Category: Trauma
Posted: 2/29/2024 by Robert Flint, MD
(Updated: 2/2/2026)
Click here to contact Robert Flint, MD
This meta analysis did not find convincing evidence for or against seizure prophylaxis for admitted moderate to severe traumatic brain injury pts. They recommend Levetiracetam over other medications again on weak evidence.
Frontera, J.A., Gilmore, E.J., Johnson, E.L. et al. Guidelines for Seizure Prophylaxis in Adults Hospitalized with Moderate–Severe Traumatic Brain Injury: A Clinical Practice Guideline for Health Care Professionals from the Neurocritical Care Society. Neurocrit Care(2024). https://doi.org/10.1007/s12028-023-01907-x
Category: Administration
Keywords: employee, independent contractor, employment, job market (PubMed Search)
Posted: 1/12/2024 by Steve Schenkel, MPP, MD
(Updated: 2/28/2024)
Click here to contact Steve Schenkel, MPP, MD
The relationship between an Emergency Physician and the hiring group (whether large or small) may be one of employer-employee or contactor-independent contractor. There are legal job protections for employees that don’t exist for independent contractors. There are also regulations that define an independent contractor. Enforcement of these regulations varies but may be increasing. This has implications for the Emergency Medicine job market. We have the highest percentage of independent contractors of any medical specialty.
See more at Leon Adelman’s Emergency Medicine Workforce Newsletter, here https://emworkforce.substack.com/p/thousands-of-employed-emergency-physicians
Category: Hematology/Oncology
Keywords: Cancer, ACS, AMI, troponin (PubMed Search)
Posted: 2/26/2024 by Sarah Dubbs, MD
(Updated: 2/2/2026)
Click here to contact Sarah Dubbs, MD
Evidence is mounting that individuals with active or past history of cancer are at increased risk for acute cardiovascular events such as as acute myocardial infarction. This secondary analysis from the APACE (Advantageous Predictors of Acute Coronary Syndromes Evaluation) study- a multicenter, international, prospective diagnostic study looked at the prevalence of MI in patients with history of cancer presenting to the ED with acute chest pain, diagnostic accuracy of high-sensitivity troponins and diagnostic algorithms (European Society of Cardiology algorithm- see paper for details), among a few other parameters.
Take home points:
Translation to practice:
Be more conservative with cancer patients presenting to the ED with acute chest pain!
Bima, P, Lopez-Ayala, P, Koechlin, L. et al. Chest Pain in Cancer Patients: Prevalence of Myocardial Infarction and Performance of High-Sensitivity Cardiac Troponins. J Am Coll Cardiol CardioOnc. 2023 Oct, 5 (5) 591–609.
https://doi.org/10.1016/j.jaccao.2023.08.001
Category: Trauma
Keywords: Hip fracture l, hemoglobin l, mortality (PubMed Search)
Posted: 2/25/2024 by Robert Flint, MD
(Updated: 2/2/2026)
Click here to contact Robert Flint, MD
In this study, geriatric hip fracture patients with a hemoglobin less than 7.1 had higher mortality, especially in those over age 79, even when controlling for other factors such as ASA Physical status class, anti-platelet use, etc.
Bruce K, Mangram A, Sucher JF_, et al_
Consequences of anemia in geriatric hip fractures: how low is too low?
Trauma Surgery & Acute Care Open 2024;**9:**e001175. doi:10.1136/tsaco-2023-001175
Category: Orthopedics
Keywords: neck pain, radiculopathy (PubMed Search)
Posted: 2/24/2024 by Brian Corwell, MD
Click here to contact Brian Corwell, MD
Axial neck pain is a dull aching “soreness” pain from the posterior neck muscles with radiation to the occiput, periscapular and shoulder regions.
Associated with headaches, stiffness and muscle spasm.
Patients with cervical radiculopathy, however, usually present with unilateral pain discomfort.
Patients may complain of pain radiation into the ipsilateral arm. Though frequently difficult to describe, this may be in a dermatomal distribution. Patients may also report decreased sensation in a dermatomal distribution or weakness along the corresponding myotome.
The most affected nerve roots are C7 (C6-7 herniation), followed by C6 (C5-6 herniation) and C8 (C7-T1 herniation).
Cervical Spondylosis (degenerative change) is the most common ideology.
As discs breakdown with age and lose height, increased force loads are transmitted to bony regions of the spinal segment leading to bone hypertrophy which creates foraminal stenosis and resultant radiculopathy.
Cervical radiculopathy, like lumbar radiculopathy, is largely a self-limited condition. Several older studies following this diagnosis revealed that a majority of patients were either asymptomatic or mildly symptomatic at time of follow-up.
Improvement is seen over the initial four to six months following diagnosis.
Category: Administration
Posted: 2/22/2024 by Robert Flint, MD
(Updated: 2/2/2026)
Click here to contact Robert Flint, MD
This research letter notes: “The Rural Emergency Hospital is a new Medicare payment model available to hospitals with 50 or fewer beds in rural areas. Rural hospitals converting to this model will have emergency department (ED), observation, and outpatient services.”. Their study concludes that the majority of these hospitals already transfer the vast majority of their admissions to larger hospitals and this designation is a recognition of already established practices.
https://doi.org/10.1016/j.annemergmed.2023.08.492
RESEARCH LETTER| VOLUME 83, ISSUE 2, P177-180, FEBRUARY 2024
Category: EMS
Keywords: vital signs, age, pediatric, prehospital intervention (PubMed Search)
Posted: 2/21/2024 by Jenny Guyther, MD
(Updated: 2/2/2026)
Click here to contact Jenny Guyther, MD
Vital signs in children can be difficult to remember since they vary with age. Using a standardized card or app (such as PALS) can help EMS clinicians remember the values. Most pediatric vital sign reference ranges were derived from samples of healthy children in the outpatient setting (ie PALS). This study attempted to validate a range of pediatric vital signs that were more accurate in predicting the need for prehospital interventions compared to the standard PALS vital sign ranges. The thought was that by using EMS data, these vital sign ranges could better alert EMS to patients in need of acute intervention.
The authors used a large EMS database to determine the vital signs for the patients age and correlated that to prehospital interventions (including IV, medication, EKG, advanced airway management, ect). They used the <10% and >90% for the age values (termed "extreme" vitals signs) as a cut off to be considered abnormal. Using the EMS derived values, 17.8% of the encounters with an extreme vital sign received medication. If the PALS abnormal vital sign range was used, only 15.2% of those patients were given medications. Overall, encounters with an extreme vital sign had a higher proportion of any intervention being performed compared to other vital sign criteria (i.e. only 33.7% with PALS).
These extreme vital signs also had a greater accuracy in predicting mortality.
Bottom line: While vital signs are based on physiology that does not change based on location, using a seperate criteria for the EMS population, can improve discrimination between sick and sicker patients and hopefully allow EMS to recognize and intervene on sicker patients sooner.
Ramgopal S, Sepanski RJ, Crowe RP, Martin-Gill C. External validation of empirically derived vital signs in children and comparison to other vital signs classification criteria [published online ahead of print, 2023 Apr 27]. Prehosp Emerg Care. 2023;1-15. doi:10.1080/10903127.2023.2206473
Category: Critical Care
Keywords: poisoning, intoxication, altered mental status, GCS, endotracheal intubation (PubMed Search)
Posted: 2/20/2024 by Kami Windsor, MD
Click here to contact Kami Windsor, MD
Background: Acutely intoxicated / poisoned patients are commonly encountered in the ED, with the classic teaching that a GCS < 9 is an indication to intubate for airway protection. But we’ve probably all had a patient who was borderline, or who we thought was still protecting their airway pretty well despite a lower GCS. Are we risking our patient’s health and our careers by holding off on intubation? Maybe not.
The NICO trial, a multicenter, randomized controlled trial, looked at patients presenting by EMS with GCS <9 due to suspected poisoning, without immediate indication for intubation (defined by signs of respiratory distress with hypoxia, clinical suspicion of any brain injury, seizure, or shock with systolic BP <90 mmHg). They found that withholding intubation with close monitoring, compared to the standard practice of intubating at the EMS or ED physician’s discretion, resulted in:
Comparing the patients who were intubated in each group, there was no significant difference between groups in:
Notes:
Bottom Line: Without clear indication for intubation such as respiratory distress or accompanying head bleed, etcetera, intubation for mental status alone shouldn't be dogma in acute intoxication. Close monitoring will identify need for intubation, without apparent worsened outcomes due to a watchful waiting approach.
Freund Y, Viglino D, Cachanado M, et al. Effect of Noninvasive Airway Management of Comatose Patients With Acute Poisoning: A Randomized Clinical Trial. JAMA. 2023; 330(23):2267-2274. doi: 10.1001/jama.2023.24391.
Category: Trauma
Keywords: Pelvic binder, trauma, survival, mortality (PubMed Search)
Posted: 2/18/2024 by Robert Flint, MD
(Updated: 2/2/2026)
Click here to contact Robert Flint, MD
This retrospective study of 66 trauma patients who had pelvic fractures attempted to determine if prehospital applied pelvic binders had an impact on mortality. There were 3 cohorts: appropriately applied binders (14), inappropriately applied (14 not at the level of the greater trochanter), and none applied (38). Survival for applied was 92% and those without was 81% which was not statistically significant. The authors concluded: “In conclusion, our study found that the use of prehospital pelvic binders did not show a significant effect on patient outcomes for those with unstable pelvic fractures. Instead, injury severity score (ISS) emerged as the most significant predictor of survival.”
Previous studies have shown regular education is needed on proper use of binders. We should continue to educate on appropriate positioning and the use of pelvic binders. For me, this study is not large enough to convince that we should go away from binder use. We need more data before we abandon the pelvic binder.
Alonja Reiter, André Strahl, Sarina Kothe, Markus Pleizier, Karl-Heinz Frosch, Konrad Mader, Annika Hättich, Jakob Nüchtern, Christopher Cramer,
Does a prehospital applied pelvic binder improve patient survival?,
Injury,
2024,
111392,
ISSN 0020-1383,
Category: Pediatrics
Keywords: myositis, acute kidney injury, problems walking, calf pain (PubMed Search)
Posted: 2/14/2024 by Jenny Guyther, MD
(Updated: 2/16/2024)
Click here to contact Jenny Guyther, MD
BACM stands for benign acute childhood myositis which is typically a benign, viral induced self limiting illness. This was a retrospective study looking at 65 patients in Italy to further characterize the characteristics of the disease.
In this study, the median patient age was 6 years with a male predominance. The incidence of BACM peaked in winter with a second peak in the fall. Patients presented with prodromal symptoms including fever, cough, coryza, sore throat and vomiting. The exam showed difficulty walking and myalgias with reproducible calf tenderness and preserved reflexes. Influenza B and A, COVID and other viral pathogens have been detected in these patients.
Lab work may show an elevated creatinine kinase, AST and potassium. WBC and CRP may also be elevated. The median CK value was 943 U/L and on average normalized within one week. Other studies have shown median CK values in the 3300s. Treatment includes hydration to promote CK clearance and prevent complications including acute kidney injury related to rhabdomyolysis. Recurrent myositis or CK values > 5000 U/L should have screening tests for muscular dystrophy and metabolic disorders.
Attainaese et al. Benign acute children myositis: 5 year experience in a tertiary pediatric hospital. European Journal of Pediatrics, published online July 18 2023.
Category: Toxicology
Keywords: bupropion, QRS widening, NaHCO3 (PubMed Search)
Posted: 2/15/2024 by Hong Kim, MD
(Updated: 2/2/2026)
Click here to contact Hong Kim, MD
Bupropion associated cardiac toxicity widens the QRS complex by inhibiting the cardiac gap junction, not cardiac Na channel blockade. NaHCO3 is often administered when EKG changes are noted. But the effectiveness of NaHCO3 in bupropion toxicity is not well established.
A retrospective study between 2010-2020 showed, that administration of NaHCO3 only decreased QRS duration by 2 msec (median). The median NaHCO3 administered was 100 mEq. Although this study was limited by the fact that it only had a small sample size of 13, NaHCO3 administration may provide limited clinical benefit in patients with QRS widening from bupropion overdose.
Simpson M et al. Sodium bicarbonate treatment for QRS widening in bupropion overdoses
Category: Gastrointestional
Keywords: ED recidivism, abdominal pain, follow up appointments (PubMed Search)
Posted: 2/14/2024 by Neeraja Murali, DO, MPH
(Updated: 2/2/2026)
Click here to contact Neeraja Murali, DO, MPH
How many times have you discharged a patient with a clinical impression of “abdominal pain” with no clear explanation or diagnosis?
How many of these times do you direct them to follow up with gastroenterology? And more importantly, how often do they actually do so?
This study discussed a multi-disciplinary approach to ensuring adequate follow up for patients, utilizing an EMR based transition of care (TOC) program. The study stratified patients into 2 groups, pre and post TOC program implementation, to assess rates of appointment scheduling and attendance, as well as rates of return to ED within 30 days. Patients were further stratified based on their Distressed Communities Index (DCI) score (a composite of 7 different socioeconomic metrics) into 5 tiers: Distressed Communities, At Risk Communities, Mid-Tier Communities, Comfortable Communities, and Prosperous Communities. Prior to the implementation of the TOC program, the onus was on the patient to schedule their appointment. The TOC program consisted of an order placed in EMR, which triggered review of the patient's chart by the gastroenterology attending or NP. This individual would then message the information to the appropriate GI subspecialty clinic, along with a time frame in which the patient should be seen. The clinic would then check the patient's insurance reach out to the patient directly to schedule the appointment.
While there was no signifcant difference in 30-day readmission between the pre and post TOC program patients, the post-implementation group was found to both schedule appointments (50% vs 27% p-value <0.01) AND show up to appointments (34% vs 24% p-value <0.01) at significantly higher rates compared to Pre-TOC patients. Additionally, post-TOC patients in the At-Risk and Distressed DCI groups were 22x more likely to follow up than the same groups in the pre-TOC group (OR 22.18, 95% CI 4.23–116.32).
Though the study had promising results, it did admittedly have some limitations, namely the size of the at-risk and distressed groups. Another consideration, though not mentioned in the paper, is that access to a working phone is necessary to the success of this program. Nevertheless, the idea of a TOC program is worth consideration as a means to ensure that patients are not lost to follow up and potentially reduce the risk of adverse events.
Mizrahi J, Marhaba J, Buniak W, Sun E. Transition-of-care program from emergency department to gastroenterology clinics improves follow-up. Am J Emerg Med. 2023;69:154-159. doi:10.1016/j.ajem.2023.04.030
Category: Administration
Keywords: Transfer, surgery, scoping review, further research (PubMed Search)
Posted: 1/28/2024 by Robert Flint, MD
(Updated: 2/11/2024)
Click here to contact Robert Flint, MD
These authors performed a scoping review of English language studies involving United States general surgery patients that required transfer to another facility looking at timing of transfer, triage guidelines, and mode of transport . They concluded: “There were mixed results for the impact of transfer timing on outcomes with heterogeneous definitions of delay and populations. Triage guidelines for EGS transfer were consensus or expert opinion. No studies were identified addressing the mode of interfacility EGS transfer.” More research is needed in the area concerning timing, triage and mode of transport for these patients.
Silver, David S. MD, MPH; Teng, Cindy MD; Brown, Joshua B. MD, MSc. Timing, triage, and mode of emergency general surgery interfacility transfers in the United States: A scoping review. Journal of Trauma and Acute Care Surgery 95(6):p 969-974, December 2023. | DOI: 10.1097/TA.0000000000004011
Category: Misc
Posted: 2/10/2024 by Brian Corwell, MD
(Updated: 2/2/2026)
Click here to contact Brian Corwell, MD
Ever see a commercial showing active fit people drinking sugar beverages?
Ever wonder if exercise is protective from the effects of added sugar?
What are the health risks of added sugar?
How much is too much?
C. elegans, a roundworm, shares 40% of its genes with humans
-Frequently used as a model for health and longevity research
In a 2021 study, researchers altered the diet of the roundworms and found that added sugar was linked to increased glycation end products, high levels of which are associated with an increased risk of CV disease, diabetes and Alzheimer’s disease.
Foods such as fruits are high in natural sugars. Added sugars however are “added” by manufactures to increase flavor.
In our diet, added sugars are everywhere from white bread to ketchup to your favorite Starbucks beverage.
-Sugar- sweetened beverages are the largest source of added sugars in the American diet.
In 2016 the FDA added a section on nutritional labels for added sugars.
The CDC advises limitation of added sugars to 10% of total daily caloric intake.
Added sugars (vs. natural sugars) are more likely to cause spikes in blood sugar and create an inflammatory state thereby increasing the risk of numerous medical problems.
A recent study from the Harvard school of public health investigated whether the benefits of physical activity outweigh the risks of CV disease associated with consumption of sugar-sweetened beverages.
Using 2 cohorts (100,000 people) over a 30-year period, those who consumed sugar-sweetened beverages more than twice a week had a higher risk of CV disease.
Those with daily consumption were at higher risk.
Even those that hit the recommended 150 minutes of weekly exercise were not protected.
Physical activity only reduced the risk of CV disease by approximately 50%.
Though the study did not specifically look at sports and energy drinks, these beverages are large sources of added sugars.
For example, A 20-ounce Gatorade's Thirst Quencher contains 36g of sugar.
Take home: Added sugar, even in moderation, may have negative health consequences even in individuals who exercise regularly.
Category: Pediatrics
Keywords: pediatrics, fever, neonate, preterm (PubMed Search)
Posted: 2/9/2024 by Kathleen Stephanos, MD
Click here to contact Kathleen Stephanos, MD
It is an often asked question: should I consider the corrected or the chronologic age when determining the need for fever evaluation in a pediatric patient? The 2021 AAP guidelines for the well appearing febrile neonate are widely accepted and apply to neonates under 60 days. These highly practical guidelines are, unfortunately, not applicable to pre-term neonates. The question often becomes what age to use for a pre-term neonate- the age they actually are, or the age they would be if they had completed a full term gestation.
Hadhud et al attempted to clarify the age utilized in a retrospective review. This looked at febrile 448 pre-term neonates evaluated for fevers. It found that those patients with both a corrected and chronologic age over 3 months had a 2.6% rate of serious bacterial infections or SBI (UTI, bacteremia or meningitis), those with a corrected age under 3 months but a chronologic age over 3 months had a 16.7% rate of SBIs, and those with both a corrected and chronologic age of under 3 months had a 33.3% rate of SBI.
Overall, these rates of infection are higher than the typically reported in febrile neonates, supporting that pre-term neonates have a much higher risk of infections overall. Ultimately, pre-term neonates should be carefully assessed and a more thorough evaluation is typically warranted in this patient population even if they have reached the generally accepted 60 day marker by chronologic age- use the corrected age.
Hadhud M, Gross I, Hurvitz N, Ohana Sarna Cahan L, Ergaz Z, Weiser G, Ofek Shlomai N, Eventov Friedman S, Hashavya S. Serious Bacterial Infections in Preterm Infants: Should Their Age Be "Corrected"? J Clin Med. 2023 May 1;12(9):3242. doi: 10.3390/jcm12093242. PMID: 37176683; PMCID: PMC10178985.
Category: Pharmacology & Therapeutics
Keywords: Necrotizing Fasciitis, Necrotizing Soft Tissue Infection, Skin and Soft Tissue Infection, clindamycin, linezolid, NSTI (PubMed Search)
Posted: 2/8/2024 by Matthew Poremba
Click here to contact Matthew Poremba
Empiric antimicrobial treatment for necrotizing soft tissue infections (NSTIs) should include coverage of a wide range of pathogens including Staphylococcus spp, Streptococcus spp, anaerobic bacteria and gram negative bacteria. Treatment should also include an agent that suppresses toxin production by group A Streptococcus (GAS), with the Infectious Diseases Society of America (IDSA) guidelines recommending clindamycin plus penicillin for treatment of GAS causing necrotizing fasciitis and toxic shock syndrome. A typical empiric NSTI regimen would be vancomycin plus clindamycin plus piperacillin-tazobactam.
Linezolid is an appealing alternative to clindamycin and vancomycin, as it has anti-toxin effects via inhibition of exotoxin expression, potent in vitro activity against Streptococcus spp, activity against methicillin-resistant Staphylococcus aureus (MRSA), and potential for less adverse effects than clindamycin plus vancomycin. Several recent studies have looked at using linezolid in lieu of clindamycin plus vancomycin when treating NSTIs.
Published Studies:
Dorazio and colleagues published a retrospective single center study compared 62 matched pairs of patients who received linezolid vs. clindamycin plus vancomycin as part of their NSTI treatment.
Heil and colleagues published a retrospective single center cohort study examined patients who received either linezolid (n = 29) or clindamycin (n = 26) for treatment invasive soft tissue infection or necrotizing fasciitis with GAS isolated from blood and/or tissue.
Lehman and colleagues published a retrospective single center study compared patients who received linezolid (n = 21) versus clindamycin plus vancomycin (n = 28) in addition to gram-negative and anaerobic coverage for empiric treatment of NSTIs.
Bottom Line:
When added to an agent with good gram negative and anaerobic coverage (i.e. piperacillin-tazobactam), linezolid may be a more viable option for coverage of MRSA and GAS toxin production during empiric NSTI treatment when compared to clindamycin plus vancomycin. This is largely due to a more favorable side effect profile.
Category: Critical Care
Posted: 2/6/2024 by Mike Winters, MBA, MD
Click here to contact Mike Winters, MBA, MD
PEEP in the Ventilated COPD Patient?
Jubran A. Setting positive end-expiratory pressure in the severely obstructive patient. Curr Opin Crit Care. 2024; 30:89-96.
Category: Ultrasound
Keywords: POCUS; Renal Colic; Flank Pain; Hydronephrosis (PubMed Search)
Posted: 2/5/2024 by Alexis Salerno Rubeling, MD
Click here to contact Alexis Salerno Rubeling, MD
Ultrasound is the first line diagnostic tool to evaluate younger patients who present to the ED with flank pain.
Most of the time on ultrasound, you will not see the actual kidney stone. More often, you will see associated signs such as hydronephrosis.
In a patient with hydronephrosis, the normally hyperechoic renal pelvis will become anechoic. With increased severity of the hydronephrosis, you can have complete distortion of the kidney.

You can tell the difference between hydronephrosis and a renal vein by placing color doppler over the image. Hydronephrosis will not have flow.
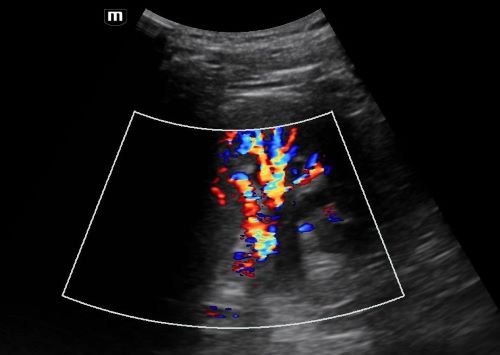
Moore CL, Carpenter CR, Heilbrun ML, et al. Imaging in Suspected Renal Colic: Systematic Review of the Literature and Multispecialty Consensus. J Urol. 2019 Sep;202(3):475-483. doi: 10.1097/JU.0000000000000342.
Category: Trauma
Keywords: Ct, head injury, geriatric (PubMed Search)
Posted: 1/28/2024 by Robert Flint, MD
(Updated: 2/4/2024)
Click here to contact Robert Flint, MD
In this prospective study looking at geriatric patients with unknown head injury vs. known head injury, the unknown head injury group had an ICH 1.5%, neurosurgical intervention 0.3% and delayed ICH 0.1% when compared to known head injury (10.5%, 1.2% and 0.7% respectively). The authors concluded that the risk of ICH was high enough in uncertain head injury patients to warrant scanning.
Turchiaro ML Jr, Solano JJ, Clayton LM, Hughes PG, Shih RD, Alter SM. Computed Tomography Imaging of Geriatric Patients with Uncertain Head Trauma. J Emerg Med. 2023 Dec;65(6):e511-e516. doi: 10.1016/j.jemermed.2023.07.009. Epub 2023 Jul 26. PMID: 37838489.
Category: Quality Assurance/Quality Improvement
Keywords: Patient Mortality, Emergency Department Closure (PubMed Search)
Posted: 2/2/2024 by Brent King, MD
(Updated: 2/3/2024)
Click here to contact Brent King, MD
Takeaway Message: In this study from England, the closure or downgrading of selected emergency departments had no observable impact on patient mortality.
Due to staffing shortages in the UK, the NHS has closed or reduced the capacity of some emergency departments thus strategically concentrating emergency services. The authors of this observational study sought to determine the impact on patient mortality from the closure of five emergency departments between 2007 and 2014. While transport time to an emergency department did increase by up to 25 minutes (median change - 9 minutes, range 0-25 minutes), no change in mortality was identified in the population studied.
The Bottom Line: Closure of selected emergency departments had no impact on population mortality in this UK study but the affected patients had other EDs in relatively close proximity to the ones that had closed.
Comment: This article's findings contradict those of a previously posted Pearl which noted a decrease in mortality when newly opened EDs reduced the volume of existing EDs (Woodworth L. Swamped: Emergency department crowding and patient mortality. Journal of Health Economics, 2020; 70: 102279). The reasons for this discrepancy are unclear but may be due to differences in the healthcare systems of the US and UK.
Knowles E, Shephard N, Stone T_, et al_
The impact of closing emergency departments on mortality in emergencies: an observational study
Emergency Medicine Journal 2019;**36:**645-651.
