Category: Misc
Posted: 3/26/2024 by Heidi Teague, MD
(Updated: 3/30/2024)
Click here to contact Heidi Teague, MD
Advancements in complex illness management have led to an increasing number of patients surviving longer, with subsequent development of end-stage organ disease, cancer, and dementia. EDs are encountering patients with more complex medical needs who present with challenging complaints such as functional loss, bounce-back visits for uncontrolled symptoms, and caregiver fatigue. ACEP underscored the importance of advancing access to palliative care in 2013 and is one of its top five measures in the Choosing Wisely campaign, aimed at minimizing unwarranted and excessive medical interventions. Proactive symptom management, including promptly addressing pain, dyspnea, nausea, and other distressing symptoms, as well as goals of care conversations, and early referral to hospital and outpatient palliative services can enhance patient and caregiver comfort and quality of life.
Wang DH. Beyond Code Status: Palliative Care Begins in the Emergency Department. Annals of emergency medicine. 2017;69(4):437-443. doi:10.1016/j.annemergmed.2016.10.027
Category: Pediatrics
Posted: 3/29/2024 by Rachel Wiltjer, DO
Click here to contact Rachel Wiltjer, DO
Standard practice regarding various pediatric fractures has started to shift over the last several years, often to less restrictive means of treatment. Torus (buckle) fractures of the distal radius are one of the most common pediatric fractures and tend to heal very well with minimal intervention.
The FORCE study (FOrearm fracture Recovery in Children Evaluation), a multicenter study out of the UK, was conducted to compare rigid immobilization (splinting) to a soft bandage used as needed per family discretion for treatment of these fractures. There was no different in outcomes of self-reported pain, function, quality of life, complications, or school absences. UK orthopedic guidelines have been updated to reflect a recommendation against rigid immobilization as well as against any need for specialist follow-up. American guidelines are slower to follow suit, but in recent years have transitioned to an approach of a removable brace.
Take Home: Pediatric torus fractures of the distal radius likely do not require immobilization and can be managed with self-limited activity instead. Practice in the US is in flux, but it is reasonable to manage with a removable brace or soft dressing as well as pediatrician follow up.
Hussain, M, Perry, D, and Messahel, S. Summary of Recent Advances in Management of Torus Fracture of the Distal Radius in Children_. Arch Dis Child_. Epub ahead of print
Knight R, Dritsaki M, Mason J, Perry DC, Dutton SJ. The Forearm Fracture Recovery in Children Evaluation (FORCE) trial: statistical and health economic analysis plan for an equivalence randomized controlled trial of treatment for torus fractures of the distal radius in children. Bone Jt Open. 2020 Jun 9;1(6):205-213.
Category: Misc
Posted: 3/12/2024 by Mike Witting, MS, MD
(Updated: 3/28/2024)
Click here to contact Mike Witting, MS, MD
Considering starting a research project? Apply the FINER criteria:
Feasible
Do you have the resources to study this? Enough patients? Support?
Interesting
Does it interest you enough to devote your time to it? Does it interest colleagues?
Novel
Would it provide new findings, or confirm, refute, or extend prior findings?
Ethical
Can you think of a way to ethically study it?
Relevant
Consider possible outcomes of your research. Could the study advance care or policy?
Adapted from Hulley SB, Cummings SR. Designing clinical research, 4th edition, Lippincott, Williams and Wilkins, 2013.
Category: Administration
Keywords: Administration, Patient Experience, Microaggression, Discrimination (PubMed Search)
Posted: 3/27/2024 by Mercedes Torres, MD
(Updated: 2/2/2026)
Click here to contact Mercedes Torres, MD
Do microaggressions and discrimination impact the patient experience in your ED? How can we address this?
This article is one of few studies to address this topic specifically in the ED. Authors used quantitative (discrimination scale) and qualitative (follow-up interviews) methods to answer this question in two urban academic EDs.
Common themes from patient responses provide food for thought and action in this regard:
Punches BE, Osuji E, Bischof JJ, et al. Patient perceptions of microaggressions and discrimination toward patients during emergency department care. Acad Emerg Med. 2023; 30: 1192-1200. doi:10.1111/acem.14767
Category: Critical Care
Posted: 3/26/2024 by Mike Winters, MBA, MD
Click here to contact Mike Winters, MBA, MD
Bag-Valve-Mask Ventilation During OHCA
Idris AH, et al. Bag-valve-mask ventilation and survival from out-of-hospital cardiac arrest: A multicenter study. Circulation. 2023;148:1847-56.
Category: Trauma
Keywords: Alcohol, withdrawal, trauma, protocol, sparing (PubMed Search)
Posted: 3/24/2024 by Robert Flint, MD
(Updated: 2/2/2026)
Click here to contact Robert Flint, MD
This study compared admitted trauma patients with alcohol withdrawal or those at risk of withdrawal before and after a benzodiazepine sparing protocol (using clonidine and gabapentin) was initiated. They found a lower daily CIWA score and significantly less lorazepam use in the benzodiazepines sparing group. This sparing protocol appears to be safe and effective.
McCullough, Mary Alyce MD; Miller, Preston R. III MD; Martin, Tamriage MD; Rebo, Kristin A. PharmD; Stettler, Gregory R. MD; Martin, Robert Shayn MD; Cantley, Morgan PharmD; Shilling, Elizabeth H. PhD; Hoth, James J. MD, PhD; Nunn, Andrew M. MD
Journal of Trauma and Acute Care Surgery 96(3):p 394-399, March 2024. | DOI: 10.1097/TA.0000000000004188
Category: Orthopedics
Posted: 3/23/2024 by Brian Corwell, MD
(Updated: 2/2/2026)
Click here to contact Brian Corwell, MD
The OPAL trial attempted to investigate the effectiveness of opioids in the acute management of neck and back pain.
346 adults presenting to the Emergency department or primary care provider with 12 weeks or less of lower back pain, neck pain or both (of at least moderate intensity).
51% male. 49% female.
Location: Sydney, Australia
All participants received guideline care (advice to stay active, reassurance of a positive prognosis, avoidance of bed rest, and, if required, other non-opioid analgesics).
Patients were then randomly assigned to an opioid (oxycodone, up to 20 mg PO qD) or and an identical placebo, for up to 6 weeks*.
*Trial used a combination oxycodone/naloxone to reduce risk of opioid induced constipation and assist with blinding.
*Trial used a modified release formulation that could be dosed q12h rather than q4-6h to increase adherence.
*Recommended regimen was oxycodone 5mg every 12 hours, with titration as necessary, max dose 20mg total per day.
*Trial physicians were able to individualize the prescription to suit the patient’s needs.
* Mean prescribed dose was approx. oxycodone 10mg total daily.
*Most patients only treated for 2 weeks
Primary outcome: Pain severity at 6 weeks
Results: Mean pain score at 6 weeks was identical between groups.
Trend towards faster recovery in the placebo group in the first 2 weeks.
Take home: Consider the likely benefit vs harm of prescribing opioids for acute back and neck pain in the ED.
Friedman BW, Irizarry E, Chertoff A, Feliciano C, Solorzano C, Zias E, Gallagher EJ. Ibuprofen Plus Acetaminophen Versus Ibuprofen Alone for Acute Low Back Pain: An Emergency Department-based Randomized Study. Acad Emerg Med. 2020 Mar;27(3):229-235.
Category: EMS
Keywords: Suicide, EMS, prevention, causes (PubMed Search)
Posted: 3/20/2024 by Jenny Guyther, MD
(Updated: 2/2/2026)
Click here to contact Jenny Guyther, MD
7,365 suicide related cardiac arrests were included in this study that included a several year study period in Queensland Australia. Cardiac arrests where resuscitation was attempted by EMS and where circumstances were concerning for suicide were included. ROSC rates were 28.6% with survival at 30 days being only 8%. 30-day survival for medical cardiac arrests in this jurisdiction was 16.4%. Overdose and poisoning had the best survival rate (19.9%), while hanging and chemical asphyxia were the worst (7.3 and 1.1% respectively).
Bottom line: Survival rates for suicide related out of hospital cardiac arrest were worse compared to other causes of medical arrest. Suicide prevention should become a focus with emphasis on early identification and treatment of people at high risk of suicide. While EMS is well trained on the management of cardiac arrest, training should also emphasize suicide risk assessment and identification.
Doan et al. Suicide related out-of-hospital cardiac arrests in Queensland, Australia: temporal trends of characteristics and outcomes over 14 years. Prehospital Emergency Care. 2023.
Category: Critical Care
Keywords: ROSC, OHCA, cardiac arrest, shock, vasopressors, norepinephrine, noradrenaline, epinephrine, adrenalin (PubMed Search)
Posted: 3/19/2024 by Kami Windsor, MD
Click here to contact Kami Windsor, MD
Post-arrest shock is a common entity after ROSC. There is support for the use of continuous norepinephrine infusion over epinephrine to treat shock after ROSC, due to concerns about increased myocardial oxygen demand and associations with higher rates of rearrest [1,2] and mortality [2,3] with the use of epinephrine compared to norepinephrine, and increased refractory shock with use of epinephrine infusion after acute MI [4].
An article in this month’s AJEM compared norepinephrine and epinephrine infusions to treat shock in the first 6 hours post-ROSC in OHCA [5]. With a study population of 221 patients, they found no difference in the primary outcome of incidence of tachyarrhythmias, but did find that in-hospital mortality and rearrest rates were higher in the epinephrine group.
Bottom Line: Absent definitive evidence, norepinephrine should probably be the first pressor you reach for to manage post-arrest shock, especially if there is strong suspicion for acute myocardial infarction.
Category: Trauma
Keywords: Geriatric trauma, outcome, hospice (PubMed Search)
Posted: 3/17/2024 by Robert Flint, MD
(Updated: 2/2/2026)
Click here to contact Robert Flint, MD
This was a database study of nearly 2 million trauma patients over age 65 who were discharged looking at all levels of trauma centers. The authors found:
“Dominance analysis showed that proportion of patients with Injury Severity Score of >15 contributed most to explaining hospice utilization rates (3.2%) followed by trauma center level (2.3%), proportion White(1.9%), proportion female (1.5%), and urban/rural setting (1.4%).”
Level one centers had the lowest level of discharge to hospice. The authors felt: “As the population ages, accurate assessment of geriatric trauma outcomes becomes more critical. Further studies are needed to evaluate the optimal utilization of hospice in end-of-life decision making for geriatric trauma.”
Fakhry, Samir M. MD, FACS; Shen, Yan PhD; Wyse, Ransom J. MPH; Garland, Jeneva M. PharmD; Watts, Dorraine D. PhD
Journal of Trauma and Acute Care Surgery 94(4):p 554-561, April 2023. | DOI: 10.1097/TA.0000000000003883
Category: Administration
Keywords: Ramadan, fasting (PubMed Search)
Posted: 3/16/2024 by Kevin Semelrath, MD
(Updated: 2/2/2026)
Click here to contact Kevin Semelrath, MD
This study is out of the American University of Beirut, Lebanon, and courtesy of our own Mazen El Sayed!
Many patients of Muslim faith will observe fasting during the month of Ramadan, with no food, water, oral of IV medication taken from sunrise to sunset
This study showed a lower daily ED volume than during non Ramadan months, however did show a higher length of stay during Ramadan.
It also found an increase in mortality rates during Ramadan (OR 2.88) and 72 hour ED bounce-backs (OR 1.34)
Be sensitive and aware of the needs of your patients of Muslim faith during this holy month of fasting.
Ramadan Kareem
Impact of Ramadan on emergency department visits and on medical emergencies. Reem G Al Assaad, Rana Bachir, Mazen J. El Sayed. Europena Journal of Emergency Medicine. 2018, 25:440-444.
Category: Pediatrics
Keywords: Pediatric intubation, airway, cuffed, depth (PubMed Search)
Posted: 3/15/2024 by Jenny Guyther, MD
(Updated: 2/2/2026)
Click here to contact Jenny Guyther, MD
The gold standard for confirming ETT position is a chest xray, but this can often be delayed while the patient is stabilized. Many physicians will estimate ETT insertion depth to be 3x the ETT size, but this is based on selection of the correct tube. There are several other published formulas, including the PALS guidelines [age in years/2 + 12] which applies to children older than one year. In 1982, there was an article published that cited the formulas of [Height (cm) x 0.1 +5] or [Weight(kg)/5 + 12].
This was a retrospective study where the ideal position of cuffed ETT (from the front teeth) was determined by looking at post intubation xrays of 167 patients between 28 days and 18 years. The individual optimal ETT insertion depth was plotted against age, weight and height for all children. This study showed that there is not a fully linear relationship between age, height or weight which is a flaw of all of these formulas. Calculations using the patients’ weight performed the worst. Age based and height formulas performed the best.
Ebenebe et al. Recommendations for endotracheal tube insertion depths in children. Emerg Med J 2023; 0:1-5. epub ahead of print.
Category: Pharmacology & Therapeutics
Keywords: Bactrim, skin and soft tissue infections, Streptococcus spp (PubMed Search)
Posted: 3/14/2024 by Wesley Oliver
Click here to contact Wesley Oliver
MYTH: Bactrim cannot be used as monotherapy for nonpurulent skin and soft tissue infections.
Not True!
Organisms of concern: Streptococcus spp.
Here’s why:
TRUTH: Bactrim CAN be used as monotherapy for nonpurulent skin and soft tissue infections.
Prepared by Rianna Fedora, PharmD on 2/26/24
Category: Critical Care
Posted: 3/12/2024 by Quincy Tran, MD, PhD
(Updated: 2/2/2026)
Click here to contact Quincy Tran, MD, PhD
Background: There is no clear guidelines regarding whether norepinephrine or epinephrine would be the preferred agent to maintain hemodynamic stability after cardiac arrest. In recent years, there has been more opinions about the use of norepinephrine in this situation.
Settings: retrospective multi-site cohort study of adult patients who presented to emergency departments at Mayo Clinic hospitals in Minnesota, Florida, Arizona with out-of-hospital-cardiac arrest (OHCA). Study period was May 5th, 2018, to January 31st, 2022
Participants: 18 years of age and older
Outcome measurement: tachycardia, rate of re-arrest during hospitalization, in-hospital mortality.
Multivariate logistic regressions were performed.
Study Results:
Discussion:
It was retrospective study that uses electronic health records. Thus, other important factors from the pre-hospital settings might not be accurate.
On the other hand, the patient population came from multiple hospitals with varying practices so the patient population is more generalizable.
Conclusion:
Although the rate of tachyarrhythmia was not different between patients receiving norepinephrine vs. epinephrine after ROSC. This study would add more data to the current literature that norepinephrine might be more beneficial for patients with post-cardiac arrest shock.
Normand S, Matthews C, Brown CS, Mattson AE, Mara KC, Bellolio F, Wieruszewski ED. Risk of arrhythmia in post-resuscitative shock after out-of-hospital cardiac arrest with epinephrine versus norepinephrine. Am J Emerg Med. 2024 Mar;77:72-76. doi: 10.1016/j.ajem.2023.12.003. Epub 2023 Dec 10. PMID: 38104386.
Category: Ultrasound
Keywords: ultrasound, nerve block (PubMed Search)
Posted: 3/11/2024 by Alexis Salerno Rubeling, MD
Click here to contact Alexis Salerno Rubeling, MD
What happens if you have a patient who steps on a nail? How can you make this procedure easier for you and the patient?
– Use a Posterior Tibial Nerve Block! !
To Perform This Procedure:
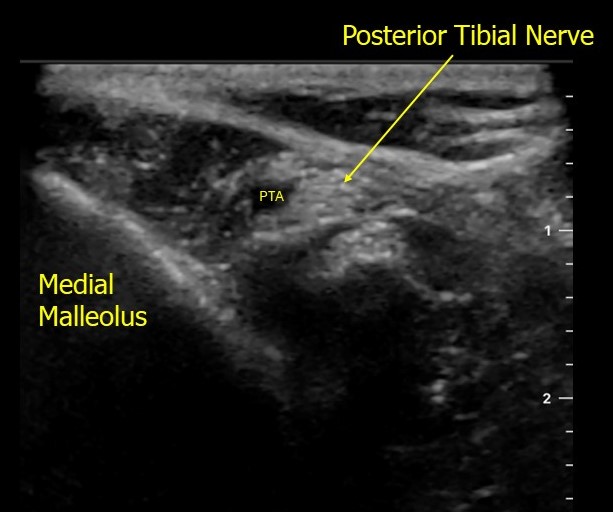
https://www.acep.org/patient-care/map/map-posterior-tibial-nerve-block-tool
Tibial — Highland EM Ultrasound Fueled pain management (highlandultrasound.com)
Category: Trauma
Posted: 3/10/2024 by Robert Flint, MD
(Updated: 2/2/2026)
Click here to contact Robert Flint, MD
This secondary analysis of the NEXUS head injury data found patients over 65:
-sustained more significant injuries than younger pts
-presented more frequently with occult injuries
-when they required neurosurgery intervention only 16% went home, 32% were discharged to rehab facility and 41% died
-mechanism of injury was most commonly fall from standing
-mortality rates were highest for fall from ladder and auto vs. pedestrian injuries
The authors concluded: “Older blunt head injury patients are at high risk of sustaining serious intracranial injuries even with low-risk mechanisms of injury, such as ground-level falls. Clinical evaluation is unreliable and frequently fails to identify patients with significant injuries. Outcomes, particularly after intervention, can be poor, with high rates of long-term disability and mortality.”
William R. Mower, Thomas E. Akie, Naseem Morizadeh, Malkeet Gupta, Gregory W. Hendey, Jake L. Wilson, Lorenzo Pierre Leonid Duvergne, Phillip Ma, Pravin Krishna, Robert M. Rodriguez,
Blunt Head Injury in the Elderly: Analysis of the NEXUS II Injury Cohort,
Annals of Emergency Medicine,
2024,
Category: Orthopedics
Posted: 3/8/2024 by Brian Corwell, MD
(Updated: 2/2/2026)
Click here to contact Brian Corwell, MD
Acetaminophen and low back pain.
Acetaminophen has been a traditionally recommended first line intervention for acute low back pain.
Cochrane reviews in 2016 and 2023 found that acetaminophen showed no benefit compared to placebo in patients with acute low back pain.
A 2020 study investigated whether the addition of acetaminophen to short term NSAID therapy was beneficial.
A randomized double-blind study conducted in two urban emergency departments.
Patients randomized to a 1-week course of ibuprofen plus acetaminophen versus ibuprofen plus placebo.
Population: patients presenting with acute, non-radicular, non-traumatic lower back pain of fewer than two weeks duration.
Authors compared pain and functional outcomes at one week following discharge.
Conclusion: there was no outcome benefit from the addition of acetaminophen to ibuprofen.
Friedman BW, et al. Ibuprofen Plus Acetaminophen Versus Ibuprofen Alone for Acute Low Back Pain: An Emergency Department-based Randomized Study. Acad Emerg Med. 2020 Mar;27(3):229-235.
Category: Trauma
Posted: 3/3/2024 by Robert Flint, MD
(Updated: 2/2/2026)
Click here to contact Robert Flint, MD
This is a retrospective study looking at traumatic brain injury patients comparing those with and without pre-existing psychiatric illness at the time of injury. Those with pre-existing illness had longer hospital stays, longer ICU stays and more frequent readmissions.
Benavides F, Liporaci J, Getchell J, et al. Effects of pre-existing psychiatric illness on traumatic brain injury outcomes: A propensity-matched cohort study. Trauma. 2024;0(0). doi:10.1177/14604086231187157
Category: Quality Assurance/Quality Improvement
Keywords: Metacognition, Diagnostic Error (PubMed Search)
Posted: 3/2/2024 by Brent King, MD
(Updated: 2/2/2026)
Click here to contact Brent King, MD
This classic article should be on everyone’s reading list.
The Bottom Line: Clinicians engaging in metacognition, that is thinking about our reasoning process, can avoid making some critical errors and falling victim to cognitive biases.
Diagnostic errors are common in clinical medicine and particularly common in situations in which the clinician is faced with a novel circumstance and cannot, therefore easily apply heuristics or rules. There are also certain classic situations in which cognitive errors often occur (e.g., mistaking intracranial injury for intoxication). Through a process of active consideration of one’s diagnostic approach, many errors and cognitive biases (particularly availability bias and anchoring bias) can be avoided.
Take-home message: This article is worth reading in its entirety. Applying these principles can protect both patients and clinicians from the consequences of diagnostic errors.
Croskerry, P. Cognitive forcing strategies in clinical decision-making. Ann Emerg Med 2003;41:110-120
Category: Pediatrics
Posted: 2/29/2024 by To-Lam Nguyen, MD
(Updated: 3/1/2024)
Click here to contact To-Lam Nguyen, MD
You've heard of one kill pills such as calcium channel blockers, beta blockers, sulfonylureas, anti-malarials, but less commonly known is benzonatate, or tessalon perles.
Tessalon perles are not recommended for children under the age of 10. 1-2 capsules of benzonatate in children <2 years old have been reported to cause serious side effects including restlessness, tremors, convulsions, coma and even cardiac arrest rapidly after ingestion (within 15-20 minutes and death within a couple of hours). It is attractive to young children as it somewhat resembles a jelly bean.
Pearls on Tessalon Perles:
https://www.poison.org/articles/are-benzonatate-capsules-poisonous
Thimann DA, Huang CJ, Goto CS, Feng SY. Benzonatate toxicity in a teenager resulting in coma, seizures, and severe metabolic acidosis. J Pediatr Pharmacol Ther. 2012 Jul;17(3):270-3. doi: 10.5863/1551-6776-17.3.270. PMID: 23258970; PMCID: PMC3526931.
