Category: Pediatrics
Keywords: Kawasaki's disease, SJS, TEN, dermatitis (PubMed Search)
Posted: 2/9/2018 by Mimi Lu, MD
Click here to contact Mimi Lu, MD
Case: 5 year old presents to the ED with 2 weeks of fever. She has extensive cracked, bleeding lips and a rash on her hands and feet. She was recently diagnosed with “walking pneumonia” and hand, foot and mouth disease this week. Her pediatrician sent her in for further workup after she was found to have an elevated CRP on outpatient labs. A similar picture appears in the link below:
What's the diagnosis?
The diagnosis of Mycoplasma pneumonia-induced rash and mucositis (MIRM) was recently termed in the 2015 Journal of American Academy of Dermatology. It is characterized by mucocutaneous eruptions with prominent mucosal involvement. 94% of patients in the reviewed cases had extensive oral lesions that can range from erosions, ulcers or vesiculobullous lesions. 82% of patients had ocular involvement characterized by purulent bilateral conjunctivitis. In 63% of cases, patients were found to have urogenital lesions. Almost all of these patients had prodromal symptoms of cough and fever preceding the eruption by 1 week. The disease was found to be most prominent with young (11.9 ± 8.8 years) and with a 66% male predominance. The treatment is antibiotics such as azithromycin and oral corticosteroids with a minority of patients requiring IVIG. These patients have a good prognosis.
Bottom Line: Consider MIRM in patients with extensive mucosal disease that do not completely fit the criteria of Kawasaki’s or Stevens-Johnson Syndrome/ Toxic Epidermal Necrolysis.
Reference:
Canavan TN, Mathes EF, Frieden I, Shinkai K. Mycoplasma pneumoniae-induced rash and mucositis as a syndrome distinct from Stevens-Johnson syndrome and erythema multiforme: a systematic review. J Am Acad Dermatol. 2015
Feb;72(2):239-45.
Category: Critical Care
Posted: 2/6/2018 by Mike Winters, MBA, MD
Click here to contact Mike Winters, MBA, MD
Hyperoxia and the Post-Arrest Patient
Roberts BW, et al. Association between early hyperoxia exposure after resuscitation from cardiac arrest and neurological disability: a prospective multi-center protocol-directed cohort study. Circulation 2018; epub ahead of print.
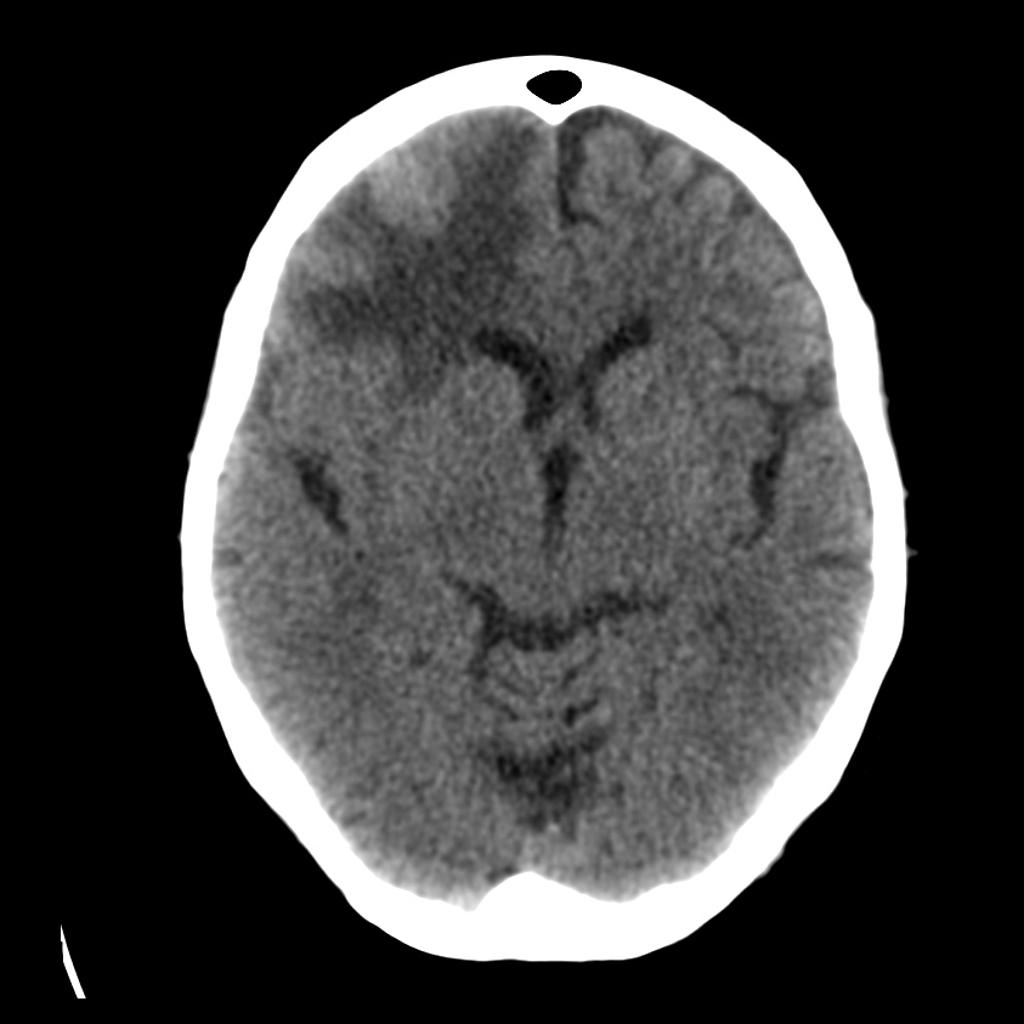
Category: Geriatrics
Keywords: dizziness, CT, MRI, Cerebellar (PubMed Search)
Posted: 2/5/2018 by Danya Khoujah, MBBS
(Updated: 2/2/2026)
Click here to contact Danya Khoujah, MBBS
15% of older adults presenting to ED for dizziness have serious etiologies; 4-6% are stroke-related and sensitivity of CT for identifying stroke or intracranial lesion in dizziness is poor (16%), so if CNS etiology suspected, seek neuro consult or MRI (83% sensitivity)
Lo AX, Harada CN. Geriatric dizziness: evolving diagnostic and therapeutic approaches for the emergency department. Clin Geriatr Med. 2013;29(1):181-204.
Category: Infectious Disease
Keywords: sepsis, pseudomonas (PubMed Search)
Posted: 2/3/2018 by Ashley Martinelli
(Updated: 2/2/2026)
Click here to contact Ashley Martinelli
Debating between cefepime or piperacillin/tazobactam for your septic patient? Use this table to help you decide.
|
|
| Cefepime | Piperacillin/Tazobactam |
| Gram Negative Spectrum | Pseudomonas aeruginosa | Yes | Yes |
| Aerobic gram negative organisms | E. coli Klebsiella sp. Proteus mirabilis M catarrhalis H. influenza | E. coli Klebsiella sp. Proteus mirabilis M. catarrhalis H. influenza | |
| Anerobic gram negative organisms | No | B. fragilis
| |
| Gram Positive Spectrum | MRSA | No | No |
| Aerobic gram positive organisms | MSSA CoNS Group A Strep S. pneumoniae
| MSSA CoNS Group A Strep S. pneumoniae E. faecalis | |
| Anaerobic gram positive organisms | P. acnes Peptostreptococci | P. acnes Peptostreptococci Clostridium sp. | |
| Infection Site Concerns | CNS Penetration | Yes | No1 |
| Urine Penetration | Yes | Yes | |
| Lung Penetration | Yes | Low2 | |
| Dosing Frequency (Normal Renal Function) | Q8h | Q6h | |
1. Tazobactam CNS penetration is limited, thus limiting antipseudomonal activity in the CNS
2. Low pulmonary penetration, may not achieve therapeutic levels in patients with critical illness
Take home points:
-Piperacillin/tazobactam differs in spectrum with its ability to cover enterococcus and anaerobes. Consider for sepsis with gastrointestinal source
-Cefepime can be used for CNS infections and readily achieves therapeutic concentrations in the lungs. Metronidazole can be added to ensure anaerobic organism coverage.
-Piperacillin/tazobactam should be dosed every 6 hours in patients with normal renal function to achieve therapeutic concentration.
1. Gilbert, D. N., Chambers, H. F., Eliopoulos, G. M., Saag, M. S., & Pavia, A. T. (2016). Sanford guide to antimicrobial therapy 2016. 46th edition. Sperryville, VA, USA: Antimicrobial Therapy, Inc.
2. Nau R, Kinzig-Schippers M, Sörgel F, et al. Kinetics of piperacillin and tazobactam in ventricular cerebrospinal fluid of hydrocephalic patients.?Antimicrobial Agents and Chemotherapy. 1997;41(5):987-991.
3. Felton T, McCalman K, Malagon I, et al. Pulmonary penetration of piperacillin and tazobactam in critically ill patients. Clinical pharmacology and therapeutics. 2014;96(4):438-448. doi:10.1038/clpt.2014.131.
4. Boselli E, Breilh D, Duflo F, et al. Steady-state plasma and intrapulmonary concentrations of cefepime administered in continuous infusion critically ill patients with severe nosocomial pneumonia. Critical Care Medicine.2003;31:2102-2106.
Category: Pediatrics
Keywords: Pediatrics, Abdominal Pain (PubMed Search)
Posted: 2/2/2018 by Megan Cobb, MD
Click here to contact Megan Cobb, MD
 Your patient is an18 months old female with intermittent abdominal pain for the last 4-5 days. She has history of constipation and soy allergy, seen at an outside hospital three days ago for the same. She had an xray and was discharged home with instructions for at home clean out with diagnosis of constipation.
Your patient is an18 months old female with intermittent abdominal pain for the last 4-5 days. She has history of constipation and soy allergy, seen at an outside hospital three days ago for the same. She had an xray and was discharged home with instructions for at home clean out with diagnosis of constipation.
Mother is bringing her to your ED because the pain is back. The laxatives helped somewhat, but her symptoms have returned. She reports that the patient cries spontaneously, lasting 1-2 minutes, then completely resolves. These episodes happen at multiple times during the day.
ROS: Decreased appetite and energy, but NO fevers, vomiting, diarrhea, bloody stool, abdominal distension, hematuria, or lethargy.
Intussusception classically presents with colicky abdominal pain, palpable mass, and currant jelly stools, but in less than 50% of patients. The clinical presentation of intussusception actually occurs on a spectrum. Children who present early in their course may look well with intermittent, unexplained crying episodes, while others may be febrile, dehydrated, with bloody stools, and be septic. The diagnosis can be missed in up to 60% of children presenting for initial evaluation. Identified risk factors include any syndrome or abnormality causing a lead point, ie Meckel's Diverticulum, Familial Polyposis, lymphoma and Henoch-Scholein Purpura, as well as GI infections, bacterial and viral, (Adenovirus, Rotavirus, and HHV6, etc.)
On exam, our patient's abdomen was soft but hard to evaluate due to behavior. Flat plate AXR demonstrated a circular hyperdensity in the RUQ, which on ultrasound, corresponded to a large ileocolic intussusception. She was successfully treated with air enema reduction, which in recent review has the lowest recurrence rate of intussusception.
Bottom Line -
In children with intermittent abdominal pain or unexplained crying episodes, consider intussusception on your differential, as more than half are missed on initial presentation, which can be subtle. Late presentations can include bowel perforation, peritonitis, sepsis, and shock. If diagnosed, arrange for enema reduction or transfer to a facility with this capability.
References:
Waseem M, Rosenberg HK. Intussusception. Pedi Emer Care. Nov 2008, 24(11): 793-800.
Gluckman S, Karpelowsky J, Webster AC, McGee RG. Management for intussusception in children. Cochrane Review of Systematic Databases. 2017; Issue 6.
Category: Toxicology
Posted: 2/1/2018 by Kathy Prybys, MD
(Updated: 2/2/2018)
Click here to contact Kathy Prybys, MD
47 year old woman presents with cough, headache, weakness, and low grade fever. Her symptoms have been present for several days. Vital signs are temperature 99.9 F, HR 96, RR 16, BP 140/88, Pulse Ox 98%. Physical exam is nonfocal. She is Influenza negative. She is treated with Ibuprofen and oral fluids. Upon discharge she mentions she is having difficulty hearing and feels dizzy. Upon further questioning she admits to ringing in her ears. What tests should you order?
ANSWER: Salicylate and Acetaminophen levels.
Patient admits to taking BC Powder, an over the counter medication to self treat over the past few days. The active ingredients of BC powder are 845 mg of aspirin and 65 mg of caffeine. Her salicylate level is 45 mg/dL. Her other labs are unremarkable. Serial salicylate levels should be obtained every 2-4 hours and correlated with blood pH and clinical findings.
Salicylates commonly cause of ototoxicity. Tinnitus and hearing loss are early signs of salicylate toxicity and occur between 20-45 mg/dL. Other CNS effects are vertigo, hyperventilation, delirium, seizure, lethargy, and coma. Salicylate and acetaminophen are contained in numerous over the counter medications and are often mistakenly considered safe by the public resulting in accidental overdose. Early signs of toxicity can be missed or confused with other illness with serious consequences.
American College of Medical Toxicology. Guidance Document: Management Priorities in Salicylate Toxicity. J Med Tox. 2015;11(1):149-152.
Emergency department management of the salicylate-poisoned patient. O'Malley GF. Emerg Med Clin North Am. 2007 May ;25(2):333-46.
Category: Critical Care
Keywords: sepsis, septic shock, glucocorticoids, steroids, hydrocortisone (PubMed Search)
Posted: 1/29/2018 by Kami Windsor, MD
Click here to contact Kami Windsor, MD
As hospital volumes increase and ED patient boarding becomes more commonplace, emergency physicians may find themselves managing critically ill patients beyond the initial resuscitation.
The benefit of glucocorticoids in critically ill patients with septic shock has remained a topic of controversy for decades due to conflicting studies, including the 2002 Annane trial and the 2008 CORTICUS trial, which had opposing results when it came to the mortality benefit of steroids.
The results of the eagerly-awaited ADRENAL trial, a multicenter randomized controlled trial investigating the benefit of steroids in septic shock, were released earlier this month:
Take Home Points:
1. Administration of standard daily dose hydrocortisone by infusion does not seem to affect mortality in septic shock.
2. Emergency providers should continue to consider stress-dose steroids in patients with shock and a high risk of adrenal insufficiency (e.g., chronic steroid therapy, genetic disorders, infectious adrenalitis, etc).
Category: Orthopedics
Keywords: Dental avulsion, tooth, trauma (PubMed Search)
Posted: 1/27/2018 by Brian Corwell, MD
Click here to contact Brian Corwell, MD
Dental Avulsion in the field/sporting event
- Only replace avulsed secondary teeth
- Handle the tooth by the crown only
- Rinse tooth with cold running water gently (the root should not be wiped)
- Immediate attempt to reimplant permanent tooth into socket by 1st capable person:
* Time is tooth: Each minute tooth is out of socket reduces tooth viability by 1%
* Best chance of success if reimplant done within 5–15 min*? Poor tooth viability if avulsed for >1 hr
- If unsuccessful, place tooth in a transport solution (from most to least desirable):
- Hanks balanced salt solution (HBSS)
* Balanced pH culture media available commercially in the Save-A-Tooth kit
* Effective hours after avulsion
- Cold milk:
* Best alternative storage medium
* Place tooth in a container of milk that is then packed in ice (prevents dilution)
- Saliva:
* Store in a container of parent or child's saliva
- Never use tap water or dry transport
Category: Neurology
Keywords: edema, hemorrhage, tumor, CT, MRI, contrast (PubMed Search)
Posted: 1/24/2018 by Danya Khoujah, MBBS
(Updated: 2/2/2026)
Click here to contact Danya Khoujah, MBBS
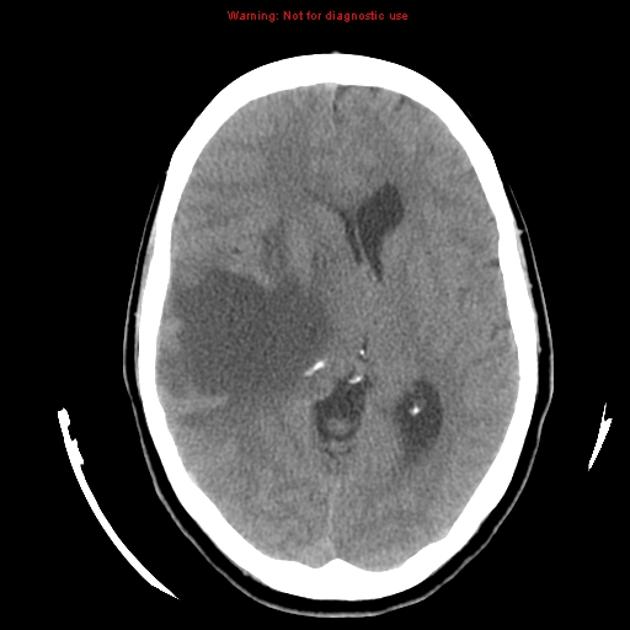

Klein JP, Dietrich J. Neuroradiologic Pearls for Neuro-oncology. Continuum 2017;23(6):1619-1634.
Category: Pediatrics
Keywords: Pain control in children, opiates, NSAIDS, motrin, orthopedic (PubMed Search)
Posted: 1/19/2018 by Jenny Guyther, MD
Click here to contact Jenny Guyther, MD
Bottom line: Oral morphine was not superior to ibuprofen and both drugs decreased pain with no difference in efficacy. Morphine was associated with more adverse events.
Poonai et al. Oral Morphine versus ibuprofen administered at home for postoperative orthopedic pain in children: a randomized controlled trial. CMAJ 2017. 189: E1252-E1258.
Category: Toxicology
Keywords: Liver dialysis, MARS (PubMed Search)
Posted: 1/18/2018 by Kathy Prybys, MD
(Updated: 1/19/2018)
Click here to contact Kathy Prybys, MD
Acute liver failure carries a high morbidity without liver transplantation. Liver support systems can act as “bridge” until an organ becomes available for the transplant procedure or until the liver recovers from injury. Artificial liver support systems temporally provide liver detoxification utilizing albumin as scavenger molecule to clear the toxins without providing synthetic functions of the liver (coagulation factors). One of the most widely used devices is the Molecular Adsorbent Recirculating System (MARS).This system has 3 different fluid compartments: blood circuit, albumin with charcoal and anion exchange column, and a dialysate circuit that removes protein bound and water soluble toxins with albumin.
Bottom Line
MARS therapy could be a potentially promising life saving treatment for patients with acute poisoning from drugs that have high protein-binding capacity and are metabolized by the liver, especially when concomitment liver failure. Consider consultation and transfer of patients to liver center.
The Molecular Adsorbent Recirculating System (MARS®) in the Intensive Care Unit: A Rescue Therapy for Patients with Hepatic Failure. F Saliba, Critical Care 10.1 (2006): 118.
Category: Orthopedics
Keywords: Head injury, concussion, sideline (PubMed Search)
Posted: 1/13/2018 by Brian Corwell, MD
(Updated: 2/2/2026)
Click here to contact Brian Corwell, MD
Concussion – Where are we now?
The Sport Concussion Assessment Tool 5th edition (SCAT 5) was released in 2017
It is a standardized tool to assist health care professionals in the evaluation of sport associated concussions
It should be used for those 13 years and older (there is a child version for younger athletes)
Print and bring to the sideline for your next coverage event!
http://bjsm.bmj.com/content/bjsports/early/2017/04/26/bjsports-2017-097506SCAT5.full.pdf
Some points to consider:
It should take at least 10 minutes to complete. Any less and you may not be performing the test correctly
The SCAT5 is the standard tool used in concussion assessment in the NCAA and NFL and other professional sports
Some symptoms of concussion appear over time. For example, an athlete may have zero or minimal symptoms immediately after yet be considerably symptomatic in 10 to 15 minutes.
-Follow up screening evaluations are essential even in those with a negative initial sideline screening test
The SCAT5 should be used immediately after injury
-Utility decreases post injury after days 3-5
-The included symptom checklist has utility in tracking recovery
-Attempt to perform in an environment free of distractions (crowd noise, bad weather)
The clinical utility of the SCAT5 can be enhanced by adding assessment of other factors such as reaction time, balance assessment, video-observable signs (if available) and oculomotor screening.
Category: Pediatrics
Posted: 1/12/2018 by Mimi Lu, MD
Click here to contact Mimi Lu, MD
Category: Toxicology
Keywords: activated charcoal, large acetaminophen overdose, NAC dose (PubMed Search)
Posted: 1/11/2018 by Hong Kim, MD
(Updated: 2/2/2026)
Click here to contact Hong Kim, MD
Acetaminophen (APAP) overdose is the leading cause of liver failure in the U.S. and Europe. Large APAP ingestion can result in hepatotoxicity despite the early initiation of n-acetylcysteine (NAC).
A recently published study from Austrialia investigated the effect of activate charcoal and increasing the NAC dose for large APAP overdose patients (3rd bag: 100 to 200 mg/kg over 16 hours) during first 21 hours of NAC therapy
acetaminophen ratio (first APAP level taken between 4 to 16 hour post ingestion / APAP level on the Rumack nomogram line at that time point) was determined to compare APAP levels at different time points among study sample
e.g.
first APAP level at 4 hour post ingestion = 400
APAP level on the Rumack APAP nomogram at 4 hour post ingestion = 150
APAP ratio = 400/150 = 2.67
Findings:
Conclusion:
Note: Any increase in NAC dosing from the standard 21 hour therapy should be performed after consulting your regional poison center.
Chiew AL et al. Massive paracetamol overdose: an obsevational study of the effect of activated charcoal and increased acetylcysteine dose (ATOM-2). Clin Toxicol 2017;55:1055-1065. PMID: 28644687.
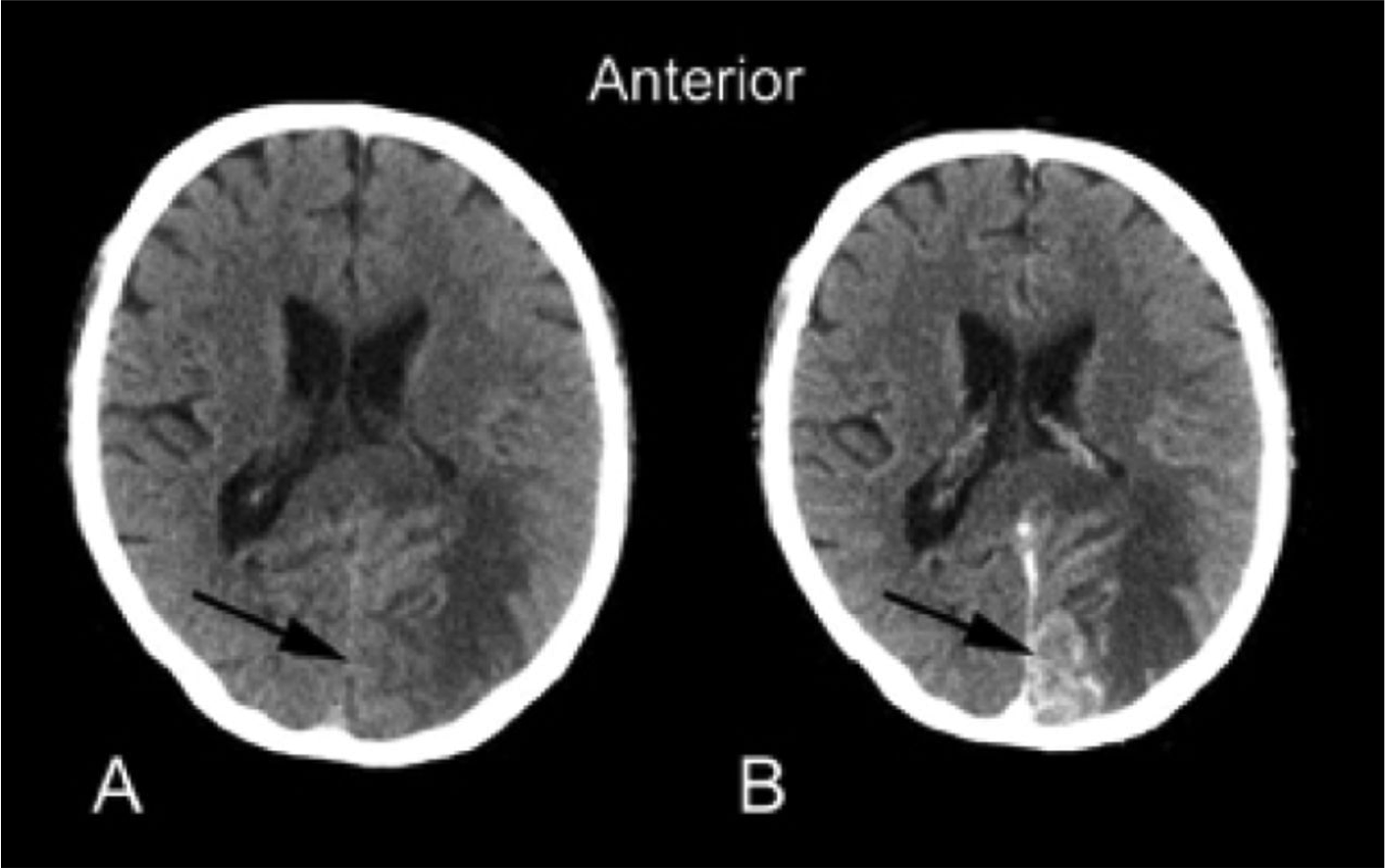
Category: Neurology
Keywords: RCVS, thunderclap headache, migraine, SAH (PubMed Search)
Posted: 1/10/2018 by WanTsu Wendy Chang, MD
Click here to contact WanTsu Wendy Chang, MD
Bottom Line: Consider RCVS in the differential of thunderclap headache and in patients who present with worse than usual migraine headache.
Arrigan MT, Heran MKS, Shewchuk JR. Reversible cerebral vasoconstriction syndrome: an important and common cause of thunderclap and recurrent headaches. Clin Radiol. 2017 Dec 21 [Epub ahead of print]
Follow me on Twitter @EM_NCC
Category: Critical Care
Posted: 1/9/2018 by Mike Winters, MBA, MD
(Updated: 2/2/2026)
Click here to contact Mike Winters, MBA, MD
Septic Cardiomyopathy
Beesley S, et al. Septic cardiomyopathy. Crit Care Med 2018. [epub ahead of print]
Category: Pharmacology & Therapeutics
Keywords: Epinephrine, Asthma (PubMed Search)
Posted: 1/8/2018 by Wesley Oliver
Click here to contact Wesley Oliver
Patients with severe asthma exacerbations that are unresponsive to inhaled beta-agonists may require the use of epinephrine to control their symptoms. When patients get to this point what route of administration should be used for the administration of epinephrine?
The most recent asthma guidelines (published in 2007) recommend the use of SubQ epinephrine 0.3-0.5 mg every 20 minutes for 3 doses. Drug references typically list SubQ or IM epinephrine 0.01 mg/kg (~0.3-0.5 mg) every 20 minutes as appropriate routes of administration. There is currently no data demonstrating that one route of administration is better than the other in patients with asthma; however, in other disease states, such as anaphylaxis, IM epinephrine is preferred due to the more rapid and reliable absorption over SubQ administration.
Auto-injectors that administer IM epinephrine 0.3 mg are available. These auto-injectors may decrease the risk of medications error; however, they can be expensive. SubQ administration requires the use of a syringe and a vial/ampule of 1 mg/mL epinephrine.
Bottom Line: Either SubQ or IM epinephrine administration is appropriate for patients with severe asthma exacerbations. The preferred method at a given institution will be dictated by historical practice, risk of medication dosing errors, and drug cost.
1. National Asthma Education and Prevention Program, Third Expert Panel on the Diagnosis and Management of Asthma. Expert Panel Report 3: Guidelines for the Diagnosis and Management of Asthma. Bethesda (MD): National Heart, Lung, and Blood Institute (US); 2007 Aug. Available from: https://www.ncbi.nlm.nih.gov/books/NBK7232/
2.Simons FER, Ardusso LRF, Bilo MB, El-Gamal YM, Ledford DK, Ring J, et al. World Allergy Organization Anaphylaxis Guidelines: Summary. J Allergy Clin Immunol. 2011;127(3):587–93. e1-e20.
Category: Geriatrics
Keywords: Delirium, dementia, screening, altered (PubMed Search)
Posted: 1/7/2018 by Danya Khoujah, MBBS
Click here to contact Danya Khoujah, MBBS
A recent study was undertaken to validate the 4A's Test for the assessment of delirium in the elderly, with particular focus on inpatient geriatric patients; it revealed that the tool had high sensitivity in detecting delirium, particularly in those with dementia or language barriers, in whom this diagnosis can often be difficult to make. Further studies would be useful in a similar demographic of emergency department geriatric patients to confirm that this straightforward test is generalizable to the emergency department geriatric patient population.
The 4A’s Test used for this study was accessed from www.the4AT.com (Free Access).
The 4AT consists of four items with a maximum achievable score of 12.
Item 1 determines patient’s level of alertness by operator observation (maximum score 4).
Items 2 and 3 screen cognition and attention with the use of the Abbreviated Mental Test-4 (AMT-4) (maximum score 2) and Months Backwards (maximum score 2).
Item 4 assesses for ?uctuation and acute changes in mental state (score 0 or 4).
A score of 0 indicates delirium or cognitive impairment is unlikely.
A score between 1 and 3 indicates possible cognitive impairment (corresponding to stand alone dementia screening tools).
A score of 4 and above is suggestive of delirium.
Category: Pediatrics
Keywords: NAT, non-accidental trauma, abusive head trauma, intra-abdominal injury, burns (PubMed Search)
Posted: 1/6/2018 by Megan Cobb, MD
Click here to contact Megan Cobb, MD
In addition to suspicion of NAT with traumatic brain injury and burns, remember these other high risk injuries and features:
- Duodenal injuries in children <4 y/o
- Frena injuries in non-ambulating children
- Proximal and midshaft humeral fractures > supracondylar fractures
- Any bruising on the trunk, ears, neck, or with larger size or pattern
- Delay in seeking care, inconsistent history, mechanism inconsistent with developmental age, and blame of a sibling or other child inflicting harm are all historical features also high risk.
Non-accidental trauma (NAT) continues to be a sad, but prevelant pathology in the United States. It is estimated that one million children in the US have been victims of maltreatment. As high as one third of children with NAT had the abuse missed on prior medical evaluation. There are several screening tools and clinical prediction rules that have been developed for clinical use, but none are to be used as substitutes for full skeletal survey and CT scan when indicated.
TEN-4 (clinical prediction rule): 97% sensitivity, 84% specificity with regards to NAT in the setting of bruising by age, location and characteristic.
PEDIBIRN (clinical prediction rule): 96% sensitive, 43% specificity with regards to abusive head trauma in children less than 3 years old.
PredAHT (clinical prediction rule): 72% sensitive, 86% specificity, also for abusive head trauma less than 3 years old.
PIBIS (screening tool): scoring system for well appearing infants presenting with brief resolved unexplained event (BRUE), previously called apparent life threatening event or ALTE.
Escobar, MA, et al. The association of nonaccidental trauma with historical factors, examination findings, and diagnostic testing during the initial trauma evaluation. Journal Trauma Acute Care Surgery. 2017; 82(6).
Category: Critical Care
Keywords: endotracheal intubation, cardiac arrest, airway, respiratory failure (PubMed Search)
Posted: 1/2/2018 by Kami Windsor, MD
(Updated: 1/4/2018)
Click here to contact Kami Windsor, MD
Although the data is limited, current published rates of in-hospital, non-operating room peri-intubation cardiac arrest (PICA) range from 2 to 6%.1,2,3
Several risk factors associated with PICA have been identified and include:
Other common findings:
Bottom Line: Endotracheal intubation is one of the riskiest procedures we regularly perform as emergency physicians.
References
1. Heffner AC, Swords DS, Neale MN, Jones AE. Inicidence and factors associated with cardiac arrest complicating emergency airway management. Resuscitation. 2013; 84(11):1500-4.
2. Kim WY, Kwak MK, Ko BS, et al. Factors associated with the occurrence of cardiac arrest after emergency tracheal intubation in the emergency department. PLoS One. 2011; 9(11):e112779.
3. Wardi G, Villar J, Nguyen T, et al. Factors and outcomes associated with inpatient cardiac arrest following emergent endotracheal intubation. Resuscitation. 2017; 121:76-80.
