Category: Pediatrics
Posted: 12/1/2023 by To-Lam Nguyen, MD
Click here to contact To-Lam Nguyen, MD
Since Christmas is coming up, let's talk about Hemophilia A (factor VIII deficiency) and Hemophilia B (factor IX deficiency, also known as Christmas disease)
Deficiencies in Factors VIII and IX are the most common severe inherited bleeding disorders.
Pathophysiology:
Clinical Manifestations:
Lab findings and diagnosis
Genetics
Classification
trauma to induce bleeding
Treatment
Summary:
Kliegman R, Stanton B, St. Geme JW, Schor NF, Behrman RE. Nelson Textbook of Pediatrics. Edition 20. Elsevier; 2016. Accessed December 2, 2023. https://search.ebscohost.com/login.aspx?direct=true&db=cat01362a&AN=hshs.004567758&site=eds-live
Kliegman R, Stanton B, St. Geme JW, Schor NF, Behrman RE. Nelson Textbook of Pediatrics. Edition 20. Elsevier; 2016. Accessed December 2, 2023. https://search.ebscohost.com/login.aspx?direct=true&db=cat01362a&AN=hshs.004567758&site=eds-live
Category: Critical Care
Posted: 11/28/2023 by Caleb Chan, MD
(Updated: 2/2/2026)
Click here to contact Caleb Chan, MD
McCallister R, Nuppnau M, Sjoding MW, Dickson RP, Chanderraj R. In patients with sepsis, initial lactate clearance is confounded highly by comorbidities and poorly predicts subsequent lactate trajectory. CHEST. 2023;164(3):667-669.
Category: Hematology/Oncology
Keywords: Transfusion, Anemia, MI, ACS, hematology (PubMed Search)
Posted: 11/27/2023 by Sarah Dubbs, MD
Click here to contact Sarah Dubbs, MD
Hot off the NEJM press, published November 11, 2023:
Restrictive or Liberal Transfusion Strategy in Myocardial Infarction and Anemia (Carson, Brooks, Hebert, et al Myocardial Ischemia and Transfusion (MINT) Investigators)
3504 pateints were included in this study. A primary-outcome event occurred in 295 of 1749 patients (16.9%) in the restrictive-strategy group and in 255 of 1755 patients (14.5%) in the liberal-strategy group. More specifically, death occurred in 9.9% of the patients with the restrictive strategy and in 8.3% of the patients with the liberal strategy; myocardial infarction occurred in 8.5% and 7.2% of the patients, respectively.
Conclusions from the study: Liberal transfusion strategy did NOT significantly reduce the risk of recurrent MI or death at 30 days.
N Engl J MedCarson JL, Brooks MM, Hébert PC, et al. Restrictive or Liberal Transfusion Strategy in Myocardial Infarction and Anemia. . Published online November 11, 2023. doi:10.1056/NEJMoa2307983
Category: Trauma
Keywords: Geriatric, trauma, mortality, risk factors (PubMed Search)
Posted: 11/26/2023 by Robert Flint, MD
(Updated: 2/2/2026)
Click here to contact Robert Flint, MD
A chart review of 1300 patients over age 65 admitted to the trauma service, arrived as a trauma activation, or had an injury severity score over 12 over a 6 year period looking at 30 day mortality found:
"five factors associated with increased 30-day mortality in older trauma patients: GCS < 15, ISS > 15, age ≥ 85 years, anticoagulation, and multimorbidity."
Fall from standing was the leading cause of trauma
Again, fragility is the index we should be using, not age alone. This study is limited in its retrospective chart review nature. Prospective research in the area of geriatric trauma is needed. Until then, assess those over age 65 for risk factors associated with fragility and treat accordingly.
Yadav, K., Lampron, J., Nadj, R. et al.Predictors of mortality among older major trauma patients. Can J Emerg Med 25, 865–872 (2023). https://doi.org/10.1007/s43678-023-00597-w
Category: Orthopedics
Keywords: foot injury (PubMed Search)
Posted: 11/25/2023 by Brian Corwell, MD
Click here to contact Brian Corwell, MD
The fleck sign of the foot is a small bony fragment seen in the Lisfranc joint space.
The space between the bases of the first and second metatarsal
This finding is associated with an avulsion of the Lisfranc ligament
Lisfranc Injuries
Category: Critical Care
Posted: 11/23/2023 by William Teeter, MD
Click here to contact William Teeter, MD
https://pubmed.ncbi.nlm.nih.gov/37142091/
Category: Trauma
Keywords: Geriatric, older person, trauma, super-geriatric (PubMed Search)
Posted: 11/23/2023 by Robert Flint, MD
(Updated: 2/2/2026)
Click here to contact Robert Flint, MD
This retrospective study looked at trauma patients over age 65 and divided them into age ranges 65-80 (geriatric) and 80 plus (super-geriatric). They then looked at mechanusm of injury, mortality, interventions,etc. What they found was ages 65-80 were more likely to be injured in motor vehicle crashes vs. falls for those over 80. Those over 80 received less interventions including hemmorhage control surgery and had much higher levels of withdrawal of care.
This study highlights that the geriatric population is not as a monolithic group over age 65, but more nuanced by various age ranges over 65. Research going forward should be adjusted to these nuanced age ranges. Out treatment approaches should be adjusted in geriatric vs. super-geriatric patients as well.
El-Qawaqzeh K, Anand T, Alizai Q, Colosimo C, Hosseinpour H, Spencer A, Ditillo M, Magnotti LJ, Stewart C, Joseph B. Trauma in the Geriatric and the Super-Geriatric: Should They Be Treated the Same? J Surg Res. 2024 Jan;293:316-326. doi: 10.1016/j.jss.2023.09.015. Epub 2023 Oct 6. PMID: 37806217.
Category: Administration
Keywords: boarding, administration, crowding (PubMed Search)
Posted: 11/22/2023 by Mercedes Torres, MD
(Updated: 2/2/2026)
Click here to contact Mercedes Torres, MD
A recently published study of ED APPs, residents, attendings, and nurses attempted to assess clinician's perspectives on how ED boarding impacts ED staff and patients. Authors performed a survey followed by focus group sessions to obtain qualitative insignts from participants.
All respondents associated boarding with feelings of burnout and self-reported poor satisfaction with communication and the process of boarding care.
Several key themes emerged which are outlined below:
This publication highlights the negative workforce and patient safety effects of ED boarding. It amplifies the voices of our colleagues who work towards change to improve both the health of our wrokforce as well as that of our patients and the communities that we serve.
Loke D, et al. Clinicians’ Insights on Emergency Department Boarding: An Explanatory Mixed Methods Study Evaluating Patient Care and Clinician Well-Being. The Joint Commission Journal on Quality and Patient Safety 2023; 000:1-8.
Category: Pediatrics
Keywords: POCUS, Pediatrics, Lung Ultrasound, Bronchiolitis (PubMed Search)
Posted: 11/20/2023 by Alexis Salerno Rubeling, MD
Click here to contact Alexis Salerno Rubeling, MD
Acute bronchiolitis (AB) is a common cause of respiratory tract infections in infants. A recent study looked at the application of Point-of-Care Lung Ultrasound (LUS) in infants <12 months who presented with symptoms of AB.
They scored infant lungs using a cumulative 12-zone system. With the below scale:
0 - A lines with <3 B lines per lung segment.
1 - ≥3 B lines per lung segment, but not consolidated.
2 - consolidated B lines, but no subpleural consolidation.
3 - subpleural consolidation with any findings scoring 1 or 2.
They found that infants with higher LUS scores had increased rates of hospitalization and length of stay.
Here are some tips for ultrasounding a pediatric patient:
Smith JA, Stone BS, Shin J, Yen K, Reisch J, Fernandes N, Cooper MC. Association of outcomes in point-of-care lung ultrasound for bronchiolitis in the pediatric emergency department. Am J Emerg Med. 2023 Oct 21;75:22-28. doi: 10.1016/j.ajem.2023.10.019. Epub ahead of print. PMID: 37897916.
Category: Trauma
Keywords: Reverse shock index, Peds trauma, prediction (PubMed Search)
Posted: 11/18/2023 by Robert Flint, MD
Click here to contact Robert Flint, MD
This small study suggests using reverse shock index times the Glasgow Comma Scake score may give a prognostication on pediatric trauma severity and resource utilization.
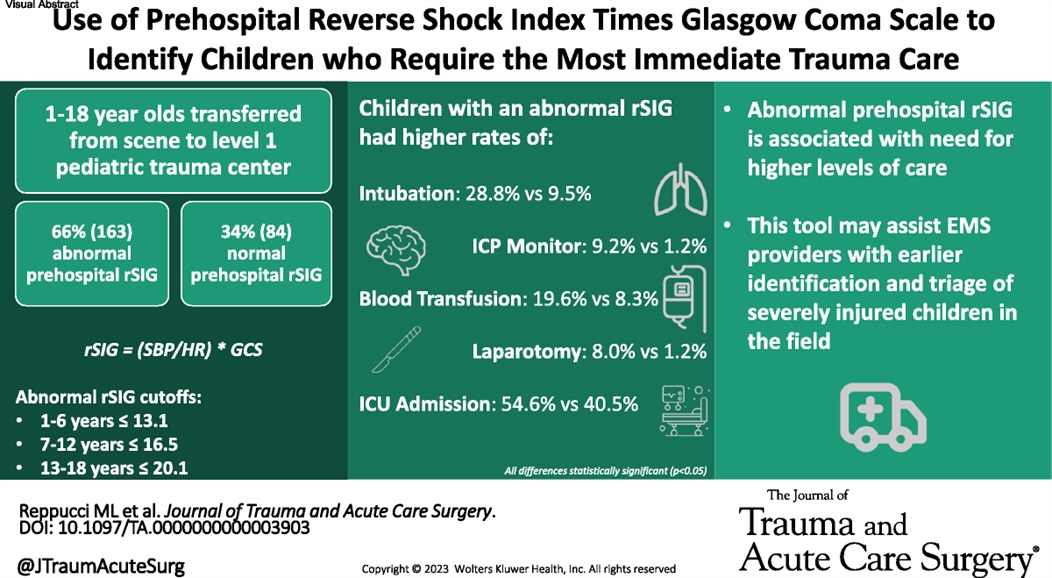
Reppucci, Marina L. MD; et al.
Journal of Trauma and Acute Care Surgery 95(3):p 347-353, September 2023. | DOI:
Category: Pediatrics
Keywords: pediatric trauma, transport, time to destination (PubMed Search)
Posted: 11/17/2023 by Jenny Guyther, MD
(Updated: 2/2/2026)
Click here to contact Jenny Guyther, MD
Hosseinpour H. Interfacility Transfer of Pediatric Trauma to Higher Levels of Care: The Effect of Transfer Time and Level of Receiving Trauma Care. Journal of Trauma and Acute Care Surgery. Epub ahead of print.
Category: EMS
Keywords: mental health, excited delirium, agitation, sedation, ketamine (PubMed Search)
Posted: 11/15/2023 by Jenny Guyther, MD
(Updated: 2/2/2026)
Click here to contact Jenny Guyther, MD
Bourke et al. Acute Severe Behavioral Disturbance Requiring Parenteral Sedation in Pediatric Mental Health Presentations to Emergency Medical Services: A Retrospective Chart Review. Annals of Emergency Medicine. 2023; 1-13. epub ahead of print.
Category: Trauma
Keywords: Brain injury, ketamine ICP (PubMed Search)
Posted: 11/12/2023 by Robert Flint, MD
Click here to contact Robert Flint, MD
This pediatric ICU study measured ICP during and after ketamine infusion. There was no increase in ICP associated with the ketamine infusion. This small study adds to the data that ketamine is safe in pediatric brain injured patients.
Laws, Jennifer C. MD1; Vance, E. Haley DNP2; Betters, Kristina A. MD1; Anderson, Jessica J. PharmD3; Fleishman, Sydney BA4; Bonfield, Christopher M. MD2; Wellons, John C. III MD, MSPH2,5; Xu, Meng MS6; Slaughter, James C. DrPH6; Giuse, Dario A. Dr.Ing7; Patel, Neal MD, MPH5,7; Jordan, Lori C. MD, PhD8; Wolf, Michael S. MD1,2
Category: Orthopedics
Posted: 11/11/2023 by Brian Corwell, MD
Click here to contact Brian Corwell, MD
https://prod-images-static.radiopaedia.org/images/626179/d58f35a8aa4a0a6750a6adce4087a4_gallery.jpg
"I was kicked in the inside of my knee while it was straight (extended). Look at the x-ray and tell me if its bad"
The arcuate sign
Avulsion fracture of the styloid of the proximal fibula. The fragment is usually small (less than 1 cm) and displaced superiorly and medially. This fracture pattern is pathognomonic for posterolateral corner (PLC) injury.
Treatment in ED is knee immobilization in full extension. Refer to orthopedics for PCL reconstruction.
Category: Critical Care
Keywords: Pneumonia, Corticosteroids, Steroids, Respiratory Failure, Infection (PubMed Search)
Posted: 11/9/2023 by Mark Sutherland, MD
Click here to contact Mark Sutherland, MD
For the folks who have been in practice for a while, you may be aware of the roller-coaster evidence base looking at steroids for pneumonia. Once thought to be beneficial and clearly indicated, of late steroids for pneumonia have fallen out of favor. Hamad et al have published an excellent (and brief) review in Clinical Infectious Diseases which suggests the pendulum might be swinging back in favor of giving steroids to patients with pneumonia. It's a ~5 minute read, so I recommend glancing through it yourself, but below are my two cents (solely my opinion) on where we are with steroids for pneumonia.
Take Home Points (OPINION ALERT):
1) When you have a condition present that you consider an indication for steroids (e.g. severe COVID-19 for sure; septic shock, s. pneumo infection, and ARDS depending on how you feel about the existing literature) --> strongly consider giving steroids unless there's a contraindication
2) When you have an undifferentiated patient who MAY have one of these conditions (e.g. pneumonia with COVID pending, patient potentially in ARDS or high risk of going into ARDS, etc) who is very sick --> it is reasonable to give steroids (if no contraindication) or not give steroids. My tendency is to lean towards giving steroids in these cases, but do be aware that society guidelines recommend against steroids here (although debatable if they just haven't caught up to more recent literature)
3) When you have an undifferentiated patient who may have one of these conditions, but is NOT very sick --> I do not think there is significant enough evidence to support empiric steroids
4) Factors that might push you one way or another:
Category: Gastrointestional
Keywords: NG Tube (PubMed Search)
Posted: 11/9/2023 by Neeraja Murali, DO, MPH
Click here to contact Neeraja Murali, DO, MPH
Think before placing a nasogastric tube!
Multiple articles which discussed complications of NGT placement were included in this integrative review, with the majority (n=67) publishing results in English. The authors categorized adverse events into two broad categories:
1) Mechanical adverse events - including respiratory, esophageal, and pharyngeal complications, obstructed tube, intestinal and intracranial (!) perforation, and tube withdrawal
-The largest cohort (n=44) was respiratory, with displacement or placement of tube to the respiratory tract
2) Others - pressure injury and misconnection
-One study showed pressure related injury in 25%, and 5 articles discussed complications of misconnection (including extravasation of gastric fluids and inadvertent connection to central venous catheters)
16 of the 69 studies reported death as a consequence of improper placement.
One big takeaway: there is no universally accepted standard for verificaiton of tube placement. Xray is considered to be *most* accurate. Tubes should also be checked periodically and depth should be marked. Evidence-based guidelines need to be developed to improve patient safety, outcomes, and quality of care.
Motta APG, Rigobello MCG, Silveira RCCP, Gimenes FRE. Nasogastric/nasoenteric tube-related adverse events: an integrative review. Rev Lat Am Enfermagem. 2021 Jan 8;29:e3400. doi: 10.1590/1518-8345.3355.3400. PMID: 33439952; PMCID: PMC7798396.
Category: Trauma
Keywords: ECMO, Trauma, Survivial (PubMed Search)
Posted: 10/14/2023 by Robert Flint, MD
(Updated: 2/2/2026)
Click here to contact Robert Flint, MD
This systematic review and analysis found in 1822 trauma patients treated with ECMO:
-Overall 66% survival to discharge
-VV ECMO was significantly superior to VA ECMO
-Mean age was 35 years. Typical of ECMO use in trauma is younger healthier patients are chosen to receive ECMO
“ECMO is not a routine life-saving intervention following trauma, but rather a salvage therapy that effectively replaces conventional treatment for young, healthy patients when conventional methods fail. Its complexity requires a multidisciplinary healthcare team and sufficient resources for optimal implementation.”
Zhang et al. European Journal of Medical Research (2023) 28:412 https://doi.org/10.1186/s40001-023-01390-2
Category: Quality Assurance/Quality Improvement
Keywords: Medication Errors, Pharmacy (PubMed Search)
Posted: 11/4/2023 by Brent King, MD
(Updated: 2/2/2026)
Click here to contact Brent King, MD
Spanish investigators conducted a 6-month, prospective, observational study to determine the impact of emergency department pharmacists on medication errors. They specifically focused on so called "High Alert" medications and on errors that, if undetected prior to administration, were likely to have serious deleterious consequences.
Over the course of the study, the pharmacists reviewed the medication records and histories of nearly 3000 patients. The pharmacists intervened in the care of 557 patients. Errors were most often detected during the process of medication reconcilliation. Over half of the potential errors were considered "severe" and the majority of pharmacist interventions were deemed important to the patient's care. Many of the medication errors detected involved "High Alert" medications.
The Bottom Line: Pharmacists are integral members of a high-functioning emergency department team. Their specialized knowledge contributes to a safe and effective care environment.
Perez-Moreno MA, Rodriguez-Camacho JM, Calderon-Hernandez B, et al. Clinical relevance of pharmacist intervention in an emergency department. Emerg Med J. 2017;34:495-501. doi:10.1136/emermed-2015-204726.
Category: EMS
Keywords: Stroke, EMS, medical record linkage, prehospital (PubMed Search)
Posted: 11/3/2023 by Ben Lawner, MS, DO
Click here to contact Ben Lawner, MS, DO
BACKGROUND: Prehospital (EMS) clinicians are positioned on the front lines of health care. With respect to stroke identification and treatment, early recognition is essential to positive outcomes. Considerable variability exists within EMS documentation. Despite considerable variability in documentation, the establishment and tracking of core stroke metrics serves as a benchmark to gauge performance and outline strategies for improvement.
METHODS: Authors conducted a retrospective, observational analysis of EMS encounters (2018-2019) which ultimately received a diagnosis of an "acute cerebrovascular event." Hospital based diagnoses included: hemorrhagic stroke, ischemic stroke, or transient ischemic attack. The data set was comprised of a statewide EMS documentation and a state wide acute stroke registry. Authors examined compliance with six core performance metrics which included measurement of blood glucose, documentation of last known well time, and on-scene time < 15 mins for patients with suspected stroke. During the 18 month study, almost 6000 encounters met criteria for inclusion.
RESULTS: EMS documentation remains a significant source of variability. EMS crews were largely compliant with blood glucose measurement. However, last known well time had the lowest (24%) documentation rate. Patients diagnosed with subarachnoid hemorrhage had the lowest rate of compliance with metrics.
BOTTOM LINE: Accurate prehospital stroke diagnosis remains a challenge. Consistent data collection and benchmarking remains an important first step in the evaluation of performance. Higher NIHSS scores and ischemic strokes are linked to higher rates of metric compliance.
Oostema JA, Nickles A, Luo Z, Reeves MJ. Emergency Medical Services Stroke Care Performance Variability in Michigan: Analysis of a Statewide Linked Stroke Registry. J Am Heart Assoc. 2023 Jan 3;12(1):e026834. doi: 10.1161/JAHA.122.026834. Epub 2022 Dec 20. PMID: 36537345; PMCID: PMC9973590.
Category: Pediatrics
Keywords: Neonate, Newborn, resuscitation, NRP (PubMed Search)
Posted: 11/3/2023 by Kelsey Johnson, DO
(Updated: 2/2/2026)
Click here to contact Kelsey Johnson, DO
Term? Tone? Tantrum?
Immediately after delivery, your initial neonatal assessment should evaluate for:
- Appearance of full or late pre-term gestation (>34 weeks)
- Appropriate tone (flexed extremities, not floppy)
- Good cry and respiratory effort
Newborns meeting this criteria should not require resuscitation. They can be placed skin to skin on mother and allowed to breastfeed. Delayed cord clamping for 60 seconds is recommended, as data shows improved neurodevelopmental outcomes and iron stores in first year of life.
Neonates not meeting these criteria should be brought to the warmer for resuscitation, with the focus being on:
- Warm - via radiant warmer. Maintain temps 36.5 C – 37.5 C
- Dry - Neonates have thin skin and lose heat readily from evaporative loses
- Stim - tactile stimulation on the head, midline of the back and extremities to provoke a cry and encourage respiratory effort
Avoid routinely bulb-suctioning unless there is significant obstructing mucous, as this can increase vagal tone and result in bradycardia. If bulb suctioning is used, first suction the mouth before the nose.
Majority of resuscitations do not require additional support, however if heart rate is <100 or there is poor respiratory effort, the physician should initiate PPV.
PPV settings: PIP 20 PEEP 5 FiO2 21% Rate of 60 breaths per minute
Improvement in the neonate’s HR is the primary indicator of effective PPV!
If HR poorly responding (remains <100), ensure appropriate mask size, reposition, suction, and increase PIP (max 35) and FiO2.
If HR drops below 60, intubate with uncuffed ETT
- Prioritize adequate ventilation as this is the highest priority in neonatal resuscitation
- Initiate compressions at rate of 120/min.
- Epi dosing is 0.01-0.03 mg/kg q3-5 min
- ETT size estimation by gestational age:
25 weeks = 2.5, 30 weeks = 3.0, 35 weeks = 3.5, 40 weeks = 4.0
