Category: Critical Care
Posted: 4/23/2024 by Caleb Chan, MD
Click here to contact Caleb Chan, MD
Background:
-Muscle rigidity has been described as a side-effect of fentanyl, specifically activation of expiratory muscles
-Excessive expiratory muscle use acts as “anti-PEEP,” causing lung derecruitment and hypoxemia
-End-expiratory lung volume (EELV) has been used as a surrogate for lung recruitment
Study:
-Small, two center, observational study (46 patients with ARDS)
-50% of patients had a significant increase in EELV after administration of neuromuscular blockade (NMB)
-Statistically significant correlation between a higher dosage of fentanyl and a greater increase in EELV after NMB
Takeaways:
-NMB can improve lung recruitment for a subset of patients with ARDS, particularly in patients with significant expiratory muscle use (this can be seen on your physical exam of your intubated ED boarding patient)
-Although this was not the main point of this study, consider fentanyl-associated “anti-PEEP,” particularly in patients receiving fentanyl whose hypoxemia and/or ventilator mechanics are disproportionate to their imaging
-This can be assessed with NMB (but ensure the patient will have adequate minute ventilation first)
-Naloxone has also been shown to reverse fentanyl-associated rigidity, but obviously would induce patient discomfort/withdrawal
*Of note, because this was an observational trial, it is possible that the patients with increased work of breathing were simply given more fentanyl. Regardless, these findings are consistent with previously documented physiologic side effects of fentanyl.
Plens GM, Droghi MT, Alcala GC, et al. Expiratory muscle activity counteracts positive end-expiratory pressure and is associated with fentanyl dose in patients with acute respiratory distress syndrome. Am J Respir Crit Care Med. 2024;209(5):563-572.
Category: Trauma
Posted: 4/21/2024 by Robert Flint, MD
Click here to contact Robert Flint, MD
PECARN has a decision tool to identify blunt trauma patients under age 18 who are low probability for important intra-abdominal injuries. The questions to ask are:
Answering no to all yields <0.1% chance of intra-abdominal trauma requiring intervention. (See MedCalc link for other calculations)
A prospective validation study in the Lancet yielded 100% sensitivity and negative predictive value in 7542 patients under age 18
This tool can likely be used to guide imaging choices in pediatric blunt abdominal trauma patients
Category: Pediatrics
Keywords: UTI, antibiotic, duration (PubMed Search)
Posted: 4/19/2024 by Jenny Guyther, MD
(Updated: 2/2/2026)
Click here to contact Jenny Guyther, MD
This was a multicenter, randomized double blind, placebo controlled, non inferiority trial looking at children aged 2 months to 10 years with a diagnosis of urinary tract infection to see if the antibiotic course could be shortened from 10 days to 5 days in those patients who have clinically improved by day 5.
Children were prescribed amoxicillin/clavulanic acid, cefixime, cefdinir, cephalexin or trimethoprim-sulfamethoxazole and on day 6, after an in person visit were switched to placebo or continued the same antibiotic course.
A urine sample was collected on days 11-14 and treatment failure was defined as symptomatic urinary tract infection at or before this visit, asymptomatic bacteriuria, positive urine culture or gastrointestinal colonization with resistant organisms.
693 children were randomized in this trial. Children who received 5 days of antibiotics were more likely to have asymptomatic bacteriuria or a positive urine culture on days 11-14 (0.6 vs 4.2%). 28 children would need to be treated with a 10 day course to prevent one treatment failure with the 5 day course.
Bottom line: 10 days is still the ideal duration of treatment for a urinary tract infection, but the rate of failure of a 5 day course was low and the clinical significance of asymptomatic bacteriuria or a positive urine culture in an otherwise asymptomatic child is unknown.
Zaoutis et al. Short-Course Therapy for Urinary Tract Infections in Children The SCOUT Randomized Clinical Trial. JAMA pediatrics. published online June 26, 2023.
Category: Administration
Keywords: staffing, employment, Teamhealth, Medstar, Edelman (PubMed Search)
Posted: 3/16/2024 by Steve Schenkel, MPP, MD
(Updated: 4/17/2024)
Click here to contact Steve Schenkel, MPP, MD
Emergency Medicine staffing groups can be organized in any number of ways. Here’s Leon Adelman’s take:
Read more at https://emworkforce.substack.com/p/state-of-the-us-emergency-medicine-677. Read closely and you’ll find a reference to Maryland.
Category: Critical Care
Posted: 4/17/2024 by William Teeter, MD
(Updated: 4/24/2024)
Click here to contact William Teeter, MD
Moderate to High-Risk Pulmonary Embolism
In stable patients, call your local PE Response Team (PERT) for advice. The UMMC PERT team is available for any patient in the region and can be contacted through Maryland Access Center.
UMMC PERT stratifies by BOVA (with lactate criteria), CTA imaging, and patient physiology/history. For the consult, we will use the patients most recent vitals, their ROOM AIR sat if available, presence of RV dysfunction on echo/CTA, recent lactate, troponin, BNP, bedside/formal echo, and HPI.
Broad management recommendations for moderate or high-risk patients
PERT Acceptance for Transfer to UMMC/CCRU
See below for more information.
****************************************************************************************************************************************
Definitions of RV dysfunction
Absolute Contraindications to Fibrinolytic Therapy in Pulmonary Embolism
UMMC Relative Exclusion Criteria for VA ECMO for PE
HI-PEITHO (NCT04790370) “is a prospective, multicenter RCT comparing Ultrasound-facilitated catheter-directed therapy (USCDT) and best medical therapy (BMT; systemic anticoagulation) with BMT alone in patients with acute intermediate–high-risk PE.”
Inclusion Criteria
Category: EMS
Keywords: pediatric trauma, vital signs, blood pressure (PubMed Search)
Posted: 4/17/2024 by Jenny Guyther, MD
(Updated: 2/2/2026)
Click here to contact Jenny Guyther, MD
The short answer is yes, pediatric trauma patients without blood pressures recorded from EMS had a higher mortality (4.3%) compared to pediatric patients that did have a recorded blood pressure (1.1%). This is based off of a prehospital study conducted in Japan.
Prehospital vital signs are left out more often in pediatric patients compared to adults. Of those vital signs that are recorded, blood pressure is the most common one left off.
There can be several barriers to obtaining a blood pressure on the pediatric patient in the prehospital setting: lack of properly sized equipment, an uncooperative child, and lack of education. However, the inability to obtain a blood pressure can also be due to the patient being more severely injured and having other skills performed or was unable to be obtained due to poor perfusion. In this study, those who did not have a recorded blood pressure also had a lower GCS score and a higher injury severity score.
Shinohara et al. Association between blood pressure recording in prehospital setting and patient outcome in pediatric trauma patients: A prospective matching study. Journal of Trauma and Acute Care Surgery. July 2023. Epub ahead of print.
Category: Ultrasound
Keywords: POCUS; Lumbar Puncture; Neurology (PubMed Search)
Posted: 4/15/2024 by Alexis Salerno Rubeling, MD
(Updated: 2/2/2026)
Click here to contact Alexis Salerno Rubeling, MD
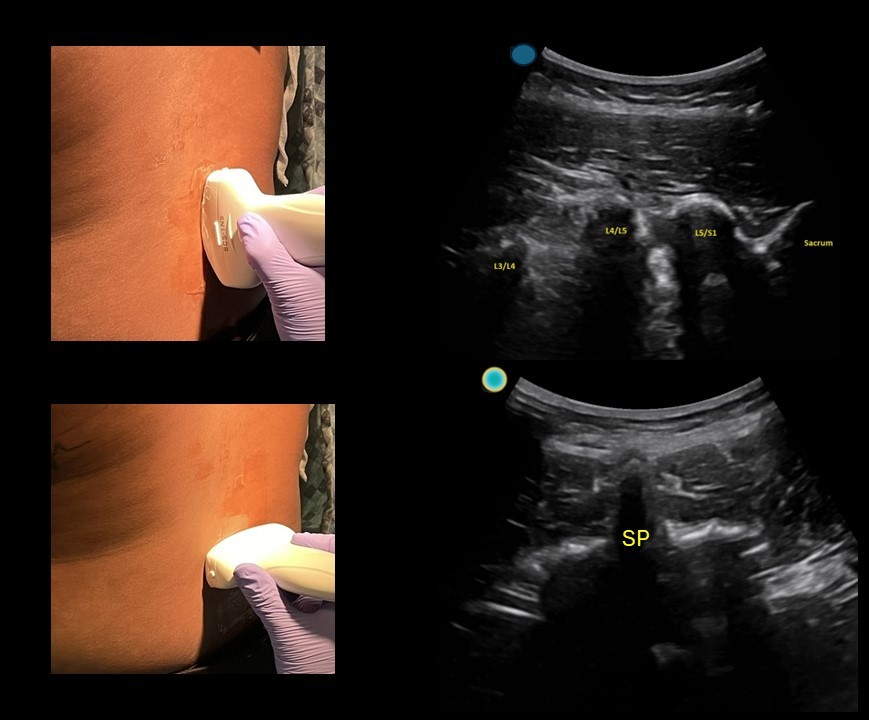
Simple tool to help improve your next lumbar puncture: Use ultrasound for site marking.
This can be done in a patient sitting up or laying on their side.
-First start with the probe marker midline towards the patient's head and use the ultrasound to identify the L4/L5 and L3/L4 space.
-Use a surgical pen away from the gel to mark midline on both sides of the probe, using the midline marker on the ultrasound probe. You can use m mode to help you identify the middle of the image when using a curvilinear probe.
-Then rotate the probe towards the patient's left and use the ultrasound to identify the midline point (spinous process)
-Use a surgical pen away from the gel to mark midline on both sides of the probe, using the midline marker on the ultrasound probe.
-Clean off the gel, connect the skin markings and use a 3 cc syringe to mark the center of the crosshair.
-Sterilize and start your LP!
Category: Trauma
Posted: 4/14/2024 by Robert Flint, MD
(Updated: 2/2/2026)
Click here to contact Robert Flint, MD
This study looked at survival pre and post implementation of an airway guideline for prehospital traumatic brain injury (TBI) patients who received positive pressure airway interventions. The guideline “focused on the avoidance and aggressive treatment of hypotension and 3 airway-related goals: (1) prevention or treatment of hypoxia through early, high-flow oxygen administration; (2) airway interventions to optimize oxygenation or ventilation when high-flow oxygen was insufficient; and (3) prevention of hyperventilation or hypocapnia by using ventilation adjuncts (ie, rate timers, flow-controlled ventilation bags, end-tidal carbon dioxide monitoring).”
Post implementation, survival to admission increased in all severity levels of TBI and in the most severely injured, survival to discharge improved.
Useful for those involved in prehospital education and as a reminder for in hospital airway management in TBI patients.
Gaither JB, Spaite DW, Bobrow BJ, et al. EMS Treatment Guidelines in Major Traumatic Brain Injury With Positive Pressure Ventilation. JAMA Surg. 2024;159(4):363–372. doi:10.1001/jamasurg.2023.7155
Category: Orthopedics
Posted: 4/14/2024 by Brian Corwell, MD
Click here to contact Brian Corwell, MD
Metacarpal fractures are frequently seen in the ED.
These are frequently non operative injuries.
For 4th and 5th metacarpal fractures, consider an ulnar gutter spilt.
For 2nd and 3rd metacarpal fractures, consider a radial gutter splint.
Splinting position (Intrinsic plus):
Wrist in approximately 20 degrees of extension (position of function)
MCP joint in 70 to 90 degrees of flexion
Slight flexion at the DIP and PIP and DIP joints.
-Important to prevent shortening of the collateral ligaments
Category: Pediatrics
Keywords: Pediatrics, preparedness (PubMed Search)
Posted: 4/5/2024 by Kathleen Stephanos, MD
(Updated: 4/12/2024)
Click here to contact Kathleen Stephanos, MD
In early 2023 Newgard et al published an article in JAMA which looked at pediatric readiness in ED's across the county. This study showed that there was a significant increase in pediatric mortality in patients who presented to EDs with lower readiness scores (<87 out of 100) when compared to those with higher readiness scores. And this translated to not just the time in the ED, but up to a year after they are seen in an ill-prepared ED. This number equated to an estimated total of 1,500 preventable deaths in children in the US each year.
Notably this does NOT look at what designation your hospital has for pediatrics (so being a level 1 pediatric trauma center does not automatically give you any points). This is based on having the physical materials needed for each age group, plans in place for specific patient age groups and evaluations (lower radiation doses for children in CT, using an US before CT for appendicitis evaluation, etc), and a person/people in place to review cases and ensure everyone is up to date on pediatric related training.
Want to check YOUR score? Go to https://www.pedsready.org/
Newgard CD, Lin A, Malveau S, et al. Emergency Department Pediatric Readiness and Short-term and Long-term Mortality Among Children Receiving Emergency Care. JAMA Netw Open. 2023;6(1):e2250941. doi:10.1001/jamanetworkopen.2022.50941
Category: Pharmacology & Therapeutics
Keywords: naloxone, opioid (PubMed Search)
Posted: 4/11/2024 by Ashley Martinelli
(Updated: 2/2/2026)
Click here to contact Ashley Martinelli
Naloxone is given frequently in the emergency department to improve the respiratory rate in patients with suspected or known opioid ingestion. In order to minimize the risk of severe opioid withdrawal (nausea, vomiting, diarrhea, anxiety, piloerection, sweating, agitation, etc.), consider diluting naloxone and administering small aliquots of 0.04-0.08mg at a time. This requires IV access and a patient with a present, but low respiratory rate.
Dilution instructions:
Supplies:
Instructions:
Administer 1 -2 mL (0.04 – 0.08 mg) naloxone every 2 minutes and assess response.
Don't forget to prescribe/give naloxone upon discharge from the emergency department.
Category: Critical Care
Keywords: cardiac arrest, OHCA, airway, mechanical ventilation, resuscitation, bag-valve mask, manual ventilation (PubMed Search)
Posted: 4/10/2024 by Kami Windsor, MD
Click here to contact Kami Windsor, MD
In cardiac arrest, avoidance of excessive ventilation is key to achieving HQ-CPR and minimizing decreases in venous return to the heart. The controversy regarding BVM vs definitive airway and OHCA outcomes continues, but data indicates that mechanical ventilation during CPR carries no more variability in airway peak pressures and tidal volume delivery than BVM ventilation [1], with the AHA suggestion to keep in-hospital cardiac arrest patients with COVID-19 on the ventilator during the pandemic [2].
So, can we automate this part of CPR?
Two recent studies looked at mechanical ventilation (MV) compared to bagged ventilation (BV) in intubated patients with out-of-hospital-cardiac arrest (OHCA).
Shin et al.'s pilot RCT evaluated 60 intubated patients, randomizing half to MV and half to BV, finding no difference in the primary outcome of ROSC or sustained ROSC, or ABG values, despite significantly lower tidal volumes and minute ventilation in the MV group [3].
Malinverni et al. retrospectively compared MV and BV OHCA patients from the Belgian Cardiac Arrest Registry, finding that MV was associated with increased ROSC although not with improved neurologic outcomes. Of note, patients across the airway spectrum were included (mask, supraglottic, intubated), and the mechanical ventilation was a bilevel pressure mode called Cardiopulmonary Ventilation (CPV) specific to their ventilators, specifically for use during cardiac arrest [4].
Bottom Line: Larger randomized trials will be necessary to get a definitive answer as to how mechanical ventilation affects outcomes in OHCA, but in instances where the cause of arrest is not primarily pulmonary (severe asthma, pneumothorax) and the ED is short-staffed or prolonged resuscitations are likely (such as in accidental hypothermic arrests), it is probably reasonable to keep patients on the ventilator:
Category: Trauma
Keywords: Trauma, blood pressure, shock index, predictor, mortality (PubMed Search)
Posted: 4/8/2024 by Robert Flint, MD
Click here to contact Robert Flint, MD
Traditionally, a systolic blood pressure (SBP) of 90 has been used as a marker of severe illness in trauma patients. This study looked at a large database and found shock index (SI) and systolic blood pressure were the best predictors of early mortality in trauma patients.
They found:
prehospital SI 0.9 and SBP 110,
ED SI 0.9 and SBP 112,
and
in elderly
prehospital SI 0.8 SBP 116
ED SI 0.8 SBP 121
were the cutoffs to predict early mortality.
We should rethink our protocols and approach to trauma patients using a higher systolic blood pressure than 90. Also note elderly had a different number than younger trauma patients.
April MD, Fisher AD, Rizzo JA, Wright FL, Winkle JM, Schauer SG. Early Vital Sign Thresholds Associated with 24-Hour Mortality among Trauma Patients: A Trauma Quality Improvement Program (TQIP) Study. Prehosp Disaster Med. 2024 Apr 2:1-5. doi: 10.1017/S1049023X24000207. Epub ahead of print. PMID: 38563282.
Category: Trauma
Keywords: Marker, penetrating trauma, radiopaque (PubMed Search)
Posted: 4/7/2024 by Robert Flint, MD
(Updated: 2/2/2026)
Click here to contact Robert Flint, MD
Using radiopaque markers such as paperclips to mark penetrating wounds prior to radiographs has been taught in trauma bays for decades. This article points out there is no evidence to support this practice and is purely based on expert opinion. With the heavy use of CT imaging to assess wound tracks, the use of markers on plain films appears to be of limited utility.
Sarfaraz K, Nemeth J, Bahreini M. The use of radiopaque markers is medical dogma. Acad Emerg Med. 2024 Feb;31(2):193-194. doi: 10.1111/acem.14858. Epub 2024 Feb 6. PMID: 38112251.
Category: Pediatrics
Keywords: pediatrics, sepsis, SIRS, septic shock (PubMed Search)
Posted: 4/5/2024 by Kelsey Johnson, DO
(Updated: 2/2/2026)
Click here to contact Kelsey Johnson, DO
Sepsis remains a leading cause of mortality in the pediatric population, and we have long been overdue for an update in recognizing and risk stratifying our pediatric patients.
Until now, pediatric sepsis screening guidelines have followed a framework modeled after the adult screening criteria from 2001 (Sepsis-2): Systemic Inflammatory Response Syndrome (SIRS). While attempts were made in 2005 to adjust these criteria to the pediatric population, data has shown poor specificity correlating to PICU admissions, need for critical interventions, end organ damage, and mortality.
As a reminder: Pediatric SIRS criteria: Temp >38.5 C or <36 C, tachycardia (or bradycardia if <1yr old), Tachypnea, leukocytosis/ leukopenia or >10% bandemia
In 2016, Sepsis-3 revised the criteria for sepsis and septic shock for the adult cohort by placing the focus on the presence of life-threatening organ dysfunction, which led to adopting criteria such as the SOFA and qSOFA scores to predict mortality risk.
Enter: The Phoenix Sepsis Score
An international, multidisciplinary task force convened by the Society of Critical Care Medicine in 2019 used evidence from an international survey, systematic review and meta-analysis to develop and validate a scoring tool intended to identify life-threatening organ dysfunction in children. Scoring tool was derived and validated retrospectively using an international, multi-center electronic medical record review of 3 million pediatric hospital encounters (excluding pre-term infants born <37 weeks and birth hospitalizations).
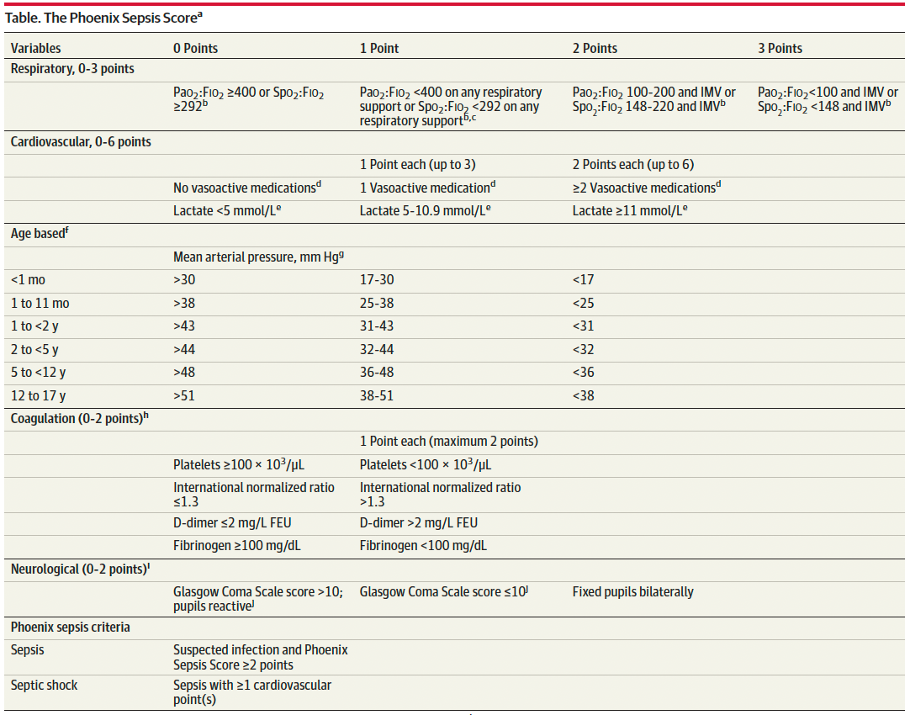
A Phoenix score of at least 2 carried a 7.1% risk of in-hospital mortality (in higher resource settings such as the USA).
Children with sepsis and organ dysfunction remote from the primary site of infection (eg respiratory failure in a child with meningitis) carried the highest mortality burden (8%) in this study.
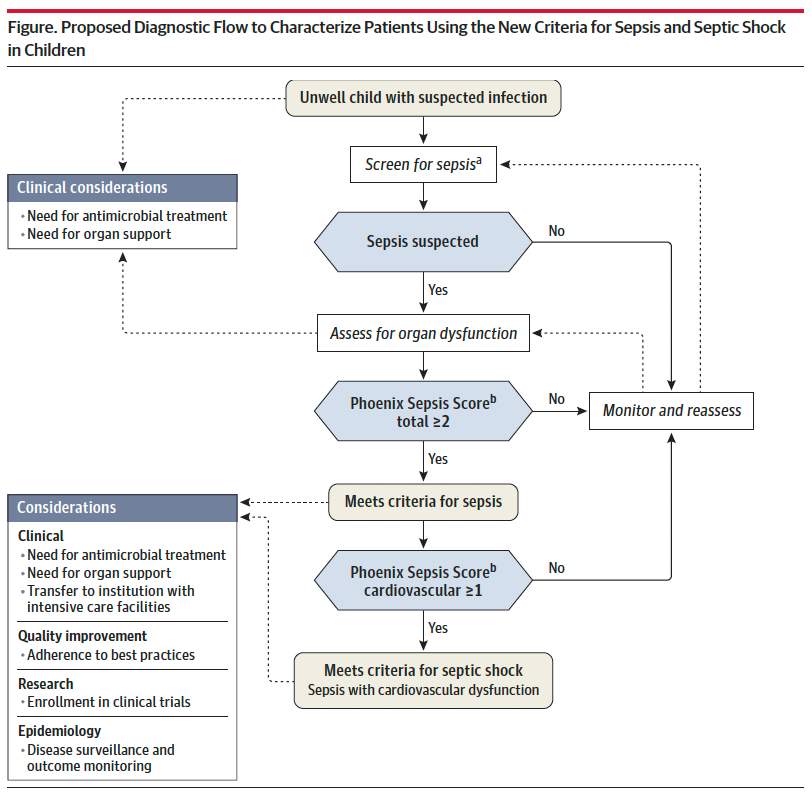
Sepsis is identified in children with suspected infection and an overall Phoenix score of 2 or more points, as this indicates potentially life-threatening organ dysfunction and thus carries higher mortality risk. Septic shock is identified by a score of 1 or more point(s) in cardiovascular dysfunction.
Lastly, it is important to recognize that this scoring criteria is NOT a sepsis screening tool, but rather should be applied when there is clinical suspicion for significant infection in the unwell child, or meeting sepsis screening criteria per your institutional criteria. Screening pediatric patients remains a clinical challenge, and there is not yet a reliable tool to apply to this population.
Bottom Line: Sepsis remains a significant cause of pediatric morbidity and mortality. The Phoenix Sepsis Score should be applied to the unwell child with suspected infection to identify sepsis and septic shock, thereby providing risk stratification and improving clinical care. Sepsis is defined by a Phoenix score of 2 or more and septic shock by a score of 1 or more in the cardiovascular category.
Schlapbach LJ, Watson RS, Sorce LR, et al. International Consensus Criteria for Pediatric Sepsis and Septic Shock. JAMA. 2024;331(8):665–674. doi:10.1001/jama.2024.0179
Category: Obstetrics & Gynecology
Keywords: postpartum, hemorrhage, pregnancy, maternal (PubMed Search)
Posted: 4/4/2024 by Michele Callahan, MD
Click here to contact Michele Callahan, MD
Postpartum hemorrhage (defined as >500 mL blood loss after birth by the WHO and >1000 mL blood loss within 24 hours of birth by ACOG), accounts for 27% of maternal deaths worldwide. It is the leading cause of maternal complications and death worldwide, with approximately 70,000 deaths globally.
In a randomized trial published in the NEJM in 2023, they implemented a bundle of first-response treatments including uterine massage, uterotonic medications, and tranexamic acid and compared this intervention group with a control group providing "usual care". They concluded that early detection of PPH and use of bundled treatment led to a lower risk of postpartum hemorrhage, lower need for laparotomy for bleeding, or lower risk of death from bleeding compared with usual care amongst patients having a vaginal delivery.
This study confirms the already widely-published recommendations for prevention of PPH with active management of the third stage of labor using prophylactic uterotonic medication (most commonly Oxytocin), uterine massage for atony, early cord clamping, and controlled cord traction for delivery of the placenta. Prompt escalation to more aggressive management (including blood transfusion, TXA, and more invasive treatments such as uterine tamponade or surgical intervention) should occur when initial treatments fail.
Gallos I, Devall A, Martin J, et al. Randomized Trial of Early Detection and Treatment of Postpartum Hemorrhage. The New England Journal of Medicine. 2023 Jul;389(1):11-21. DOI: 10.1056/nejmoa2303966. PMID: 37158447.
Category: EMS
Keywords: cardiac arrest, ECMO, E-CPR, mechanical ventilation (PubMed Search)
Posted: 4/3/2024 by Ben Lawner, MS, DO
Click here to contact Ben Lawner, MS, DO
BACKGROUND:
The ideal strategy for out of hospital ventilation is a matter of long standing debate and clinical controversy. To date, improved out of hospital outcomes have been associated with non invasive (BVM) and supraglottic airway (SGA) management strategies. A recent, prospective trial featured in Resuscitation offers a slightly different perspective. The trial enrolled 420 adult patients with refractory out of hospital cardiac arrest due to a shockable rhythm. The study looked at outcomes for patients who received endotracheal intubation (ETI) or supraglottic airway placement. Importantly, the study involved a high volume cannulation center and codified screening criteria for eCPR including: a) ongoing arrest despite 3 shocks, b) treatment with amiodarone, c) mechanical CPR and d) anticipated time to arrival at ECMO cannulation center of <30 minutes.
OUTCOMES:
Compared to patients in the SGA group, patients receiving ETI demonstrated:
In accordance with the study institution's cannulation criteria, more patients in the SGA group were deemed ineligible for ECMO.
BOTTOM LINE:
In this single center study, patients who received ETI as a primary strategy for out of hospital airway management were more likely to meet ECMO eligibility critera and exhibit improved oxygenation and ventilation.
While this is not necessarily a practice changing article, it illustrates the complexities inherent in out of hospital cardiac arrest management. EMS has largely transitioned from a “scoop and run” cardiac arrest strategy to a plan that emphasizes treat in place. For patients who may benefit from E-CPR, additional research is indicated to shed light on best out of hospital resuscitation (and airway management) practices.
Bartos JA, Clare Agdamag A, Kalra R, Nutting L, Frascone RJ, Burnett A, Vuljaj N, Lick C, Tanghe P, Quinn R, Simpson N, Peterson B, Haley K, Sipprell K, Yannopoulos D. Supraglottic airway devices are associated with asphyxial physiology after prolonged CPR in patients with refractory Out-of-Hospital cardiac arrest presenting for extracorporeal cardiopulmonary resuscitation. Resuscitation. 2023 May;186:109769. doi: 10.1016/j.resuscitation.2023.109769. Epub 2023 Mar 17. PMID: 36933882.
Category: Critical Care
Keywords: IV Fluid, balanced solutions (PubMed Search)
Posted: 4/3/2024 by Mark Sutherland, MD
(Updated: 2/2/2026)
Click here to contact Mark Sutherland, MD
Multiple studies have suggested differences in patient outcomes with balanced solutions (e.g. plasmalyte) vs unbalanced solutions (e.g. normal saline) when large volumes are administered. But what about when giving smaller volumes of fluid? Does it matter which one you choose?
A recent study by Raes et al in the Journal of Nephrology looked at urine and serum effects of administering 1L of normal saline, vs 1L of plasmalyte, to ICU patients needing a fluid bolus. Chloride levels, strong ion difference (SID), and base excess were all significantly different between the two groups. There was no difference in blood pressure or need for vasopressors. As best I can tell, other clinically significant differences such as kidney injury were unfortunately not reported.
Bottom Line: When giving small (e.g. 1L) volumes of IVF, there ARE real physiologic differences seen between balanced and unbalanced solutions. Whether these differences translate to patient-oriented or clinically significant outcomes remains unclear.
Raes, M., Kellum, J. A., Colman, R., Wallaert, S., Crivits, M., Viaene, F., Hemeryck, M., Benoît, D., Poelaert, J., & Hoste, E. (2024). Effect of a single small volume fluid bolus with balanced or un-balanced fluids on chloride and acid–base status: a prospective randomized pilot study (the FLURES-trial). JN. Journal Of Nephrology (Milano. 1992). https://doi.org/10.1007/s40620-024-01912-z
Category: Ultrasound
Keywords: POCUS; Ultrasound Artifacts (PubMed Search)
Posted: 4/1/2024 by Alexis Salerno Rubeling, MD
(Updated: 2/2/2026)
Click here to contact Alexis Salerno Rubeling, MD
Ultrasound artifacts can sometimes be helpful, but sometimes they can be misleading.
For example:
1)Does this patient have a gallstone?
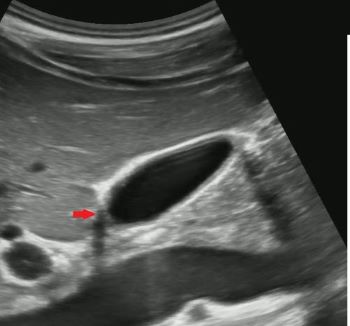
No, this is edge artifact! This is due to the ultrasound signals refracting off the side of the gallbladder wall.

No, this is side lobe artifact! This is due to a bright reflector outside of the central beam of the ultrasound signal that the machine mistakenly places with in the center of the beam. Side lobe artifact can occur near fluid filled masses such as the gallbladder and bladder.

No, this is mirror artifact!! This is due to ultrasound signals bouncing off a highly reflective surface such as the diaphragm. The ultrasound machine misinterprets the time delay from the reflected ultrasound signal as a structure deeper in the image.
Category: Toxicology
Keywords: Alcohol, mortality, predictor, trauma (PubMed Search)
Posted: 3/31/2024 by Robert Flint, MD
(Updated: 2/2/2026)
Click here to contact Robert Flint, MD
This retrospective population cohort study looked at first time ED visits for adolescents and young adults comparing those with visits related to alcohol to those not related to alcohol. Patients in the alcohol related visit group had a threefold increased one year mortality rate. Cause of death was trauma, poisoning by drug and alcohol. Risk factors include being male, age 20-29, history of mental health and having a visit for withdrawal.
Adolescents and young adults presenting to an emergency department for an alcohol related complaint are high risk for one year mortality and deserve intervention and appropriate referral.
Academic Emergency MedicineVolume 31, Issue 3 p. 220-229
Mortality in adolescents and young adults following a first presentation to the emergency department for alcohol
Lyndsay D. Harrison MSc, Asnake Y. Dumicho MSc, Anan Bader Eddeen MSc, Peter Tanuseputro MD, MHSc, Claire E. Kendall MD, PhD, Jess G. Fiedorowicz MD, PhD, Tea Rosic MD … See all authors
