Category: International EM
Keywords: Opioids, overdose, injury, death (PubMed Search)
Posted: 1/18/2017 by Jon Mark Hirshon, MPH, MD, PhD
Click here to contact Jon Mark Hirshon, MPH, MD, PhD
· Opioid deaths, such as from heroin and prescription opioids, are a major problem globally
· In the U.S., since 1999 overdose deaths from prescription opioids have quadrupled.
o Almost half of opioid deaths involve a prescription opioid
· The most common drugs related to prescription opioid deaths are:
o Methadone
o Oxycodone
o Hydrocodone
https://www.cdc.gov/drugoverdose/data/overdose.html
Category: Critical Care
Keywords: Arterial Line, Ultrasound (PubMed Search)
Posted: 1/17/2017 by Rory Spiegel, MD
(Updated: 2/2/2026)
Click here to contact Rory Spiegel, MD
It is not uncommon for critically ill patients to require invasive monitoring of their blood pressure. In these patients, radial arterial lines are often inserted. Traditionally these lines are placed using palpation of the radial pulse. This technique can lead to unacceptably high failure rate in the hypotensive patient commonly encountered in the Emergency Department.
A recent meta-analysis by Gu et al demonstrated the use of dynamic US to assist in the placement of radial arterial lines decreased the rate of first attempt failure, time to line insertion and the number of adverse events associated with insertion.
Gu WJ, Wu XD, Wang F, Ma ZL, Gu XP. Ultrasound Guidance Facilitates Radial Artery Catheterization: A Meta-analysis with Trial Sequential Analysis of Randomized Controlled Trials. Chest. 2016;149(1):166-79.
Category: Orthopedics
Keywords: Airway, wheezing, exercise (PubMed Search)
Posted: 1/14/2017 by Brian Corwell, MD
(Updated: 6/26/2021)
Click here to contact Brian Corwell, MD
You are covering a sporting event or working an ED shift when a young adolescent athlete without significant PMH presents with SOB and wheezing associated with exercise.
You immediately think exercise-induced asthma, prescribe a short-acting bronchodilator and pat yourself on the back.
While you may be right, there is increasing recognition of an alternative diagnosis
Exercise-induced laryngeal obstruction (EILO)
During high intensity exercise, the larynx can partially close, thereby causing a reduction in normal airflow. This results in the reported symptoms of SOB and wheezing.
This diagnosis has previously been called exercise induced vocal cord dysfunction. As the narrowing most frequently occurs ABOVE the level of the vocal cord, EILO is a more correct term.
While exercise induced bronchoconstriction has a prevalence of 5-20%, EILO is less common with a prevalence of 5-6%.
Patients are typically adolescents, with exercise associated wheezing and SOB, frequently during competitive or very strenuous events. Wheezing is inspiratory and high-pitched. Symptoms are unlikely to be present at time of medical contact unless you are at the event as resolution occurs within 5 minutes though associated cough or throat discomfort can persist after exercise cessation. EIB symptoms typically last up to 30 minutes following exercise.
Inhaler therapy is unlikely to help though some athletes report subjective partial relief. This may be explained as approximately 10% of individuals have both EIB and EILO.
In athletes with respiratory symptoms referred to asthma clinic, EILO was found in 35%.
Consider EILO in athletes with unexplained respiratory symptoms especially in those with ongoing symptoms despite appropriate therapy for EIB.
Category: Toxicology
Keywords: salicylate poisoning (PubMed Search)
Posted: 1/13/2017 by Hong Kim, MD
(Updated: 2/2/2026)
Click here to contact Hong Kim, MD
A small retrospective study of an acute poisoning cohort attempted to identify risk factors for severe outcome in salicylate poisoning.
Severe outcomes were defined as
A multivariate analysis of 48 patients showed that older age and increased respiratory rate were independent predictors of severe outcomes when adjusted for salicylate level.
Initial salicylate acid level was not predictive of severe outcome.
Elevated lactic acid level was also a good predictor of severe outcome in univariate analysis but not in multivariate analysis.
Limitations
Bottom line
Shively RM et al. Acute salicylate poisoning: risk factors for sever outcome. Clin Toxicol 2017 Jan 9:1-6. doi: 10.1080/15563650.2016.1271127. [Epub ahead of print]
Category: Neurology
Keywords: concussion, driving performance, cognitive impairment (PubMed Search)
Posted: 1/11/2017 by WanTsu Wendy Chang, MD
Click here to contact WanTsu Wendy Chang, MD
Schmidt JD, Hoffman NL, Ranchet M, et al. Driving after concussion: Is it safe to drive after symptoms resolve? J Neurotrauma. 2016 Dec 13. [Epub ahead of print]
Follow me on Twitter @EM_NCC
Category: Critical Care
Keywords: Sepsis, Antibiotics, Septic Shock (PubMed Search)
Posted: 1/10/2017 by Daniel Haase, MD
(Updated: 2/18/2017)
Click here to contact Daniel Haase, MD
--Recent meta-analysis comparing continuous infusion versus intermittent bolus dosing of beta-lactam antibiotics demonstrates mortality benefit (NNT = 15) in patients with severe sepsis or septic shock. (1)
--Consider beta-lactam continuous infusion on your septic patients if your hospital pharmacy allows
[Thanks to Anne Weichold, CRNP for providing the article for this pearl!]
--Beta-Lactams are time-dependent antibiotics (i.e. longer time above MIC = more time killing) annd continuous infusions should have concentrations consistently above MIC.
--Previous studies not powered to demonstrate mortality benefit, but showed pharmocokinetic improvement and higher rates of clinical cure (2)
Pratical aspects
This means the patient will require an additional IV most of the time
Most hospitals do not have a pharmacy protocol for infusion of most extended-spectrum B-lactams
1. Roberts JA, Abdul-Aziz MH, Davis JS, et al. Continuous versus Intermittent B-Lactam Infusion in Severe Sepsis. Am J Resp Crit Care Med. 2016; 194 (6): 681-91.
2. Abdul-Aziz MH, Sulaiman H, Mat-Nor MB, et al. Beta-Lactam Infusion in Severe Sepsis (BLISS): a prospective, two-centre, open-labelled randomised controlled trial of continuous versus intermittent beta-lactam infusion in critically ill patients with severe sepsis. Intensive Care Med. 2016; 42 (10) 1535-45.
Category: Visual Diagnosis
Posted: 1/9/2017 by Tu Carol Nguyen, DO
Click here to contact Tu Carol Nguyen, DO
A 60 year-old man with history of atrial fibrillation, CAD presents with left lower leg/foot pain for a few days. His foot is seen below. What's the diagnosis?


Mottling with concerns for Acute Limb Ischemia
Key Points:
Creager MA, Kaufman JA, Conte MS. Clinical practice. Acute limb ischemia. N Engl J Med. 2012;366(23):2198-206.
http://www.emdocs.net/acute-limb-ischemia-pearls-pitfalls/
Category: Pharmacology & Therapeutics
Keywords: ketorolac, NSAID, analgesia (PubMed Search)
Posted: 1/7/2017 by Michelle Hines, PharmD
(Updated: 2/2/2026)
Click here to contact Michelle Hines, PharmD
In a study comparing ketorolac IV doses of 10 mg, 15 mg, and 30 mg, no difference in pain score reduction or need for rescue analgesia was observed.
Based upon this study, lower ketorolac doses of 10 mg or 15 mg are equal in analgesic efficacy to a higher dose of 30 mg. A lower dose of 10 mg or 15 mg should be used to avoid adverse effects.
Motov S, Yasavolian M, Likourezos A, et al. Comparison of intravenous ketorolac at three single-dose regimens for treating acute pain in the emergency department: a randomized controlled trial. Ann Emerg Med 2016. PMID 27993418
Follow me on Twitter @mEDPharmD
Category: Toxicology
Keywords: Lactic acidosis (PubMed Search)
Posted: 1/5/2017 by Kathy Prybys, MD
(Updated: 1/6/2017)
Click here to contact Kathy Prybys, MD
Lactic acidosis is the most common cause of anion gap metabolic acidosis in all hospitalized patients. An elevated lactate level is an important marker of inadequate tissue perfusion causing subsequent shift to anaerobic metabolism and occuring in a variety of disease states such as sepsis. In patients with unexplained lactic acidosis without systemic hyoperfusion or seizure suspect the following toxins:
Understanding lactic acidosis in paracetamol (acetaminophen) poisoning. Shah, AD, Wood DM, et al. British Journal of Clinical Pharmacology 2011.71: 20–28.
Value of lactic acidosis in the assessment of the severity of acute cyanide poisoning. Baud FJ, et al. Crit Care Med. 2002;30(9):2044-50.
The Importance of the osmolality gap in ethylene glycol intoxication. Oostvogels R, et al. BMJ 2013 Dec 7;347:31-33.
Can Acute overdose metformin lead to lactic acidosis? Wilis BK, et al. Amer J Emerg Med. 2010;28:857.
Bench to bedside review: Severe lactic acidosis in HIV patients treated with nucleoside analogue reverse transcriptase inhibitors. Classens Y-E, et al. Critical Care. 2003;7(3):226-232.
A case of Kombucha Teas Toxicity. Kole A SH, Jones HD, et al. J Intensive care Med.2009:24(3) 205-7.
Category: International EM
Keywords: B12 deficiency, ataxia, dementia, pernicious anemia (PubMed Search)
Posted: 1/4/2017 by Jon Mark Hirshon, MPH, MD, PhD
Click here to contact Jon Mark Hirshon, MPH, MD, PhD
Vitamin B12 deficiency can cause significant disease, including severe neurologic problems. However, patient presentations can vary greatly.
Signs and symptoms can include:
Prolonged B12 deficiency can lead to significant neurologic complications, frequently related to the spinal cord, and can include:
Category: Critical Care
Posted: 1/3/2017 by Mike Winters, MBA, MD
Click here to contact Mike Winters, MBA, MD
PaCO2 and the Post-Arrest Patient
McKenzie N, et al. A systematic review and meta-analysis of the association between arterial carbon dioxide tension and outcomes after cardiac arrest. Resuscitation 2017; 111:116-126.
Category: Visual Diagnosis
Posted: 1/2/2017 by Hussain Alhashem, MBBS
Click here to contact Hussain Alhashem, MBBS
A 36-year-old male, who recently immigrated from Africa, presented to the ED with fever, rash, cough and shortness of breath. He was noted to be febrile to 39.0 C. The rash is disseminated but present mainly in his trunk as shown in the picture.

Disseminated Varicella Zoster Virus (VZV) Infection
- The patient is presenting with a rash in different stages, associated with fever and signs of systematic involvement, indicating a disseminated varicella infection.
- Definitive diagnosis of disseminated VZV infection is made by detecting its DNA in multiple anatomic sites.
- The most common complication of VZV infection in immunocompetent adults is VZV pneumonia. Early detection of VZV pneumonia can be done with bronchoalveolar lavage and PCR testing.
- Treatment is with IV acyclovir and is more effective if started within 24 hours of the beginning of symptoms. In cases that require prolonged treatment, gene sequencing should be done to detect resistant strains.
Beby?Defaux, Agnès, et al. "Disseminated varicella with multiorgan failure in an immunocompetent adult." Journal of medical virology 81.4 (2009): 747-749.
Category: Orthopedics
Keywords: DVT, Leg, Cast (PubMed Search)
Posted: 12/31/2016 by Michael Bond, MD
Click here to contact Michael Bond, MD
Take Home Point:
Low-molecular-weight heparin doesn't seem to prevent symptomatic venous thromboembolism (VTE) in patients undergoing knee arthroscopy or lower leg casting, suggest two trials in the New England Journal of Medicine.
The study was conducted by Dutch researcheers and randomized 1500 patients who underwent lower leg casting or knee arthoscopy to receive no anticoagulation or low molecular weight heparin. Patients were either treated for the entire duration of immobilzation or 8 days after their surgery (arthroscopy patients)
The rates of VTE in patients at 3 months of follow up where arthroscopy: 0.7% vs. 0.4%; casting: 1.4% vs. 1.8%. So overall very low rates of VTE, and no real difference between the groups.
A large cohort might have shown some benefit, but since the incidence is so low there is probably no reason to prophlactically treat these patients and increase their risk of major bleeding events, which was also low in the study.
The article can be found at http://www.nejm.org/doi/full/10.1056/NEJMoa1613303?query=pfw&jwd=000100949960&jspc=EM
van Adrichem RA, Nemeth B, Algra A, le Cessie S, Rosendaal FR, Schipper IB, et al. Thromboprophylaxis after Knee Arthroscopy and Lower-Leg Casting. N Engl J Med 2016.
Category: Pediatrics
Posted: 12/31/2016 by Mimi Lu, MD
Click here to contact Mimi Lu, MD
In pediatrics, providers typically prescribe 10 mg/kg (max 500 mg) and 5 mg/kg daily x 4 (max 250 mg) for treatment of pneumonia, but this dosing regimen is NOT recommended for all azithromycin usage. There are other dosing regimens that are important to keep in mind during the respiratory season:
1) Pharyngitis/ tonsillitis (ages 2-15 yr): 12 mg/kg daily x 5 days (max 500 mg/ 24 hr)
2) Pertussis
3) Acute sinusitis >/= 6 months: 10 mg/kg daily x 3 days
Tschudy MM, Arcara KM. The Harriet Lane Handbook 19th edition. Elsevier Mosby; 2012
Category: Toxicology
Keywords: cyanide toxicity, lactic acid (PubMed Search)
Posted: 12/29/2016 by Hong Kim, MD
(Updated: 12/30/2016)
Click here to contact Hong Kim, MD
Smoke inhalation victims (house fires) are at risk of carbon monoxide (CO) and cyanide poisoning (CN). CO exposure/poisoning can be readily evaluated by CO - Oximetry but CN level can be obtained in majority of the hospital.
Lactic acid level is often sent to evaluate for CN poisoning.
Bottom line:
In a manuscript published in 1991, N Engl J Med by Dr. FJ Baud is the source of this data.
CN blood levels were measured in 109 residetial fire victims in France prior to any treatment was initiated.
Baud FJ et al. Elevated blood cyanide concentrations in victims of smoke inhalation. N Engl J Med 1991;325:1761-6.
Category: Critical Care
Keywords: Acute pulmonary edema, Bolus nitrates (PubMed Search)
Posted: 12/27/2016 by Rory Spiegel, MD
(Updated: 2/2/2026)
Click here to contact Rory Spiegel, MD
It is well known that the early aggressive utilization of IV nitrates and non-invasive positive pressure ventilation (NIV) in patients presenting with acute pulmonary edema will decrease the number of patients requiring endotracheal intubation and mechanical ventilation.
Often our tepid dosing of nitroglycerine is to blame for treatment failure. Multiple studies have demonstrated the advantages of bolus dose nitroglycerine in the early management of patients with acute pulmonary edema. In these cohorts, patients bolused with impressively high doses of IV nitrates every 5 minutes, are intuabted less frequently than patients who received a standard infusion (1,2). No concerning drops in blood pressure in the patients who received bolus doses of nitrates were observed. Using the standard 200 micrograms/ml nitroglycerine concentration, blood pressure can be rapidly titrated to effect.
1. Cotter G, Metzkor E, Kaluski E, et al. Randomised trial of high-dose isosorbide dinitrate plus low-dose furosemide versus high-dose furosemide plus low-dose isosorbide dinitrate in severe pulmonary oedema. Lancet. 1998;351(9100):389-93.
2. Levy P, Compton S, Welch R, et al. Treatment of severe decompensated heart failure with high-dose intravenous nitroglycerin: a feasibility and outcome analysis. Ann Emerg Med. 2007;50(2):144-52
Category: Visual Diagnosis
Posted: 12/27/2016 by Tu Carol Nguyen, DO
Click here to contact Tu Carol Nguyen, DO
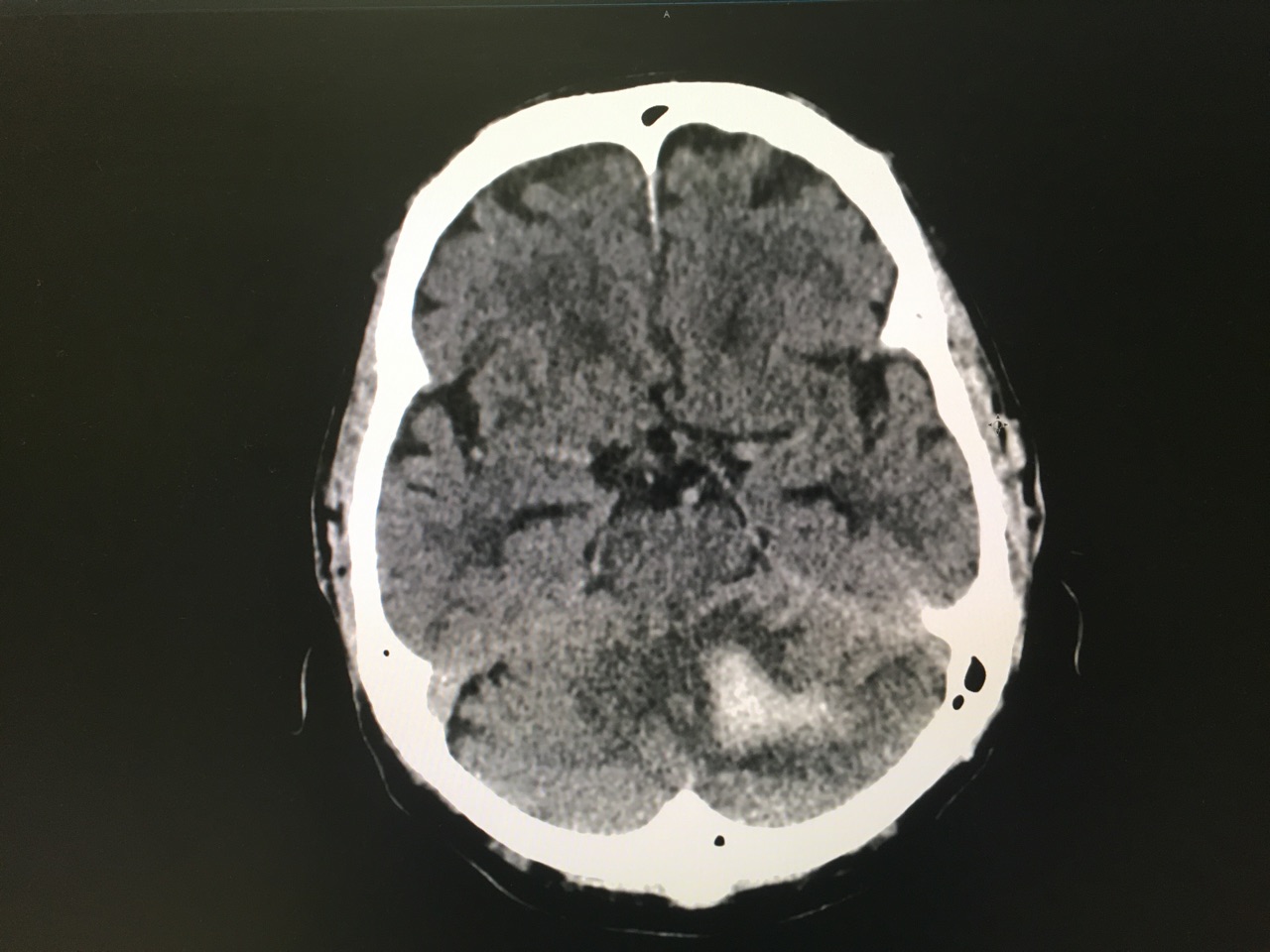
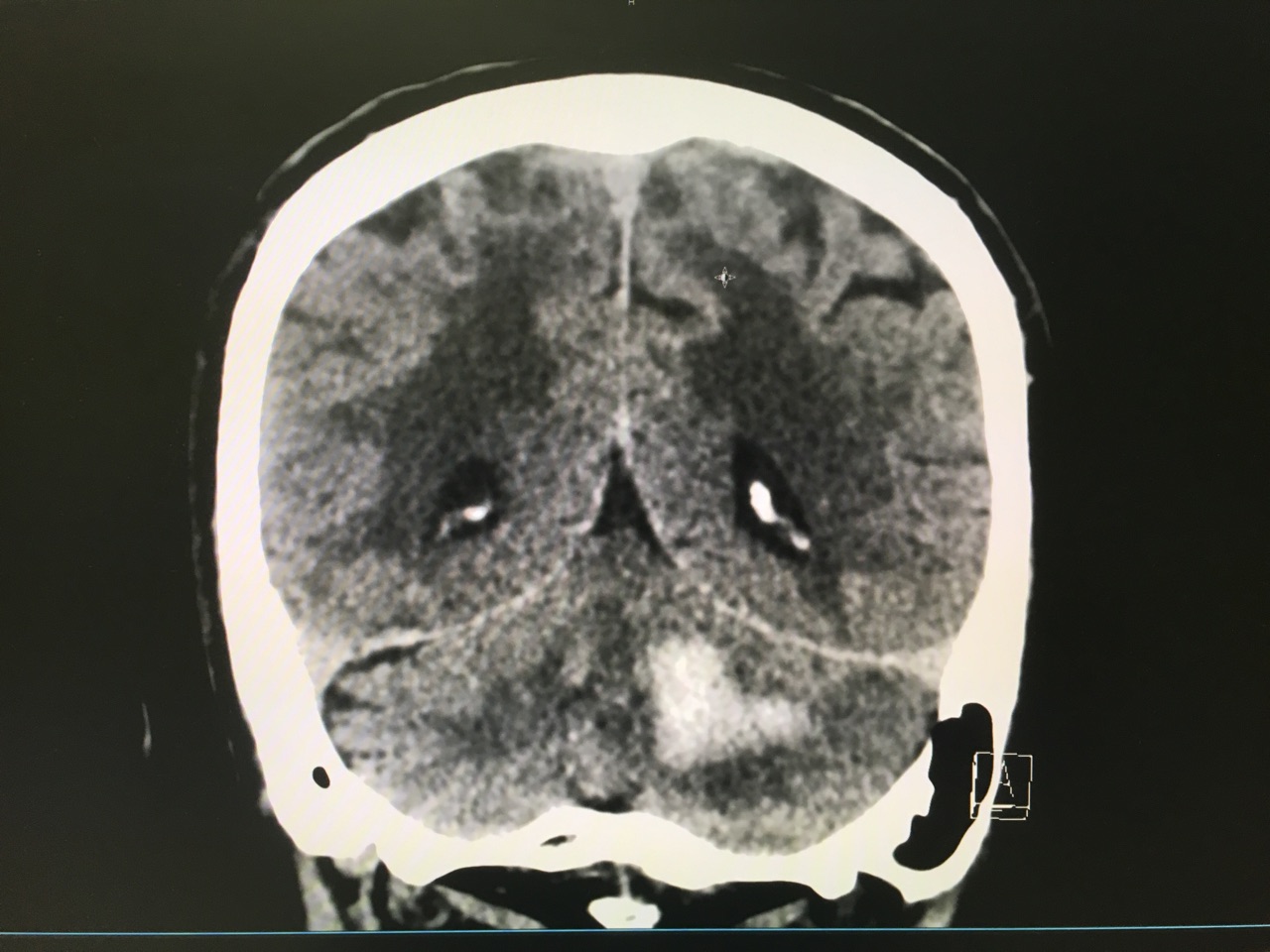
Answer: Large left cerebellar intraparenchymal hemorrhage with surrounding vasogenic edema with mild infratentorial midline shift of ~4mm
Take Home Points:
Hemphill JC, Greenberg SM, Anderson CS, et al. Guidelines for the Management of Spontaneous Intracerebral Hemorrhage: A Guideline for Healthcare Professionals From the American Heart Association/American Stroke Association. Stroke. 2015;46(7):2032-60.
Category: Orthopedics
Keywords: Concussions, musculoskeletal injury (PubMed Search)
Posted: 12/24/2016 by Brian Corwell, MD
Click here to contact Brian Corwell, MD
Significant associations were found between concussion and
Lateral ankle sprain (P = 0.012)
Knee injury (P = 0.002)
Lower extremity muscle injury (P = 0.031)
Keep in mind that 50 – 80% of concussions may go undiagnosed or unreported.
A discussion about risks of early return after concussion should include mention of risks beyond repeat head injury/2nd impact syndrome
Study limits: Retrospective design limits ability to establish causation/reporting bias
Gilbert, Burdette, et al., 2016 Association between concussion and lower extremity injuries in collegiate athletes. Sports Health 8 (6), 561-567.
Category: International EM
Keywords: Vitamin B12, pernicious anemia (PubMed Search)
Posted: 12/21/2016 by Jon Mark Hirshon, MPH, MD, PhD
Click here to contact Jon Mark Hirshon, MPH, MD, PhD
Vitamin B12 deficiency, including pernicious anemia, is typically seen in malnourished individuals. Globally, it is widespread in those who live in poverty.
In the U.S., we often consider it in individuals who are chronic alcoholics. However, it can be seen in others, including:
Category: Critical Care
Keywords: Intracranial hemorrhage, ICH, PCC, FFP, vitamin K antagonist, VKA, coumadin, warfarin (PubMed Search)
Posted: 12/20/2016 by Daniel Haase, MD
(Updated: 2/18/2017)
Click here to contact Daniel Haase, MD
The Neurocritical Care Society and Society of Critical Care Medicine just came out with new Guidelines for Reversal of Antithrombotics in Intracranial Hemorrhage (ICH) [1]
--PCC is now recommended over FFP in reversal of vitamin K antagonists (VKA) with elevated INR. Either should be co-administered with 10mg IV vitamin K. (Strong recommendation, moderate quality evidence)
TAKE AWAY: PCC should be probably be given over FFP in VKA-ICH when available
--Seems to be primarily based on a recent Lancet trial, which was stopped early due to safety concerns [2], but demonstrated more rapid reversal of INR and less hematoma expansion.
--In that study, all hematoma expansion related deaths occurred in the FFP group.
--Study was not designed to look at 90 day outcome, but trended towards improved survival.
1. Guideline for Reversal of Antithrombotics in Intracranial Hemorrhage: Executive Summary. A Statement for Healthcare Professionals From the Neurocritical Care Society and the Society of Critical Care Medicine. Frontera JA, Lewin JJ 3rd, et al. Crit Care Med. 2016 Dec;44(12):2251-2257.
2. Fresh frozen plasma versus prothrombin complex concentrate in patients with intracranial haemorrhage related to vitamin K antagonists (INCH): a randomised trial. Steiner T, Poli S, et al. Lancet Neurol. 2016 May;15(6):566-73.
