Category: Critical Care
Posted: 3/2/2010 by Mike Winters, MBA, MD
(Updated: 2/3/2026)
Click here to contact Mike Winters, MBA, MD
Ventilating the Patient with Traumatic Brain Injury
Young N, Rhodes JKJ, Mascia L, Andrews PJD. Ventilatory strategies for patients with acute brain injury. Curr Opin Crit Care 2010; 16:45-52
Category: Pediatrics
Posted: 2/27/2010 by Rose Chasm, MD
(Updated: 3/6/2010)
Click here to contact Rose Chasm, MD
Category: Orthopedics
Keywords: Segond Fracture (PubMed Search)
Posted: 2/27/2010 by Michael Bond, MD
(Updated: 2/3/2026)
Click here to contact Michael Bond, MD
The Segond Fracture:
An benign appearing avulsion fracture of the lateral tibeal plateau that is marker for more significant injuries such as:
If this avulsion fracture is seen consider immobilzing the patients knee until they can follow up with Orthopedics and/or get an MRI to determine if additional injuries are present.

Category: Pediatrics
Keywords: Pediatrics, Sedation (PubMed Search)
Posted: 2/27/2010 by Reginald Brown, MD
(Updated: 2/3/2026)
Click here to contact Reginald Brown, MD
Precedex (Dexmedetomidine) - Great for pediatric imaging procedures
Alpha-2 agonist with sedative properties
No analgesic effect alone, but shown to decrease the amount of opioids required for a painful procedure
Benefits pts go to sleep and awake in a more natural state. Caregivers tend to prefer this as opposed to other sedatives. Short recovery time- about 30 minutes
Adverse effects include bradycardia and hypotension. Not recommended in any child with cardiac abnormalities. Paradoxical hypertension with loading dose has also been observed
Effective for MRI or CT scans at loading doses of 2mcg/kg over ten minutes, then maintenance of 1mcg/kg/hr
Residents can gain experience with Precedex with Peds sedation on M,W,F mornings with sedation team, contact me to arrange a time for you to participate.
Category: Neurology
Keywords: ABCD, ABCD2, California Rule, stroke, TIA, prediction tool (PubMed Search)
Posted: 2/24/2010 by Aisha Liferidge, MD
(Updated: 2/3/2026)
Click here to contact Aisha Liferidge, MD
Category: Critical Care
Posted: 2/22/2010 by Evadne Marcolini, MD
(Updated: 2/23/2010)
Click here to contact Evadne Marcolini, MD
The question of hyperglycemia in the critically ill and how to address it has been the topic of considerable study over the years.
There have been several attempts to try to quantify the best target glucose levels in critically ill patients. This is still a moving target, but a recent study sheds some light on the effect of different levels of hyperglycemia and the types of patients who are particularly vulnerable.
This is a retrospective cohort study whic reviewed 259,000 ICU admissions over a three year period at 173 separate sites. Their findings were as follows:
Compared with normoglycemic patients, the adjusted odds for mean glucose 111-145, 146-199, 200-300, and >300 was 1.31, 1.82, 2.13 and 2.85 respectively.
There is a clear association between the adjusted odds of mortality related to hyperglycemia in patients with AMI, arrhythmia, unstable angina, pulmonary embolism, pneumonia and gastrointestinal bleed.
Hyperglycemia associated with increased mortality was independent of type of ICU, length of stay and/or pre-existing diabetes.
So, even though we have not come to solid conclusions about how far down to keep the glucose levels down, it makes sense to pay particular attention and be more vigilant of the blood glucose levels, especially in the higher-risk patients listed above.
Flaciglia M, Freyberg RW et al: Hyperglycemia-related mortality in critically ill patients varies with admission diagnosis. Crit Care Med 2009;37:3001-3009
Category: Vascular
Keywords: Aortic Dissection (PubMed Search)
Posted: 2/22/2010 by Rob Rogers, MD
(Updated: 2/3/2026)
Click here to contact Rob Rogers, MD
Suspect your patient has an aortic dissection? Don't wait to lower the blood pressure.
A few considerations for the patient with suspected aortic dissection:
Category: Cardiology
Keywords: herbal, warfarin, adverse drug effects, drug effects, drug side effects, bleeding (PubMed Search)
Posted: 2/21/2010 by Amal Mattu, MD
(Updated: 2/3/2026)
Click here to contact Amal Mattu, MD
Many cardiac patients take warfarin...no surprise.
Many patients use herbal supplements...no surprise.
Many herbal supplements can produce increased bleeding risk with warfarin, and some produce decreased effects of warfarin...that may be a bit of a surprise. Here's a few that are worth knowing:
Herbals that increase the bleeding risk of warfarin: alfalfa, angelica (dong quai), bilberry, fenugreek, garlic, ginger, and ginkgo
Herbals that decrease the effect of warfarin: ginseng, green tea
In addition to asking your patients about their prescription medications, specifically ask your patients if they take herbal supplements, over-the-counter products, or green tea (since many patients don't consider green tea to be either an herbal supplement)...especially if the patient takes warfarin. You just might diagnose or prevent a disastrous bleeding complication.
[Tachjian A, Maria V, Jahangir A. Use of herbal products and potential interactions in patients with cardiovascular diseases. J Am Coll Cardiol 2010;55:515-525.]
Category: Orthopedics
Keywords: Spine, Fracture, Diagnosis (PubMed Search)
Posted: 2/20/2010 by Michael Bond, MD
Click here to contact Michael Bond, MD
A recent study by Smith et al showed that the general abdomen/pelvic CT scan in trauma patients obtained with 5mm slices is a better screening test for spine fractures than plain films. They also showed that when compared to dedicated reconstructed thoracolumbar CT scan (2mm slices focused on the spine) it did not miss any clinically significant fractures.
The statistic for plain radiographs and the nonreconstructive CT scan are shown below.
| | Plain Radiographs | Nonreconstructive CT Scan | ||
| | Lumbar | Thoracic | Lumbar | Thoracic |
| Sensitivity % [95% CI] | 47 [33 to 62] | 13 [3 to 32] | 94 [83 to 99] | 73 [50 to 89] |
| Specificity % [95% CI] | 91 [78 to 97] | 71 [54 to 85] | 95 [85 to 99] | 94 [79 to 99] |
| Positive Predictive Value % [95% CI] | 85 [66 to 96] | 15 [2 to 45] | 95 [86 to 99] | 89 [67 to 99] |
| Negative Predictive Value % [95% CI] | 61 [48 to 72] | 56 [41 to 71] | 93 [82 to 99] | 83 [66 to 93] |
The take home point is that dedicated Spine CT scans are probably not needed unless they are going to be used to guide surgical or non-surgical management, and plain films should probably be abandoned in patients that are undergoing CT scans of the chest/abdomen/pelvis.
Smith MW, Reed JD, Facco R, Hlaing T, McGee A, Hicks BM, Aaland M: The reliability of nonreconstructed computerized tomographic scans of the abdomen and pelvis in detecting thoracolumbar spine injuries in blunt trauma patients with altered mental status. J Bone Joint Surg Am 2009; 91: 2342-2349.
Category: Toxicology
Keywords: cholecalciferol, brodifacoum (PubMed Search)
Posted: 2/18/2010 by Fermin Barrueto
(Updated: 2/3/2026)
Click here to contact Fermin Barrueto
When a child is reported to be exposed to a rat poison it is commonly a long acting coumarin like brodifacoum. The rat usually eats the poison then during its traumatic little life will cause its own death by jumping and squeezing through a crack. When a human is exposed, this is the typical sequence of events:
Treatment is the same as for coumadin, vitamin K. However, do not start empirically since the patient will be committed to high doses of vitamin K for several months. Let the patient prove they have been poisoned which means they will require recheck of their INR 2-3 days later though they can be sent home with specific warning signs of anticoagulation.
Category: Neurology
Keywords: seizure, new-onset seizure, AIDS, HIV, HIV/AIDS (PubMed Search)
Posted: 2/17/2010 by Aisha Liferidge, MD
Click here to contact Aisha Liferidge, MD
Category: Vascular
Posted: 2/15/2010 by Rob Rogers, MD
(Updated: 2/3/2026)
Click here to contact Rob Rogers, MD
Bleeding Dialysis Fistula?
Ever see a patient in the ED c/o "my fistula won't stop bleeding"? If you haven't, you probably will in the future.
Here are some helpful tips on getting these bad boys to stop oozing:
Category: Orthopedics
Posted: 2/14/2010 by Michael Bond, MD
Click here to contact Michael Bond, MD
Impingement Syndrome and the Diagnostic Accuracy of 5 Common Tests
It is also reported that subacromial impingement syndrome (SAIS) is the more frequent cause of shoulder pain.
The authors of this study attempted to determine the diagnostic accuracy of the following 5 tests for SAIS:
The study demonstrated that any 3 positive tests out of the 5 has a sensitivity of 0.75 (0.54-0.96) , specificity of 0.74 (0.61-0.88), positive likelihood ratio of 2.93 (1.60-5.36) and negative likelihood ratio of 0.34 (0.14-0.80). See the table below for the individual test characteristics. No single test was deemed accurate enough to make the diagnosis by itself.
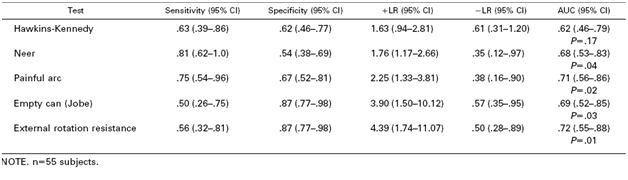
So in the end you should be familiar with most of these tests in order to use a combination of them to make the diagnosis of impingement syndrome. Future pearls will review how to perform these tests.
Michener LA, Walsworth MK, Doukas WC, Murphy KP: Reliability and diagnostic accuracy of 5 physical examination tests and combination of tests for subacromial impingement. Arch Phys Med Rehabil 2009; 90: 1898-1903.
Category: Neurology
Keywords: frostbite, neuropathy, hyperbaric oxygen (PubMed Search)
Posted: 2/11/2010 by Aisha Liferidge, MD
(Updated: 2/3/2026)
Click here to contact Aisha Liferidge, MD
Category: Toxicology
Keywords: transplant, tacrolimus, sirolimus, cyclosporine (PubMed Search)
Posted: 2/9/2010 by Bryan Hayes, PharmD
(Updated: 2/11/2010)
Click here to contact Bryan Hayes, PharmD
With all of the post-transplant patients we see in the ED, a refresher on the toxicities associated with the most common immunosuppressant medications is warranted.
Cyclosporine (Sandimmune® and Neoral®/Gengraf®) and tacrolimus (Prograf®) are both calcineurin inhibitors that inhibit activation and proliferation of T-lymphocytes and IL-2.
- Major concerns: Nephrotoxicity, drug interactions (CYP3A4)
- Adverse Effects:
o Electrolyte abnormalities: K+, ¯Mg+, glucose
o CNS: HA, tremor (statistically higher with tacrolimus)
o CV: HTN, lipids (increased with cyclosporine)
o End organ: hepatotoxicity, nephrotoxicity
o Cosmetic (cyclosporine specific): hirsutism, gingival hyperplasia, acne
Sirolimus/Rapamycin (Rapamune®) is an M-tor inhibitor that inhibits T-lymphocyte activation and proliferation.
- Major concerns: Drug interactions (CYP3A4)
- Adverse Effects:
o Delayed wound healing
o Leucopenia, thrombocytopenia
o Hypercholesterolemia
Category: Critical Care
Posted: 2/3/2010 by Evadne Marcolini, MD
(Updated: 2/3/2026)
Click here to contact Evadne Marcolini, MD
There are several conditions that alter ionized calcium levels, including:
The bottom line is to measure ionized calcium, and consider all other factors that can be contributing to hypocalcemia in addition to repleting it.
Category: Misc
Keywords: Altered Mental Status (PubMed Search)
Posted: 2/8/2010 by Rob Rogers, MD
(Updated: 2/3/2026)
Click here to contact Rob Rogers, MD
Altered Mental Status-Does Your Patient Have Non-Convulsive Status Epilepticus?
Ever intubated a patient in status epilepticus and wondered if they were still seizing after sedation and paralysis? Ever taken care of an altered patient and wondered if you should consult neurology and attempt to get an EEG?
NCSE is defined as continuous seizure activity without obvious outward manifestations of a seizure. This is important for emergency physicians to consider because it has to be detected early to prevent morbidity and mortality.
When to consider NCSE:
Category: Orthopedics
Keywords: Scaphoid, Fracture (PubMed Search)
Posted: 2/6/2010 by Michael Bond, MD
Click here to contact Michael Bond, MD
Scaphoid Fractures:
For suspected scaphoid fractures with negative radiographs it is common practice to put a person in a short arm thumb spica splint until followup up radiographs can be obtained in 10-14 days.
However, there is evidence that a short arm thumb spica splint is not enough for people that have a true scaphoid fracture. Gellman et al demonstrated that long arm thumb-spica cast immobilization for six weeks followed by short arm thumb-spica cast immobilization decreased time to union by 25% when compared to short arm thumb-spica casting alone.
The theory is that the short arm splint still allows for forearm rotation that can cause shearing motion of the volar radiocarpal ligaments. A long arm splint prevents this shearing action. The disadvantage of a long arm splint though is potential elbow joint stiffness and muscle atrophy that can occur during the prolonged period of immobilization.
So for your next patient with a scaphoid fracture seen on radiographs place them in a long arm thumb spica splint.
Gellman H, Caputo RJ, Carter V, Aboulafia A, McKay M. Comparison of short and long thumb-spica casts for non-displaced fractures of the carpal scaphoid. J Bone Joint Surg Am. 1989; 71:354-357.
Lawton JN, Nicholls MA, Charoglu CP. Immobilization for Scaphoid Fracture: Forearm Rotation in Long Arm Thumb-spica Versus Munster Thumb-spica Casts. Orthopedics 2007; 30:612
Category: Toxicology
Keywords: antibiotics, imipenem, meropenem, doripenem, ertapenem, colistin, amikacin, multiresistant (PubMed Search)
Posted: 2/4/2010 by Ellen Lemkin, MD, PharmD
Click here to contact Ellen Lemkin, MD, PharmD
CARBAPENENEMS
TIGECYCLINE
AMIKACIN
COLISTIN
1. Lee S. Engel MD. Multidrug-Resistant Gram-Negative Bacteria: Trends, Risk Factors, and Treatments. Emerg Med 41(11):18, 2009.
2. Journal of Antimicrobial Chemotherapy, 2004;Vol 54(6) Pp. 1155-1157
Category: Neurology
Keywords: epilepsy, seizure, driving (PubMed Search)
Posted: 2/3/2010 by Aisha Liferidge, MD
(Updated: 2/3/2026)
Click here to contact Aisha Liferidge, MD
