Category: Critical Care
Posted: 7/25/2017 by Mike Winters, MBA, MD
(Updated: 2/2/2026)
Click here to contact Mike Winters, MBA, MD
Improving Resuscitation Performance
Lauria M, et al. Psychological skills to improve emergency care providers' performance under stress. Ann Emerg Med. 2017; epub ahead of print.
Category: Orthopedics
Keywords: Knee instability (PubMed Search)
Posted: 7/23/2017 by Brian Corwell, MD
Click here to contact Brian Corwell, MD
PCL injuries can sometimes have involvement of the posterolateral corner (PLC)
The dial test can be used to diagnose posterior lateral instability and help differentiate it from isolated PCL injuries
The dial test involves comparing the amount of external rotation of the lower leg at the knee while the knees are in 30° and in 90° of knee flexion.
https://www.youtube.com/watch?v=rnk62Y-nDSQ
An isolated injury to the posterolateral corner will result in more than 10° of external rotation in the injured knee that is present at 30° but not at 90° of knee flexion.
http://www.kneejointsurgery.com/wp-content/uploads/2015/06/DIAL-TEST.jpg
http://www.kneejointsurgery.com/wp-content/uploads/2015/06/DIAL-TEST-90.jpg
http://www.kneejointsurgery.com/ligament-injuries/posterolateral-corner/
Category: Pediatrics
Keywords: CT scans, radiation exposure, pediatrics (PubMed Search)
Posted: 7/21/2017 by Jenny Guyther, MD
(Updated: 2/2/2026)
Click here to contact Jenny Guyther, MD
Ventricular shunt (VP) malfunction can be severe and life-threatening and evaluation has typically included a dry CT brain and a shunt series which includes multiple x-rays of the skull, neck, chest and abdomen. The goal of this study was to decrease the amount of radiation used in the evaluation of these patients since these patients will likely present many times over their lifetime. Several institutions have more towards a rapid cranial MRI, however, this modality may not be readily available.
This multidisciplinary team decreased the CT scan radiation dose from 250mA (the reference mA in the pediatric protocol at this institution) to 150 mA which allows for a balance between reducing radiation exposure and adequate visualization of the ventricular system. They also added single view chest and abdominal x-rays.
The authors found that after implementing this new protocol, there was a reduction in CT radiation doses and number of x-rays ordered with no change in the return rate.
Marchese et al. Reduced Radiation in children presenting to the ED with Suspected Ventricular Shunt Complication. Pediatrics. 2017; 139 (5).
Category: Toxicology
Keywords: Vaginal pearls, intravaginal foreign bodies (PubMed Search)
Posted: 7/20/2017 by Kathy Prybys, MD
(Updated: 7/21/2017)
Click here to contact Kathy Prybys, MD
Vaginal douching is a common and potentially dangerous practice. Women engage in this practice predominately for personal hygiene reasons but also with the false belief it will prevent or treat infections and for contraception. Numerous public health agencies and medical societies discourage douching as it has been associated with many adverse outcomes including pelvic inflammatory disease, bacterial vaginosis, cervical cancer, low birth weight, preterm birth, human immunodeficiency virus transmission, sexually transmitted diseases, ectopic pregnancy, recurrent vulvovaginal candidiasis, and infertility.
An increasing fad is the use of intravaginal detox products. Claiming to enhance female health by removing toxins, these mesh cloth-covered balls containing herbs such as mothersworth, osthol, angelica, borneol, and rhizoma, not FDA-approved, are inserted into the vagina for 3 days. Clinical experience demonstrates these products decompose into numerous pieces which become scattered retained intravaginal foreign bodies, cause mucosal irritation, and thereotically could serve as a nidus for serious infections.

Category: Critical Care
Keywords: Resuscitation, CPR, family, policy (PubMed Search)
Posted: 7/17/2017 by Kami Windsor, MD
Click here to contact Kami Windsor, MD
When surveyed, half of general medicine patients interviewed stated that they would prefer to have a loved one present if they were to develop cardiac arrest and require CPR. So far, studies have demonstrated that…
Allowing family presence during CPR is associated with the following benefits to family members:
And is NOT associated with a difference in:
Several studies have demonstrated benefits to patient family members who are offered the opportunity to witness ongoing CPR when their loved one develops cardiac arrest. These benefits--decreased rates of PTSD-related symptoms, anxiety, depression (including need for medication, professional treatment, and suicide attempts), and complicated grief--have been shown to persist at 1 year post-resuscitation event.
Themes that arise when discussing the resuscitations with family members afterward include:
1. The feeling of active involvement in the resuscitation process
2. Communication with the resuscitation team
3. Perception of the reality of death
4. Experience of and reaction to witnessing (or not witnessing) the resuscitation
Twelve percent of family members who chose to NOT be present during CPR expressed regret at their choice, versus three percent of relatives who chose to be present.
Negative outcomes cited by family members who witnessed CPR involved feeling like they were not being communicated with, or that their loved one was being over-zealously resuscitated.
Category: Orthopedics
Keywords: nursemaid, elbow (PubMed Search)
Posted: 7/15/2017 by Michael Bond, MD
Click here to contact Michael Bond, MD
Take Home Points:
The Hyperpronation Method: This reduction technique for a nursemaid's elbow (radial head subluxation) has been found to have better first attempt success than classic supination/flexion technique and less painful. (Pediatrics July '98).
Click here to see a video of the technique https://youtu.be/-0ROu4hCXwQ?t=1m15s
Category: Toxicology
Keywords: hydrogen peroxide (PubMed Search)
Posted: 7/13/2017 by Hong Kim, MD
Click here to contact Hong Kim, MD
Hydrogen peroxide (H2O2) is a common household liquid that is used for wound irrigation/antiseptic and cosmetic purposes. The concentration of household product is 3% to 5% and is considered to be relatively safe except in large volume ingestion.
High-concentration H2O2 (>10%) is commercially available as “food grade” (35%) that is diluted for household use or for alternative medicine therapy (i.e. hyperoxygenation).
Ingestion of high-concentration of H2O2 can result in caustic injury as well as ischemic injury from gas embolism.
Ingestion of 1 mL of 3% H2O2 produces 10 mL of O2 gas while 1 mL of 35% H2O2 produces 115 mL of O2 gas.
Common symptoms/findings of H2O2 ingestions includes:
A retrospective review of >10% H2O2 ingestion from National Poison Data System showed:
Management
Hatten BW et al. Outcomes after high-concentration peroxide ingestions. Ann Emerg Med. 2017;69:726-736.
Category: Neurology
Keywords: Terson syndrome, vitreous hemorrhage, intraocular hemorrhage, subarachnoid hemorrhage (PubMed Search)
Posted: 7/12/2017 by WanTsu Wendy Chang, MD
Click here to contact WanTsu Wendy Chang, MD
50 YOF with acute onset of worst headache of life associated with nausea and vomiting. Patient is somnolent, will rouse to noxious stimuli and complains of a headache as well as decreased vision.
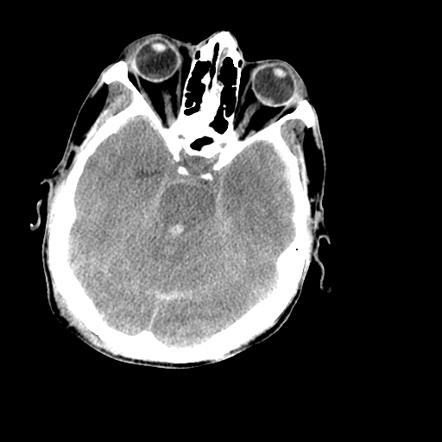
Image courtesy of Dr. Nasir Siddiqui, Radiopaedia.org. From the case rID: 36469
Follow me on Twitter @EM_NCC
Category: Orthopedics
Keywords: Hip, pediatrics, arthritis (PubMed Search)
Posted: 7/9/2017 by Brian Corwell, MD
Click here to contact Brian Corwell, MD
Idiopathic osteonecrosis of the femoral head
Children as young as 2 or as old as 12 but generally 4 to 8 (worse in older children)
Fare better than adults with osteonecrosis of femoral head
1 in 10,000
4-5x more common in males, much less common ini African Americans
Unilateral femoral head involvement 90% of the time (Bilateral 10% of the time)
Long term consequences are deformity and arthritis
Typical presentation: Subacute limping for weeks (Painless)
As activity worsens limp, it is maximal at the end of the day (Intermittent)
As in adults with hip pathology, IF pain is reported, it is located at the upper anterior thigh and groin
On examination, look for restriction in range of motion of the hip (compare with contralateral side)
May only present with mild to moderate decreased range of motion of the hip
30 versus 60 degrees for example
ABduct both legs with pelvis in neutral OR Place one hand on contralateral pelvis and ABduct affected leg with other hand.
Category: Toxicology
Keywords: Antidepressants (PubMed Search)
Posted: 7/7/2017 by Kathy Prybys, MD
Click here to contact Kathy Prybys, MD
Category: International EM
Keywords: Cholera, conflict, children (PubMed Search)
Posted: 7/5/2017 by Jon Mark Hirshon, MPH, MD, PhD
(Updated: 2/2/2026)
Click here to contact Jon Mark Hirshon, MPH, MD, PhD
Cholera is an acute diarrheal disease that can kill within hours if left untreated.
Rising cholera, diarrhea and malnutrition is a deadly combination in war torn countries, such as Yemen, South Sudan, Somalia and Sudan, especially for children.
Yemen currently has the worst outbreak globally, with over 260,000 suspected cases and over 1,600 deaths. In Yemen:
o Half the suspected cases are children
o A quarter of the deaths are among children
Bottom Line:
Cholera remains a major cause of morbidity and mortality globally, especially in areas of conflict.
http://www.who.int/mediacentre/factsheets/fs107/en/
http://www.un.org/apps/news/story.asp?NewsID=57114#.WV2aQ9Pyu9Y
Category: Geriatrics
Keywords: abuse, marks, interview (PubMed Search)
Posted: 7/3/2017 by Danya Khoujah, MBBS
Click here to contact Danya Khoujah, MBBS
When you are working up an elderly patient for trauma look for patterns such as circumferential bruising on the wrists that have the pattern of fingers the same way you would look at the injuries of a child. Remember that the person who is sitting next to them is frequently the person that is abusing them. Therefore, it is important to interview the patient alone.
Lachs MS, Pillemer KA. Elder Abuse. N Engl J Med 2015; 373:1947-1956
Category: Pharmacology & Therapeutics
Keywords: Levofloxacin, duration, dose, CAP, pneumonia (PubMed Search)
Posted: 7/1/2017 by Jill Logan
(Updated: 2/2/2026)
Click here to contact Jill Logan
When you look up dosing for levofloxacin for community acquired pneumonia (CAP), you will find that both of the following options are approved:
This is based on a multicenter, randomized, double-blind, active treatment trial comparing these two regimens in CAP (mild to severe). This non-inferiority trial shows that the 750 mg dose of levofloxacin for 5 days is "at least as effective and well tolerated" as the 500 mg dose of levofloxacin for 10 days.
So why should you choose the 750 mg daily x 5 day regimen?
As alway with levofloxacin, don't forget to renally dose adjust subsequent doses when writting a script or scheduled inpatient order for patients with reduced creatinine clearance!
Dunbar LM, Wunderink RG, Habib MP, et al. High-dose, short-course levofloxacin for community-acquired pneumonia: A new treatment paradigm. Clin Infect Dis. 2003;37:752-60.
Category: Toxicology
Keywords: Lactrodectus (PubMed Search)
Posted: 6/29/2017 by Kathy Prybys, MD
(Updated: 6/30/2017)
Click here to contact Kathy Prybys, MD
Black widow spiders belong to the genus Latro dectus which include 31 species of widow spiders found throughout world. Approximately 1500-2500 black widow bites are reported to American poison control centers annually. A black widow can be identified by their hourglass pattern (red or orange) on the ventral aspect of their shiny globular abdomen. Fortunately, envenomation is rare but when it does occur it causes severe pain, muscle cramping, abdominal (may mimic acute abdomen) often refractory to traditional analgesics and antivenom (Antivenin Latrodectus mactans) is available and effective . Alpha-latrotoxin is the potent toxin causing presynaptic cation channels to open (calcium) and release of neurotransmitters such acetycholine. The neurological signs and symptoms caused by predominantly autonomic and include tachycardia and hypertension. The antivenom is equine based and infused over 20-30 minutes with pain relief in 20 minutes.
Neurotoxic manifestations of black widow spider envenomation in pediatric patients. Sotelo-Cruz N, Gómez-Rivera N. Neurologia. 2016 May;31(4):215-22.
The Black Widow spider bite: differential, clinical manifestations, and treatment options. Shackleford R, Veillon D, Maxwell N, LaChance L, Jusino T, Cotelingam J, Carrington P. J La State Med Soc. 2015 Mar-Apr;167(2):74-8.
Category: Neurology
Keywords: autoimmune, cancer, encephalopathy (PubMed Search)
Posted: 6/28/2017 by Danya Khoujah, MBBS
Click here to contact Danya Khoujah, MBBS
Category: Critical Care
Keywords: CPR, ventilation, respiratory rate, PaCO2 (PubMed Search)
Posted: 6/27/2017 by Mike Winters, MBA, MD
Click here to contact Mike Winters, MBA, MD
Ventilation During Cardiopulmonary Resuscitation
Chang MP, Idris AH. The past, present, and future of ventilation during cardiopulmonary resuscitation. Curr Opin Crit Care 2017; 23:188-192.
Category: Orthopedics
Keywords: Adhesive Capsulitis (PubMed Search)
Posted: 6/24/2017 by Brian Corwell, MD
(Updated: 2/2/2026)
Click here to contact Brian Corwell, MD
Adhesive Capsulitis aka Frozen Shoulder
Spontaneous gradual onset stiffness and pain of the Glenohumeral joint
Shoulder capsule becomes thickened and contracted
Often affects patients between 40 and 60 years old
Left> Right shoulder
Women> men
Association with diabetes and thyroid disease
3 clinical stages
1) Pain – gradual onset, diffuse, severe, disabling, often worse at night
2) Stiffness – decreased ROM, affects ADLs, improved pain
3) Thawing – gradual return of motion
Physical examination: Painful and decreased ROM. Evaluate active and passive movement, external rotation and ABduction of the shoulder most affected
Surgical or post traumatic shoulder stiffness usually resolves within 12 months.
Adhesive capsulitis is generally self-limiting lasting an average of 18-36 months.
DDX: Chronic locked posterior shoulder dislocation (VERY IMPORTANT), tumor.
Treatment: NSAIDs, Physical therapy, Intra articular steroids
If this fails, manipulation under anesthesia and/or arthroscopic surgical release
Category: Pediatrics
Keywords: overdose, poisoning, veterinary medications (PubMed Search)
Posted: 6/24/2017 by Mimi Lu, MD
Click here to contact Mimi Lu, MD
Every year in the U.S., preventable poisonings in children result in more than 60,000 ED visits and around 1 million calls to poison centers. Calls relating specifically to pet medication exposure and children have been on the rise.
A recent study in Pediatrics was the first was kind to characterize the epidemiology of such exposures.
This study is a call to arms for an increased effort on the part of public health officials, pharmacists, veterinarians, and physicians to improve patient education to prevent these exposures from occurring.
Summary of major findings:
Most commonly Implicated exposures:
Key contributors to exposure risk:
Take home point: Make sure your pet's medications are appropriately stored for safety!
Methods involved reviewing regional Poison Control Center data from 1999 thruh 2013, during which 1431 calls regarding exposures of children less than or equal to age 19 or exposed to a veterinary medication.
While the authors concluded that most exposures did not result in major adverse outcomes, 14.1% of exposures resulted in at least minor health effects.
A broader range of more highly toxic medications are increasingly being prescribed for animals, including anti-neoplastic drugs such as cyclophosphamide and chlorambucil.
Treatment of chronic health conditions and pets, such as osteoarthritis, hypothyroidism, or anxiety is also increasingly common.
Tomasi S, Roberts KJ, Stull J, Spiller HA, McKenzie LB. Pediatric Exposures to Veterinary Pharmaceuticals. Pediatrics. 2017;139(3)
Category: Pediatrics
Keywords: Blunt thoracic trauma, pediatric trauma, chest xray (PubMed Search)
Posted: 6/16/2017 by Jenny Guyther, MD
Click here to contact Jenny Guyther, MD
Chest injuries represent the second most common cause of pediatric trauma related death. ATLS guidelines recommend CXR in all blunt trauma patients. Previous studies have suggested a low risk of occult intrathoracic trauma; however, these studies included many children who were sent home.
Predictors of thoracic injury include: abdominal signs or symptoms (OR 7.7), thoracic signs of symptoms (OR 6), abnormal chest auscultation (OR 3.5), oxygen saturation < 95% (OR 3.1), BP < 5% for age (OR 3.7), and femur fracture (OR 2.5).
4.3 % of those found to have thoracic injuries did not have any of the above predictors, but their injuries were diagnosed on CXR. These children did not require trauma related interventions.
Bottom line: There were still a number of children without these predictors that had thoracic injuries, so the authors suggest that chest xray should remain a part of pediatric trauma resuscitation.
This was a retrospective review of children aged 0-17 with blunt trauma requiring trauma team activation who had a chest xray preformed. 483 eligible children were included, all of whom were admitted to the hospital. 108 children had their thoracic injury detected on chest xray, 110 on chest CT and 76 on abdominal CT. Pneumothorax, pulmonary contusion and multiple rib fractures were the most commonly found thoracic injuries. All children also had other injuries.
Weerdenburg et al. Predicting Thoracic Injury in Children with Multi-trauma. Pediatric Emergency Care. Epub ahead of print. 2017.
Category: Toxicology
Keywords: drugs of abuse, street name (PubMed Search)
Posted: 6/5/2017 by Hong Kim, MD
(Updated: 6/15/2017)
Click here to contact Hong Kim, MD
Street names for illicit substance are diverse and unique. Knowing what your patient used prior to ED presentation can help with the management of their intoxication.
DEA recently released 7 page list of common street names for drugs of abuse.
https://ndews.umd.edu/sites/ndews.umd.edu/files/dea-drug-slang-code-words-may2017.pdf
But keep in mind that what our patients purchase and use may not actually contain the drug that they intended to purchase (e.g. fentanyl being sold as heroin).
