Category: Toxicology
Keywords: nerve agents, organophosphate compounds (PubMed Search)
Posted: 3/18/2018 by Hong Kim, MD
(Updated: 3/21/2018)
Click here to contact Hong Kim, MD
Recently, an ex-Russian spy and his daughter were poisoned in Salisbury, England using a Soviet nerve agent called Novichok. He joins a list of defectors and ex-spies who's poisoning have been connected to Russia.
Nerve agents are organophosphate compounds, similar to the commercially available pesticides, but significantly more potent. Nerve agents such as VX take seconds to minutes to irreversibly inhibit acetylcholinesterase by “aging” and result in clinical toxicity.
Signs and symptoms
Treatment
Category: Critical Care
Posted: 3/21/2018 by Ashley Menne, MD
Click here to contact Ashley Menne, MD
Worsening hypoxemia is not uncommon upon initiation of VV ECMO for severe ARDS as tidal volumes drop to double digits (often <20cc) after transition to “lung rest” ventilator settings. The following are strategies to improve peripheral oxygenation:
1. Increase the blood’s oxygen content
- Ensure FIO2 of ECMO sweep gas is 1
- Increase ECMO blood flow
o Limited by cannula size and configuration – may require placement of additional venous drainage cannula
o Also limited by greater risk of recirculation and hemolysis
- Increase blood oxygen-carrying capacity
o Transfuse PRBCs – some advocate for goal hemoglobin 12-14, though institutional practices vary significantly
2. Minimize recirculation
- Maximize distance between drainage and return cannulae
3. Reduce oxygen consumption
- Optimize sedation and neuromuscular blockade. (This is not the appropriate scenario for awake ECMO.)
- Consider therapeutic hypothermia
4. Decrease cardiac output and intrapulmonary shunt
- Consider beta blocker (esmolol) infusion
- Prone positioning (only if staff are experienced with proning on ECMO as this poses significant risk of cannula displacement)
5. Consider switching to hybrid configuration (VVA – continued venous drainage cannula and venous return cannula with addition of arterial return cannula)
Montisci A, Maj G, Zangrillo A, Winterton D, Pappalardo F. Management of Refractory Hypoxemia During Venovenous Extracorporeal Membrane Oxygenation for ARDS. ASAIO J. 2015;61(3):227-236. doi:10.1097/MAT.0000000000000207.
Category: Critical Care
Posted: 3/20/2018 by Mike Winters, MBA, MD
Click here to contact Mike Winters, MBA, MD
Peri-Intubation Cardiac Arrest
De Jong A, et al. Cardiac arrest and mortality related to intubation procedure in critically ill adult patients: A multicenter cohort study. Crit Care Med. 2018; 46:532-9.
Category: Pediatrics
Keywords: Asthma, pediatrics, fluid (PubMed Search)
Posted: 3/16/2018 by Jenny Guyther, MD
Click here to contact Jenny Guyther, MD
Fluid overload (defined in this study as (fluid input-output)/weight)) is associated with longer hospital stays, longer treatment duration and oxygen use.
Bottom line: Treat dehydration appropriately but try not to over resuscitate the asthmatic. Further studies are needed before definitive recommendations are made.
This was a retrospective cohort study over 7 years at a single children’s hospital. Children included were older than 6 years and were admitted with no pneumonia or history of chronic lung disease. Fluid intake and output were collected for the initial 72 hours of hospitalization or discharge. The study included 1175 encounters. On average, 1% increase in fluid overload was associated with about a 7 hour increase in hospital stay, 6 hours longer of beta agonist and 2 hours longer of supplemental oxygen. Fluid overload of more than 7% was determined to be clinically meaningful showing an increased risk of requiring supplemental oxygen and non-invasive pressure ventilation. One of the limitations of this study that the authors mention is that the weight they used is the admission weight and the patient may already be dehydrated, thereby overestimating fluid overload.
Kantor et al. Fluid balance is Associated with Clinical Outcomes and Extravascular Lung Water in Children with Acute Asthma Exacerbation. American Journal of Respiratory and Critical Care Medicine. Epub ahead of print, Jan 9, 2018.
Category: Neurology
Keywords: stroke, prehospital, large vessel occlusion, NIHSS, RACE, LAMS, VAN (PubMed Search)
Posted: 3/14/2018 by WanTsu Wendy Chang, MD
(Updated: 2/2/2026)
Click here to contact WanTsu Wendy Chang, MD
Follow me on Twitter @EM_NCC
Category: Orthopedics
Keywords: Shoulder pain, muscle injury (PubMed Search)
Posted: 3/10/2018 by Brian Corwell, MD
(Updated: 2/2/2026)
Click here to contact Brian Corwell, MD
Pectoralis Major Rupture
Most commonly seen in male weightlifters
Usually occurs as a tendon avulsion
Incidence is increasing
Hx: Sudden, sharp, tearing sensation with pain and weakness with arm movement
PE: Palpable defect and deformity of anterior axillary fold. Bruising and swelling.
Deformity may not be obvious with arm by side and relaxed
Testing: Weakness with ADDuction and internal rotation
Treatment: Operative treatment has better outcomes but depends on patient subgroups
Nonoperative treatment generally indicated for partial ruptures and tears in the body of the pec and muscle tendon junction
Sling, ice and pain control.
Operative treatment generally for high demand patients (athletes) and bony avulsion injuries
Category: Toxicology
Keywords: cyanide, signs and symptoms (PubMed Search)
Posted: 3/8/2018 by Hong Kim, MD
Click here to contact Hong Kim, MD
Signs and symptoms of acute cyanide poisoning are not well characterized due to its rare occurrence. Commonly mentioned characteristics of bitter almond odor and cherry red skin have poor clinical utility.
Recently published review of 65 articles (102 patients) showed that most patients experienced following signs and symptoms:
There is no clear toxidrome for cyanide poisoning.
In a poisoned patient, health care providers should consider cyanide in their differential diagnosis in the presence of severe metabolic and lactic acidosis (lactic acid > 8 in isolated cyanide poisoning or > 10 in smoke/fire victim).
Parker-Cote JL et al. Challenges in the diagnosis of acute cyanide poisoning. Clin Toxicol 2018 Feb 8:1-9. doi: 10.1080/15563650.2018.1435886. [Epub ahead of print]
Category: Geriatrics
Keywords: bruising, elderly, forensic, abuse (PubMed Search)
Posted: 3/4/2018 by Danya Khoujah, MBBS
Click here to contact Danya Khoujah, MBBS
Category: Pharmacology & Therapeutics
Keywords: Fosfomycin, urinary tract infection, cystitis (PubMed Search)
Posted: 3/3/2018 by Wesley Oliver
Click here to contact Wesley Oliver
Fosfomycin is an antibiotic infrequently used for the treatment of urinary tract infections (UTIs). It has a broad spectrum of activity that covers both gram-positive (MRSA, VRE) and gram-negative bacteria (Pseudomonas, ESBL, and carbapenem-resistant Enterobacteriaceae), which is useful in the treatment of multidrug-resistant bacteria.
Fosfomycin is FDA approved for the treatment of uncomplicated UTIs in women due to susceptible strains of Escherichia coli and Enterococcus faecalis (3g oral as a single dose). Data has also demonstrated that it can be used for complicated UTIs; however, dosing is different in this population (3 g oral every 2-3 days for 3 doses). Fosfomycin is not recommended for pyelonephritis.
The broad spectrum of activity, in addition to only needing a single dose in most cases, makes fosfomycin an attractive option; however, it should be reserved for use in certain circumstances. Fosfomycin should not be considered as a first-line option. It is also more expensive than other medications (~$100/dose) and in countries with high rates of utilization bacteria are developing resistance to fosfomycin. In addition, most outpatient pharmacies do not keep this medication in stock.
Take-Home Point:
Fosfomycin should be reserved for multidrug-resistant UTIs in which other first-line options have been exhausted.
Gupta K, Hooton TM, Naber KG, et al; Infectious Diseases Society of America; European Society for Microbiology and Infectious Diseases. International clinical practice guidelines for the treatment of acute uncomplicated cystitis and pyelonephritis in women: a 2010 update by the Infectious Diseases Society of America and the European Society for Microbiology and Infectious Diseases. Clin Infect Dis. 2011;52(5): e103-e120. doi: 10.1093/cid/ciq257.
Michalopoulos AS, Livaditis IG, Gougoutas V. The revival of fosfomycin. Int J Infect Dis. 2011;15(11):e732-e739. doi: 10.1016/j.ijid.2011.07.007.
MONUROL [prescribing information]. St. Louis, MO: Forest Pharmaceuticals, Inc; 2007. www.accessdata.fda.gov/drugsatfda_docs/label/2008/050717s005lbl.pdf. Accessed 9/7/2017September 7, 2017.
Oteo J, Bautista V, Lara N, et al; Spanish ESBL-EARS-Net Study Group. Parallel increase in community use of fosfomycin and resistance to fosfomycin in extended-spectrum beta-lactamase (ESBL)-producing Escherichia coli. J Antimicrob Chemother. 2010;65(11):2459-2463. doi: 10.1093/jac/dkq346.
Raz R. Fosfomycin: an old—new antibiotic. Clin Microbiol Infect. 2012;18(1): 4-7. doi: 10.1111/j.1469-0691.2011.03636.x
Reffert JL, Smith WJ. Fosfomycin for the treatment of resistant gram-negative bacterial infections. Insights from the Society of Infectious Diseases Pharmacists. Pharmacotherapy. 2014;34(8):845-857. doi: 10.1002/phar.1434.
Vardakas KZ, Legakis NJ, Triarides N, Falagas ME. Susceptibility of contemporary isolates to fosfomycin: a systematic review of the literature. Int J Antimicrob Agents. 2016;47(4):269-285. doi: 10.1016/j.ijantimicag.2016.02.001.
Wankum, Michael, et al. “Fosfomycin Use.” Pharmacy Times, 30 Nov. 2017, www.pharmacytimes.com/publications/health-system-edition/2017/november2017/fosfomycin-use.
Category: Toxicology
Keywords: QTc, Dysrhythmias, drug overdose (PubMed Search)
Posted: 3/1/2018 by Kathy Prybys, MD
Click here to contact Kathy Prybys, MD
A leading cause of cardiac arrest in patients 40 years and younger is due to drug poisoning. Adverse cardiovascular events (ACVE) such as myocardial injury (by biomarker or ECG), shock (hypotension or hypoperfusion requiring vasopressors), ventricular dysrhythmias (ventricular tachycardia/fibrillation, torsade de pointes), and cardiac arrest (loss of pulse requiring CPR) are responsible for the largest proportion of morbidity and mortality overdose emergencies. Clinical predictors of adverse cardiovascular events in drug overdose in recent studies include:
Bottom line:
Obtain ECG and perform continuous telemetry monitoring in overdose patients with above risk factors. Patients with two or more risk factors have extremely high risk of in-hospital adverse cardiovascular events and intensive care setting should be considered.
Clinical risk factors for in-hospital adverse cardiovascular events after acute drug overdose. Manini AF, Hoffman RS, et al. Acad Emerg Med. 2015:22(5):499-507.
Incidence of adverse cardiovascular events in adults following drug overdose. Manini AF, Nelson LS, et al. Acad Emerg Med. 2012;19:843–9.
Category: Neurology
Keywords: headache, steroids, bleed (PubMed Search)
Posted: 2/28/2018 by Danya Khoujah, MBBS
Click here to contact Danya Khoujah, MBBS
Benign headaches are common in bodybuilders. However, several less benign headaches are worth noting:
All except the first two are exclusively reported in patients on anabolic steroids, growth hormone, and/or “energy” supplements. Make sure to ask your patient about these risk factors.
Busche K. Neurologic Disorders Associated with Weight lifting and Bodybuilding. Neurology Clinics. 26 (2008) 309–324
Category: Critical Care
Keywords: ICU, fungal infection, septic shock, antifungal therapy, empiric (PubMed Search)
Posted: 2/27/2018 by Kami Windsor, MD
Click here to contact Kami Windsor, MD
Which septic patients should receive empiric antifungal therapy?
Patients with fungemia only make up about 5% of patients presenting with septic shock, but invasive fungal infections are associated with increased hospital mortality (40-50%), prolonged ICU and hospital length of stay, and increased costs of care.1
The EMPIRICUS trial showed no mortality benefit to empiric antifungals for all, even patients with candidal colonization and recent exposure to antibiotics.2
Bottom Line
Therapy should always be tailored to the specific patient, but providers should strongly consider admininistering empiric echinocandin (micafungin, caspofungin) over fluconazole in patients with severe sepsis/septic shock and:
*Especially consider addition of antifungal in patients who do not show improvements after initial management with IVF and broad spectrum antibiotics in the ED.*
Which septic patients should receive empiric antifungal therapy?
Patients with fungemia only make up about 5% of patients presenting with septic shock, but invasive fungal infections are associated with increased hospital mortality (40-50%), prolonged ICU and hospital length of stay, and increased costs of care.1
The EMPIRICUS trial showed no mortality benefit to empiric antifungals for all, even patients with candidal colonization and recent exposure to antibiotics. (It demonstrated decreased rate of new invasive fungal infection, but did not increase survival).2
Risk factors for invasive fungal infections include:3
Which antifungal agent should we use?
Although older studies have not shown benefits to echinocandin, such as micafungin, over fluconazole as initial empiric antifungal therapy,4,5 a recent study by Garnacho-Montero et al. demonstrated improved 30 and 90-day mortality in patients with candidemia whose initial antibiotic was an echinocandin rather than fluconazole.6
Category: Orthopedics
Keywords: Mild traumatic brain injury, concussion (PubMed Search)
Posted: 2/25/2018 by Brian Corwell, MD
(Updated: 2/2/2026)
Click here to contact Brian Corwell, MD
The search for an objective reliable test for mild traumatic brain injury found an early promising result last week.
May be arriving in your hospital in the near future.
A handheld sideline version is sure to follow
The FDA approved the first blood test for concussion/mild TBI
Called the Banyan BTI (Brain Trauma Indicator)
This test measures 2 neural protein biomarkers released into the blood following mild TBI
The FDA approved this test within 6 months after reviewing data on just under 2,000 blood samples.
They concluded the Banyan BTI can predict the absence of cranial CT lesions with an accuracy greater than 99% and may reduce imaging in up to a 1/3rd
Be optimistic but consider the small sample size and remember that this test looks for biomarkers and may miss subtle cases where proteins didn’t leak. This test is NOT ready to be used for return to play decisions. It takes 3 to 4 hours to result and costs about $150. Other biomarkers are being investigated and may prove to be better
https://www.fda.gov/newsevents/newsroom/pressannouncements/ucm596531.htm
Category: Toxicology
Keywords: nystagmus, toxic (PubMed Search)
Posted: 2/22/2018 by Hong Kim, MD
Click here to contact Hong Kim, MD
Abnormal ocular movement (e.g. nystagmus) can often be observed in select CNS pathology.
Certain drugs/toxin overdose can also induce nystagmus.
In an "unknown" intoxication, physical exam findings such as nystagmus may help narrow the identity of the suspected ingestion/overdose.
Category: Critical Care
Posted: 2/21/2018 by Ashley Menne, MD
Click here to contact Ashley Menne, MD
-Nonischemic cardiomyopathy, classically seen in post-menopausal women preceded by an emotional or physical stressor
-Named for characteristic appearance on echocardiography and ventriculography with apical ballooning and contraction of the basilar segments of the LV – looks like a Japanese octopus trap or “takotsubo" (pot with narrow neck and round bottom)
-Clinical presentation usually similar to ACS with chest pain, dyspnea, syncope, and EKG changes not easily distinguished from ischemia (ST elevations – 43.7%, ST depressions, TW inversions, repol abnormalities) and elevation in cardiac biomarkers (though peak is typically much lower than in true ACS)
** Diagnosis of exclusion – only after normal (or near-normal) coronary angiography **
-Care is supportive and prognosis is excellent with full and early recovery in almost all patients (majority have normalization of LVEF within 1 week)
-Supportive care may include inotropes, vasopressors, IABP, and/or VA ECMO in profound cardiogenic shock
** LVOT Obstruction **
-occurs in 10-25% of patients with Takotsubo’s cardiomyopathy
-LV mid and apical hypokinesis with associated hypercontractility of basal segments of the LV predisposes to LV outflow tract obstruction
-Important to recognize as it is managed differently:
-may be worsened by hypovolemia, inotropes, and/or systemic vasodilatation
-mainstay of treatment is avoidance of the above triggers/exacerbating factors while increasing afterload
*phenylephrine is agent of choice +/- beta blockade
Take Home Points:
***Diagnosis of exclusion!!! Presentation very similar to ACS and ACS MUST be ruled out
* Treatment is supportive and similar to usual care for cardiogenic shock. Can be severe and require mechanical circulatory support!
*10-25% have LVOT obstruction. Manage with phenylephrine +/- beta blockade
Weiner MM, Asher DI, Augoustides G, et al. Takotsubo Cardiomyopathy?: A Clinical Update for the Cardiovascular Anesthesiologist. J Cardiothorac Vasc Anesth. 2017;31(1):334-344. doi:10.1053/j.jvca.2016.06.004.
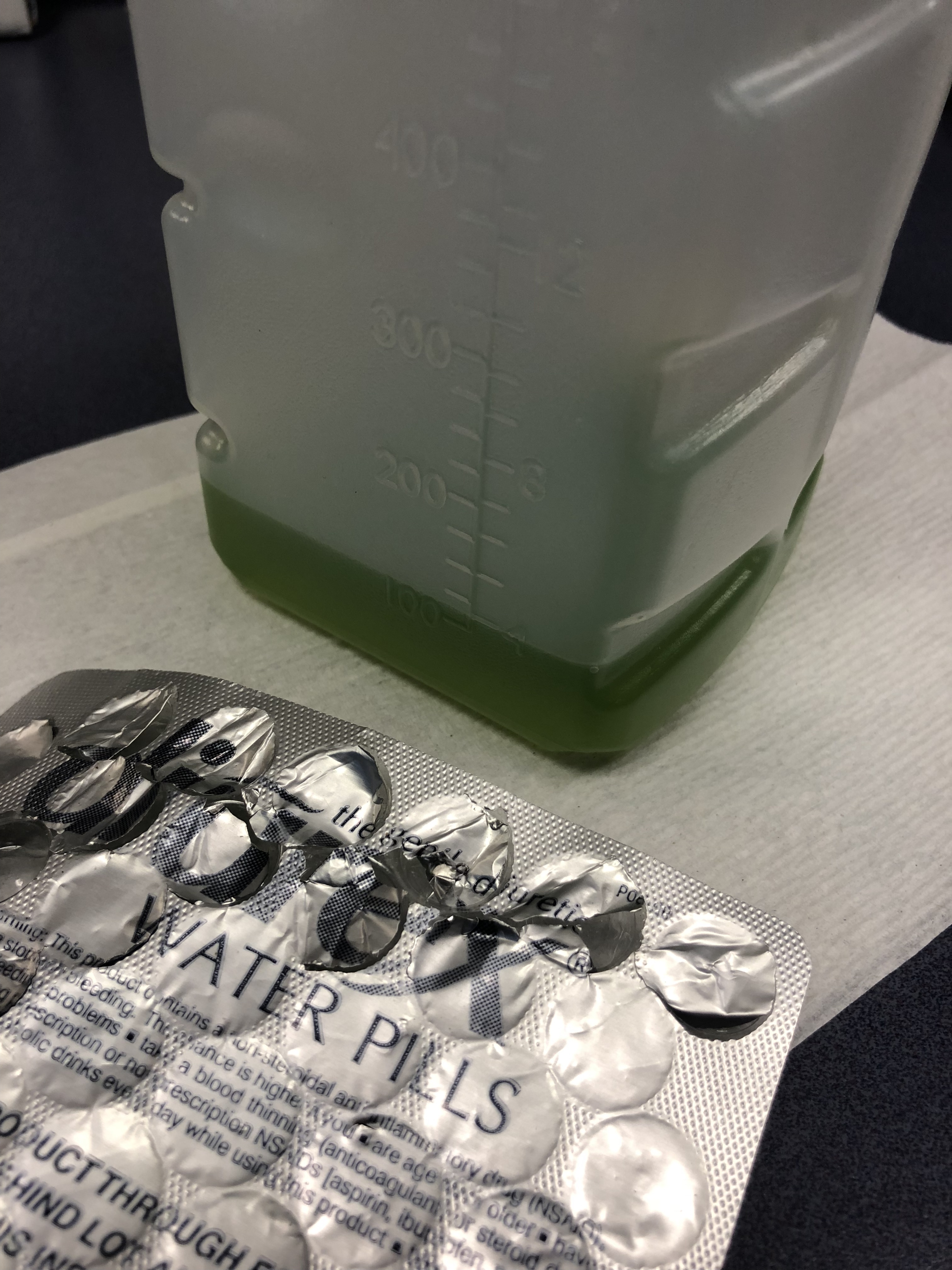
Category: Visual Diagnosis
Keywords: Green urine, diuretic (PubMed Search)
Posted: 2/17/2018 by Michael Bond, MD
(Updated: 2/2/2026)
Click here to contact Michael Bond, MD
75 y/o M is brought in by EMS after he fell off the light rail and hit his head. In the ED he is A&Ox3, and is asking for a urinal. Two minutes later the tech comes running to show you the following:
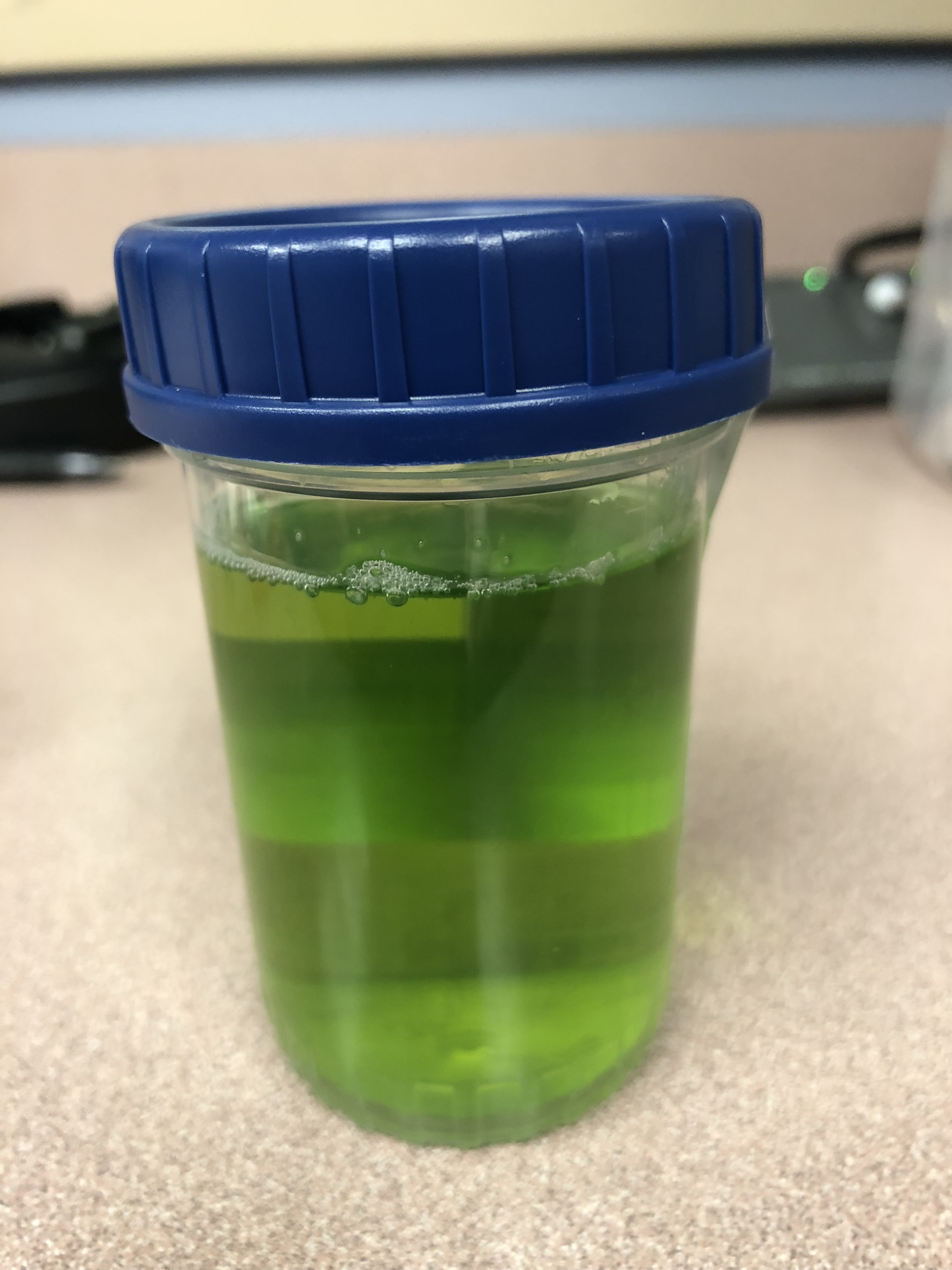
What is the cause of this patients Jolly Rancher Green Apple looking urine sample?
Answer:
Pamabrom side effect. Patient admitted to taking an “over the counter diuretic” called Diurex. The generic name is pamabrom. Pamabrom is a xanthine diuretic with only modest diuretic effect. It is marked mostly for weight loss to lose “water weight” and for relief of bloating during menstruation. A common side effect of the pills is a blue, green or golden discoloration of the urine. The capsules do not have the same side effect. The side effect is otherwise harmless and will disappear after stopping the diurex.
Category: Pediatrics
Keywords: foreign body, choking (PubMed Search)
Posted: 2/16/2018 by Jenny Guyther, MD
Click here to contact Jenny Guyther, MD
Patient: 11 month old with trouble breathing and color change after a family member sprayed air freshener. Symptoms have since resolved.
What are you concerned about in the attached xrays?
Answer: Radiolucent foreign body
Bilateral decubitus lateral films allow assessment of air trapping. The expectation is that the dependent lung will collapse partially in the normal patient. When a foreign body is present, there will be air trapping and hyperlucency in the dependent lung. In older patients, you can also obtain expiratory films to look for air trapping.
The patient had a food/mucus plug that was taken out of the right mainstem on bronchoscopy.
Foreign body aspiration is the 4th most common cause of accidental death in children younger than 3 years. Coughing and choking are the most common presenting symptoms.
CXRs are negative in > 50% of tracheal foreign bodies and 25% of bronchial foreign bodies.
More than 75% of foreign bodies in children less than 3 years are radiolucent.
Indirect signs of radiolucent foreign bodies include unilateral hyperinflation, atelectasis, consolidation and bronchiectasis (if presentation is delayed).
Bottom line: Consider bilateral lateral decubitus xrays in patients with a history concerning for foreign body.
Baram et al. Trachoebronchial Foreign Bodies in Children: The Role of Emergency Rigid Bronchoscopy. Global Pediatric Health. 2017: 1-5.
Category: Toxicology
Keywords: Cardiotoxicity, Bupropion, Ventricular dysrhythmia (PubMed Search)
Posted: 2/15/2018 by Kathy Prybys, MD
Click here to contact Kathy Prybys, MD
Bupropion (Wellbutrin, Zyban) is unique monocyclic antidepressant and smoking cessation agent that is structurally similar to amphetamines. Bupropion blocks dopamine and norepinephrine reuptake and antagonizes acetylcholine at nicotinic receptors.
Bottom line:
Bupropion is a common cause of drug induced seizures but in severe overdose can also cause prolonged QTc and wide complex ventricular dysrhythmia that may be responsive to sodium bicarbonate. All patients with an overdose of bupropion should have an ECG performed and cardiac monitoring to watch for conduction delays and life-threatening arrhythmias.
Wide complex tachycardia after bupropion overdose. Franco V. Am J Emerg Med. 2015 Oct;33 (10):1540.
Delayed bupropion cardiotoxicity associated with elevated serum concentrations of bupropion but not hydroxybupropion. Al-Abri SA, Orengo JP, et al. Clin Tox. 2013 Dec ;51(10):1230-4.
QRS widening and QT prolongation under bupropion: a unique cardiac electrophysiological profile. Caillier B. Pilote S. et al. Fundam Clin Pharmacol. 2012 Oct;26(5): 599-608.
Comparison of Resuscitative Protocols for Bupropion Overdose Using Lipid Emulsion in a Swine Model. Fulton LV, Fabrich RA, et al, Military Medicine 181, 5:482, 2016.
Category: Neurology
Keywords: occipital nerve block, migraine, headache (PubMed Search)
Posted: 2/14/2018 by WanTsu Wendy Chang, MD
(Updated: 2/15/2018)
Click here to contact WanTsu Wendy Chang, MD
Zhang H, Yang X, Lin Y, Chen L, Ye H. The efficacy of greater occipital nerve block for the treatment of migraine: a systematic review and meta-analysis. Clin Neurol Neurosurg. 2018;165:129-133.
Follow me on Twitter @EM_NCC
Category: Orthopedics
Keywords: Hip pain, athletes (PubMed Search)
Posted: 2/10/2018 by Brian Corwell, MD
(Updated: 2/2/2026)
Click here to contact Brian Corwell, MD
Femoral neck stress fractures
Adults>kids
Represents 5% of all stress fractures
Usually due to repetitive abductor muscle contraction
As with all stress fractures can occur in 2 types
1) Insufficiency type (normal physiologic stress on abnormal bone)
2) Fatigue type (abnormal/excessive physiologic stress on normal bone)
2 locations on interest:
1) Compression side (inferior femoral neck)
2) Tension side (superior femoral neck)
History: Insidious onset of groin or lateral hip pain associated with weight bearing
Exam: Antalgic gait, pain with hip log roll and with FABER (hip flexion, Abduction and external rotation test)
Treatment:
Compression side: reduced weight bearing and activity modification
Tension side: Non weight bearing (due to high risk of progression to displacement with limited weight bearing) AND surgical consultation for elective pinning to prevent displacement. If displaced, will require ORIF
Pevlis, hip and thigh injuries and conditions. Heidi Prather and Devyani Hunt. In Sports Medicine Study Guide and Review for Booards 2nd Edition. 2017
