click here to contact Mike Winters, MBA, MD
Dyspnea in the Intubated Patient
Decavele M, et al. Detection and management of dyspnea in mechanically ventilated patients. Curr Opin Crit Care. 2019; 25:86-94.
Category: Critical Care
Keywords: circulatory dysfunction, hypotension, shock, fluid resuscitation, IV fluids (PubMed Search)
Posted: 1/1/2019 by Kami Windsor, MD
Click here to contact Kami Windsor, MD
The European Society of Intensive Care Medicine (ESICM) recently released a review with recommendations from an expert panel for the use of IV fluids in the resuscitation of patients with acute circulatory dysfunction, especially in settings where invasive monitoring methods and ultrasound may not be available.
Points made by the panel include:
Recommendations from the panel include:
Bottom Line: Utilize all the information you have about your patient to determine whether or not they require IVF, and reevaluate their physical and biochemical (lactate) response to fluids to ensure appropriate IVF administration and avoid volume overload.
Cecconi M, Hernandez G, Dunser M, et al. Intensive Care Med. 2018. https://doi-org.proxy-hs.researchport.umd.edu/10.1007/s00134-018-5415-2
Category: Toxicology
Keywords: double-dose of single medication (PubMed Search)
Posted: 12/27/2018 by Hong Kim, MD
(Updated: 2/2/2026)
Click here to contact Hong Kim, MD
Taking a double-dose of a single medication is presumed to be safe in most cases. However, there is limited data to support this assumption.
A retrospective study of the California Poison Control System was performed to assess adverse effects of taking double dose of a single medication. During a 10-year period, 876 cases of double-dose ingestion of single medication were identified.
Adverse effects were rare (12 cases). However, medication classes that were involved in severe adverse effects included:
Conclusion:
Correia MS et al. A 10-year review of single medication double-dose ingestions in the nation's largest poison control system. Clin Toxicol 2018 Nov 28:1-5. doi: 10.1080/15563650.2018.1493205. [Epub ahead of print]
Category: Neurology
Keywords: headache, post concussion syndrome (PubMed Search)
Posted: 12/16/2018 by Brian Corwell, MD
(Updated: 12/23/2018)
Click here to contact Brian Corwell, MD
A previous pearl discussed medication-overuse headache (MOH).
MOH is also known as analgesic rebound headache, drug-induced headache or medication-misuse headache.
It is defined as headache… occurring on 15** or more days per month in a patient with a preexisting headache disorder who has been overusing one or more acute treatment drugs for headache with symptoms for three or more months.
The diagnosis is clinical, and requires a hx of chronic daily headache with analgesic use more than 2-3d per week.
The diagnosis of MOH is supported if headache frequency increases in response to increasing medication use, and/or improves when the overused medication is withdrawn.
The headache may improve transiently with analgesics and returns as the medication wears off. The clinical improvement after wash out is not rapid however, patients may undergo a period where their headaches will get worse. This period could last in the order of a few months in some cases.
The meds can be dc’d cold turkey or tapered depending on clinical scenario.
Greatest in middle aged persons. The prevalence rages from 1% to 2% with a 3:1 female to male ratio.
Migraine is the most common associated primary headache disorder.
** Each medication class has a specific threshold.
Triptans, ergot alkaloids, combination analgesics, or opioids on ten or more days per month constitute medication overuse.
Use of simple analgesics, including aspirin, acetaminophen and NSAIDS on 15 or more days per month constitutes medication overuse.
Caffeine intake of more than 200mg per day increases the risk of MOH.
Consider MOH in patients in the appropriate clinical scenario as sometimes doing less is more!
Category: Pediatrics
Keywords: Intubation, ETT, cuffed, airway management (PubMed Search)
Posted: 12/21/2018 by Jenny Guyther, MD
(Updated: 2/2/2026)
Click here to contact Jenny Guyther, MD
Historically uncuffed endotracheal tubes were used in children under the age of 8 years due to concerns for tracheal stenosis. Advances in medicine and monitoring capabilities have resulted in this thinking becoming obsolete. Research is being conducted that is showing the noninferiority of cuffed tubes compared to uncuffed tubes. Multiple other studies are looking into the advantages of cuffed tubes compared to uncuffed tubes.
The referenced study is a meta-analysis of 6 studies which compared cuffed to uncuffed endotracheal tubes in pediatrics. The pooled analysis showed that more patients needed tube changes when they initially had uncuffed tubes placed. There was no difference in intubation duration, reintubation occurrence, post extubation stridor, or racemic epinephrine use between cuffed and uncuffed tubes.
Bottom line: There is no difference in the complication rate between cuffed and uncuffed endotracheal tubes, but uncuffed endotracheal tubes did need to be changed more frequently.
Liang C, Zhang J, Pan G, Li X, Shi T, He W. Cuffed versus uncuffed endotracheal tubes in pediatrics: a meta-analysis. Open Med. 2018; 13:366-373.
Category: Toxicology
Keywords: Bupropion, TCAs, adolescents (PubMed Search)
Posted: 12/20/2018 by Hong Kim, MD
Click here to contact Hong Kim, MD
Selective serotonin reuptake inhibitors are the most common anti-depressant used today. However, the use bupropion in adolescents is increasing due the belief that it has fewer side effects than TCAs.
Using the National Poison Data System (2013 – 2016), the adverse effects of bupropion were compared to TCA in adolescents (13 – 19 years old) with a history of overdose (self harm).
Common clinical effects were:
TCA: n=1496; Bupropion: n=2257
| Clinical effects | TCAs | Bupropion |
| Tachycardia | 59.9% | 70.7% |
| Drowsiness/lethargy | 51.5% | 18.1% |
| Conduction disturbance | 22.2% | 15.6% |
| Agitation | 19.1% | 16.4% |
| Hallucination/delusions | 4.2% | 23.9% |
| Seizure | 3.9% | 30.7% |
| Vomiting | 2.7% | 20.0% |
| Tremor | 3.7% | 18.1% |
| Hypotension | 2.7% | 8.0% |
| Death | 0.3% | 0.3% |
Conclusion:
Bupropion overdose results in significant adverse effects in overdose; however, death is relatively rare.
Sheridan DC et al. Suicidal bupropion ingestions in adolescents: increased morbidity compared to other antidepressants. Clin Toxicol. 2018;56:360-364.
Category: Neurology
Keywords: ultrasound, lumbar puncture, LP, landmark (PubMed Search)
Posted: 12/12/2018 by WanTsu Wendy Chang, MD
(Updated: 2/2/2026)
Click here to contact WanTsu Wendy Chang, MD
Bottom Line: Consider using pre-procedural ultrasound-assistance for all lumbar punctures.
Gottlieb M, Holladay D, Peksa GD. Ultrasound-assisted lumbar punctures: a systematic review and meta-analysis. Acad Emerg Med. 2018 Aug 21. [Epub ahead of print]
Follow me on Twitter @EM_NCC
Category: Critical Care
Posted: 12/11/2018 by Mike Winters, MBA, MD
(Updated: 2/2/2026)
Click here to contact Mike Winters, MBA, MD
Noninvasive Ventilation in De-Novo Respiratory Failure
Thille AW, Frat JP. Noninvasive ventilation as acute therapy. Curr Opin Crit Care. 2018; 24:519-24.
Category: Orthopedics
Keywords: head injury, medication (PubMed Search)
Posted: 12/8/2018 by Brian Corwell, MD
Click here to contact Brian Corwell, MD
Retrospective chart review at a headache clinic seeing adolescent concussion patients
70.1% met criteria for probable medication-overuse headache
Once culprit over the counter medications (NSAIDs, acetaminophen) were discontinued,
68.5% of patients reported return to their preinjury headache status
Take home: Excessive use of OTC analgesics post concussion may contribute to chronic post-traumatic headaches
If you suspect medication overuse, consider analgesic detoxification
Heyer and Idris., 2014. Pediatr Neurol. Does analgesic overuse contribute to chronic post-traumatic headaches in adolescent concussion patients?
Category: Critical Care
Keywords: hyperoxia, oxygen therapy, saturation, SpO2, critical care, mechanical ventilation (PubMed Search)
Posted: 12/4/2018 by Kami Windsor, MD
Click here to contact Kami Windsor, MD
Hyperoxia has been repeatedly demonstrated to be detrimental in a variety of patients, including those with myocardial infarction, cardiac arrest, stroke, traumatic brain injury, and requiring mechanical ventilation,1-4 and the data that hyperoxia is harmful continues to mount:
Bottom Line: Avoid hyperoxia in your ED patients, both relatively stable and critically ill. Remove or turn down supplemental O2 added by well-meaning pre-hospital providers and nurses, and wean down ventilator settings (often FiO2). A target SpO2 of >92% (>88% in COPD patients) or PaO2 >55-60 is reasonable in the majority of patients.8
Category: Pharmacology & Therapeutics
Keywords: naloxone, overdose (PubMed Search)
Posted: 12/3/2018 by Ashley Martinelli
(Updated: 2/2/2026)
Click here to contact Ashley Martinelli
Providing naloxone to patients at risk for opioid overdose is now standard of care. A retrospective study evaluated the rate of naloxone obtainment after standardizing the process for prescribing naloxone in the emergency department and dispensing from the hospital outpatient pharmacy.
55 patients were prescribed naloxone. Demographics: mean age 48 years old, 75% male, 40% primary diagnosis of heroin diagnosis, 45.5% were prescribed other prescriptions.
Outcomes:
Barriers identified included lack of ED dispensing program, cost of medication, even though cost is minimal and can be waived, and likely multifactorial reasons why patients did not present to pharmacy as instructed.
Take Home Points:
Verdier M, Routsolias JC, Aks SE. Naloxone prescriptions from the emergency department: An initiative in evolution. Am J Emerg Med. 2018;37(1)164-165.
Category: Pediatrics
Posted: 12/1/2018 by Rose Chasm, MD
(Updated: 2/2/2026)
Click here to contact Rose Chasm, MD
Davies, P., and I. Maconochie. “The relationship between body temperature, heart rate and respiratory rate in children.” Emergency Medicine Journal 26.9 (2009): 641-643.
Daymont, Carrie, Christopher P. Bonafide, and Patrick W. Brady. “Heart Rates in Hospitalized Children by Age and Body Temperature.” Pediatrics 135.5 (2015): e1173-e1181.d
The National Institute for Health and Care Excellence. Pediatric Fever Guidelines, 2007 and 2013
Category: Toxicology
Keywords: alcohol withdrawal syndrome, phenobarbital (PubMed Search)
Posted: 11/29/2018 by Hong Kim, MD
Click here to contact Hong Kim, MD
Alcohol withdrawal syndrome is frequently treated with benzodiazepines following CIWA-Ar (Clinical Institute Withdrawal Assessment of Alcohol scale). There are other medications that are used as either second line or as adjunctive agents along with benzodiazepines. A retrospective study compared the clinical outcomes between phenobarbital vs. benzodiazepines-based CIWA-Ar protocol to treat AWS.
The primary was ICU length of stay (LOS); secondary outcome were hospital LOS, intubation, and use of adjunctive pharmacotherapy.
Study sample: 60 received phenobarbital and 60 received lorazepam per CIWA-Ar.
Phenobarbital protocol:
Results
|
| Phenobarbital | CIWA-Ar |
| ICU LOS | 2.4 days | 4.4 days |
| Hospital LOS | 4.3 days | 6.9 days |
| Intubation | 1 (2%) | 14 (23%) |
| Adjunctive agent use | 4 (7%) | 17 (27%) |
Conclusion
Phenobarbital therapy appears to be a promising alternative therapy for AWS. However, additional studies are needed prior to adapting phenobarbital as first line agent for AWS management.
Tidwell WP et al. Treatment of alcohol withdrawal syndrome: phenobarbital vs. CIWA-Ar protocol. Am J Crit Care. 2018 Nov;27(6):454-460. PMID: 30385536.
Category: Neurology
Keywords: diplopia, imaging, radiology, CT, ophthalmology (PubMed Search)
Posted: 11/28/2018 by Danya Khoujah, MBBS
(Updated: 2/2/2026)
Click here to contact Danya Khoujah, MBBS
Diplopia can be a challenging complaint to address in the ED. Although not all patients will require imaging, use the simplified table below to help guide the imaging study needed:
| Clinical Situation | Suspected Diagnosis | Imaging Study | |
| Diplopia + cerebellar signs and symptoms | Brainstem pathology | MRI brain | |
| 6th CN palsy + papilledema | Increased intracranial pressure (e.g. idiopathic intracranial hypertension or cerebral venous thrombosis) | CT/CTV brain | |
| 3rd CN palsy (especially involving the pupil) | Compressive lesion (aneurysm of posterior communicating or internal carotid artery) | CT/CTA brain | |
| Diplopia + thyroid disease + decreased visual acuity | Optic nerve compression | CT orbits | |
| Intranuclear ophthalmoplegia | Multiple sclerosis | MRI brain | |
| Diplopia + facial or head trauma | Fracture causing CN disruption | CT head (dry) | |
| Diplopia + multiple CN involvement (3,4,6) + numbness over V1 and V2 of trigeminal nerve (CN5) +/- proptosis | Unilateral, decreased visual acuity | Orbital apex pathology | CT orbits with contrast |
| Uni- or bi-lateral, normal visual acuity | Cavernous sinus thrombosis | CT/CTV brain | |
C.N.: cranial nerve
Margolin E, Lam C. Approach to a Patient with Diplopia in the Emergency Department. J Emerg Med. 2018 Jun;54(6):799-806
Category: Critical Care
Keywords: resuscitation, liver failure, cirrhosis (PubMed Search)
Posted: 11/20/2018 by Kami Windsor, MD
Click here to contact Kami Windsor, MD
A few (out of 10) tips for the care of sick patients with liver failure:
Fuhrmann V, Whitehouse T, Wendon J. The ten tips to manage critically ill patients with acute-on-chronic liver failure. Intensive Care Med. 2018;44(11):1932-5.
Category: Pediatrics
Keywords: Foreign bodies, coins, xrays (PubMed Search)
Posted: 11/16/2018 by Jenny Guyther, MD
(Updated: 2/2/2026)
Click here to contact Jenny Guyther, MD
Coins are the most commonly ingested foreign body in the pediatric age group with a peak occurrence in children less than 5 years old. X-rays are considered the gold standard for definitive diagnosis and location of metallic foreign bodies. This study aimed to find a way to decrease radiation exposure by using a metal detector.
19 patients ages 10 months to 14 years with 20 esophageal coins were enrolled in the study. All proximal esophageal coins were detected by the metal detector. 5 patient's failed initial detection of the coin with the metal detector and all of those patients had the coin in the mid or distal esophagus with a depth greater than 7 cm from the skin.
Bottom line: A metal detector may detect proximal esophageal coins. This may have a role in decreasing repeat x-rays.
Aljasser A, Elmaraghy C and Jatana K. Utilization of a handheld metal detector protocol to reduce radiation exposure in pediatric patients with esophageal coins. International Journal of Pediatric Otolaryngology. 2018: 104-108.
