Category: Trauma
Keywords: Spleen, trauma, spleen injury grades (PubMed Search)
Posted: 8/19/2023 by Robert Flint, MD
(Updated: 2/2/2026)
Click here to contact Robert Flint, MD
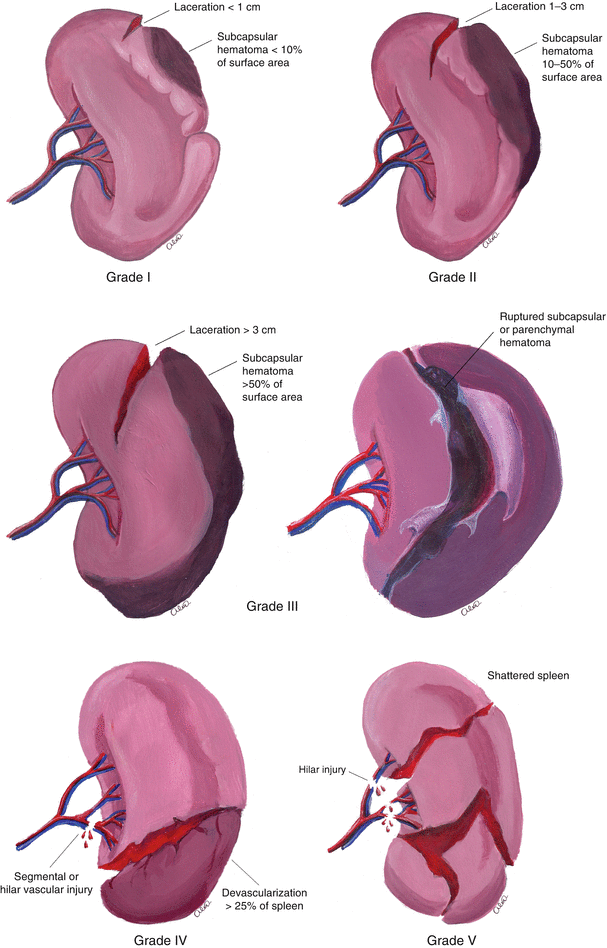
Splenic injury treatment depends on the grade of injury. In general, grades 1 and 2 are non-operatively managed. Grades 4 and 5 tend to be managed operatively. Interventional radiology is used commonly for grade 3 and grades 1 and 2 if active contrast extravasation is seen. Below is a refresher on splenic injury grading.
Table 1
Adaptation of AAST Organ Injury Scale for Spleen
| Grade | Injury type | Description of injury |
|---|---|---|
| I | Hematoma | Subcapsular, <10% surface area |
| II | Hematoma | Subcapsular, 10% to 50% surface area |
| Laceration | Capsular tear, 1 cm to 3 cm parenchymal depth that does not involve a trabecular vessel | |
| III | Hematoma | Subcapsular, >50% surface are or expanding: ruptured subcapsular or parenchymal hematoma: intraparenchymal hematoma_>5 cm or expanding |
| IV | Laceration | Laceration involving segmental or hilar vessels producing major devascularization (>25% of spleen) |
| V | Laceration | Completely shattered spleen |
1. An update on nonoperative management of the spleen in adults. BMJ Trauma Surgery and Acute Care Open. Volume 2, Issue 1. Ben L Zarzaur, Grace S Rozycki
2. https://www.google.com/search?q=splenic+laceration+grading&rlz=1C9BKJA_enUS1063US1063&oq=splenic+laceration+grading&aqs=chrome..69i57j0i512l3j0i22i30l6.9531j0j4&hl=en-US&sourceid=chrome-mobile&ie=UTF-8#vhid=0ARTxhEO89dgGM&vssid=l
Category: Pediatrics
Keywords: Drowning, near drowning, CXR (PubMed Search)
Posted: 8/18/2023 by Jenny Guyther, MD
(Updated: 2/2/2026)
Click here to contact Jenny Guyther, MD
This was a retrospective study involving several hospitals in Italy. 135 patients who had drowned (the term used in the article) were included. 4.5% of patients died. Most drowning occurred in July and August. The most common comorbidity was epilepsy in about 10% of patients. Several patients were also witnessed to have trauma and syncope. Early resuscitation, either by bystanders or trained professionals, was paramount in survival.
Children who are conscious at presentation and have mild or no respiratory distress have the best prognosis. A well appearing child should be observed for 6-8 hours, given that 98% of children will present with symptoms within the first 7 hours. A chest xray is not indicated in the asymptomatic patient. Patients who are submerged greater than 25 minutes or without ROSC after 30 minutes have a poor prognosis.
Bottom line: Never swim alone and everyone should be trained in bystander CPR.
Category: EMS
Keywords: Hands only CPR, bystander CPR, directions (PubMed Search)
Posted: 8/16/2023 by Jenny Guyther, MD
(Updated: 2/2/2026)
Click here to contact Jenny Guyther, MD
Bystander CPR increases out-of-hospital CPR survival and direction by 911 telecommunicators increases the frequency of bystander CPR. The majority of 911 centers use Medical Priority Dispatch System which walks 911 telecommunicators through a series of questions that give different instructions based on the caller's answers. Studies have shown out-of-hospital cardiac arrests are only recognized between 79-92% of the time and telecommunicator instructions for CPR can take between 176-285 seconds.
This study reviewed recorded 911 calls of patients who were found to be in cardiac arrest. Calls where the caller was not with the patient and confirmed overdoses were some of the call types that were excluded.
Out of 65 reviewed calls, 28% were not recognized during the actual call. When they were reviewed, 8/18 of the calls were deemed to be recognizable. Themes that were noted were: incomplete or delayed recognition assessment (ie uncertainty in breathing), communication gaps (callers were confused with instructions or questions), caller emotional distress, delayed repositioning for chest compressions, non essential questions and assessments, and caller refusal/hesitation or inability to act.
Bottom line: In addition to bystander CPR training, education on the process and questions involved in calling 911 could be helpful in an emergency.
Missel et al. Barriers to the Initiation of Telecommunicator-CPR during 911 Out-of-Hospital Cardiac Arrest Calls: A Qualitative Study. 2023. Prehospital Emergency Care.
Category: Critical Care
Posted: 8/15/2023 by Caleb Chan, MD
Click here to contact Caleb Chan, MD
Background:
There has been interest in vitamin C as an adjunctive therapy in patients with systemic inflammation and vasoplegia to reduce inflammation. While it was suggested that vitamin C may have some benefit (along with hydrocortisone and thiamine) in septic shock, the LOVIT trial showed possible harm from high-dose vitamin C administration in septic ICU patients. The VALENCIA trial sought to evaluate whether vitamin C could reduce the duration of vasopressor therapy in patients with moderate vasoplegic shock.
Study:
-double-blinded RCT at two tertiary centers, 71 patients (36 to placebo, 35 to vitamin C)
-adult patients with vasoplegic shock of any cause
-vasopressor requirement >10 μg/min of norepi after hypovolemia was excluded
-notable exclusion criteria: end-stage renal failure and expected survival <12 hrs
Results:
-65 pts with septic shock, 6 pts with non-infectious cause
-no significant difference in the duration of vasopressors between the treatment group (median, 44 h [95% CI, 37-54 hrs]) and the control group (55 hrs [95% CI, 33-66 hrs])
-also no statistically significant difference in the vasopressor dose at 12 hourly time points, ICU or 28-day mortality and ICU or hospital length of stay
Take-home points:
Small study that ultimately may be under-powered but did not show that vitamin C reduces vasopressor duration in moderate vasoplegic shock
Anstey MH, Aljeaidi MS, Palmer R, et al. Intravenous vitamin C for vasoplegia: A double-blinded randomised clinical trial (VALENCIA trial). Journal of Critical Care. 2023;78:154369.
Category: Gastrointestional
Keywords: Appendicitis (PubMed Search)
Posted: 8/13/2023 by Neeraja Murali, DO, MPH
(Updated: 2/2/2026)
Click here to contact Neeraja Murali, DO, MPH
In recent years, there has been an uptick in non-operative management of acute appendicitis. This study examins outcomes in older patients (>65 years old).
The study authors evaluated retrospective data and included 474845 patients in the US with acute uncomplicated appendicitis betwen 10/2021 and 04/2022. All participants survived at least 24 hours postoperatively and none carried a diagnosis of inflammatory bowel disease; there were 43,846 patients treated nonoperatively and 430,999 who underwent appendectomy. The primary outcome was incidence of post-treatment complications, with secondary outcomes of mortality, length of stay, and inpatient costs.
In patients 65+, there was a 3.72% decrease in risk of complications, 1.82% increase in mortality, and increased LOS and costs.
Ultimately, operative management of acute appendicits was associated with reduced mortality, length of stay, and costs across all adult patients. While nonoperative management remains an option in the treatment of acute appendicits, surgical management continues to be the accepted standard.
Meier J, Stevens A, Bhat A, Berger M, Balentine C. Outcomes of Nonoperative vs Operative Management of Acute Appendicitis in Older Adults in the US. JAMA Surg. 2023;158(6):625–632. doi:10.1001/jamasurg.2023.0284
Category: Administration
Keywords: Exercise, health, cardiovascular mortality (PubMed Search)
Posted: 8/12/2023 by Brian Corwell, MD
(Updated: 2/2/2026)
Click here to contact Brian Corwell, MD
The WHO and the US Department of Health and Human Services, among other groups, recommend between 150-300 minutes of moderate intensity or 75 to 150 minutes of vigorous intensity physical activity per week.
This could add up to almost 45 minutes a day!
Who has the time for that?
This is an extremely challenging goal with work and other life responsibilities.
Some recent studies asked whether routinely cramming the recommended weeks’ worth of physical activity into a couple of days, weekend warriors (WW), leads to the same life-extending benefits as distributing the exercise load throughout the week.
In a retrospective analysis of almost 90,000 individuals (56% women), providing a week of accelerometer-based physical activity data: Three activity patterns were compared: active weekend warrior (active WW, ≥150 minutes with ≥50% of total achieved in 1-2 days), active regular (≥150 minutes and not meeting active WW status), and inactive (<150 minutes).
A weekend warrior (WW) pattern of physical activity was associated with similarly lower risks of cardiovascular outcomes (incident atrial fibrillation, myocardial infarction, heart failure, and stroke) compared with more evenly distributed physical activity.
Another large prospective cohort study of over 350,000 US adults (51% women) did not find any significant difference in mortality rates between weekend warriors and regularly active participants. Compared with physically inactive participants, active participants (both weekend warrior and regularly active) had lower all-cause and cause-specific mortality rates.
Take home: Any exercise is better than none. Adults who perform 150 minutes or more of moderate to vigorous physical activity (or 75 minutes of vigorous activity) per week may experience similar health benefits whether the sessions are spread throughout the week or concentrated in a weekend.
Note: Being a weekend warrior can increase the risk of MSK complications and injury..
Future studies should include the use of wearable devices and not rely on self-reporting exercise behavior.
1. Khurshid S, Al-Alusi MA, Churchill TW, Guseh JS, Ellinor PT. Accelerometer-Derived “Weekend Warrior” Physical Activity and Incident Cardiovascular Disease. JAMA. 2023;330(3):247–252.
2. dos Santos M, Ferrari G, Lee DH, et al. Association of the “Weekend Warrior” and Other Leisure-time Physical Activity Patterns With All-Cause and Cause-Specific Mortality: A Nationwide Cohort Study. JAMA Intern Med. 2022;182(8):840–848.
Category: Pharmacology & Therapeutics
Keywords: Tenecteplase, Pulmonary Embolism, Cardiac Arrest (PubMed Search)
Posted: 8/10/2023 by Wesley Oliver
Click here to contact Wesley Oliver
ACLS guidelines state that thrombolytics may be considered for suspected pulmonary embolism during cardiac arrest. There is limited data supporting the recommendation; however, it is noted that the benefits likely outweigh the risks. There is also no consensus on the appropriate thrombolytic timing, drug, or dose.
Our institution recently implemented the use of tenecteplase for acute ischemic stroke, ST-elevation myocardial infarction (STEMI), and pulmonary embolism (PE). When using tenecteplase for suspected PE during cardiac arrest, we use the same weight-based dose used for STEMIs. We include a label on the outside of the tenecteplase box that lists all the doses for the various indications.
Tenecteplase Dose
<60 kg: 30 mg
≥60 to <70 kg: 35 mg
≥70 to <80 kg: 40 mg
≥80 to <90 kg: 45 mg
≥90 kg: 50 mg
The tenecteplase dose is administered as an IV bolus over 5 seconds.
There is also limited data for the duration of CPR after thrombolytic administration, with no recommendations being made in most literature. Our current institutional guidelines recommend to consider continuing CPR for 60-90 minutes before resuscitation efforts are terminated. The only guideline that makes any mention of duration of CPR is the European Resuscitation Council Guidelines 2021, which makes the same recommendation.
Berg KM, Soar J, Andersen LW, et al. Adult Advanced Life Support: 2020 International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science with Treatment Recommendations. Circulation. 2020; 142(suppl 1):S92-139.
Lavonas EJ, Drennan IR, Gabrielli A, et al. Part 10: special circumstances of resuscitation: 2015 American Heart Association guidelines update for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2015; 132(suppl 2):S501-S518.
Lott C, Truhlá A, Alfonzo A, et al; ERC Special Circumstances Writing Group Collaborators. European Resuscitation Council Guidelines 2021: Cardiac arrest in special circumstances. Resuscitation. 2021 Apr;161:152-219.
TNKase (tenecteplase) [prescribing information]. South San Francisco, CA: Genentech; March 2023.
Category: Critical Care
Posted: 8/8/2023 by William Teeter, MD
Click here to contact William Teeter, MD
Targeted Therapeutic Mild Hypercapnia after Resuscitated Cardiac Arrest (TAME)
Current guidelines recommend normocapnia for out-of-hospital cardiac arrest (OHCA), the TAME Study asked is mild hypercapnia better?
Conclusion: "In patients with coma who were resuscitated after out-of-hospital cardiac arrest, targeted mild hypercapnia did not lead to better neurologic outcomes at 6 months than targeted normocapnia."
https://www.nejm.org/doi/full/10.1056/NEJMoa2214552
https://clinicaltrials.gov/study/NCT03114033
https://www.thebottomline.org.uk/blog/ebm/tame/
Category: Ophthamology
Keywords: POCUS, Ocular, Posterior Chamber (PubMed Search)
Posted: 8/7/2023 by Alexis Salerno Rubeling, MD
Click here to contact Alexis Salerno Rubeling, MD
Prior research has shown that EPs can accurately detect ocular pathology using POCUS.
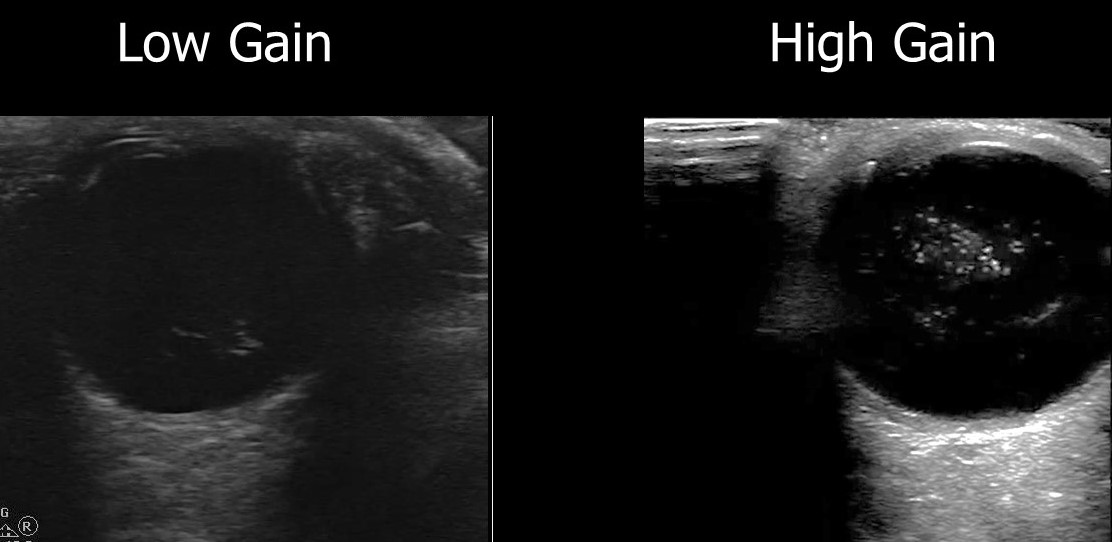
A recent retrospective review looked at how ultrasound image gain levels impacted the accuracy of POCUS for detection of retinal detachment, retinal hemorrhage and posterior vitreous detachment.
They included 383 ED patients who received ocular POCUS and ophthalmology consultations.
Conclusions: The authors found that increasing the gain for ocular POCUS images allowed for increased sensitivity.
Here is an example of a vitreous hemorrhage on ocular POCUS using low gain and high gain.
Chang M, Finney N, Baker J, Rowland J, Gupta S, Sarsour R, Saadat S, Fox JC. Optimal Image Gain Intensity of Point-of-care Ultrasound when Screening for Ocular Abnormalities in the Emergency Department. West J Emerg Med. 2023 May 5;24(3):622-628. doi: 10.5811/westjem.59714.
Category: Quality Assurance/Quality Improvement
Keywords: Physician Burnout, Quality of Care, Professionalism (PubMed Search)
Posted: 6/13/2023 by Brent King, MD
(Updated: 6/19/2023)
Click here to contact Brent King, MD
Takeaways: Physicians who have symptoms of burnout as measured by standard burnout scales are more likely to be involved in patient safety incidents, more likely to be cited for poor professionalism, and more likely to have lower patient satisfaction scores. They are also more likely to leave their jobs, experience career regret, and experience job dissatisfaction/ The risk of burnout is highest among emergency physicians and intensivists.
In this systematic review and meta analysis, the authors reviewed 170 qualitative and quantitative studies including 239,246 physicans to determine the impact of physician burnout on a variety of issues including, quality of care delivered, perception of professionalism, patient satisfaction, and career engagement.
As compared to physicians who did not report symptoms of burnout, burned-out physicians were about four times more likely to be unhappy in their jobs and three times more likely to regret their career decision and to express an intention to leave their jobs.Physician burnout doubled the likelihood of involvement in a patient safety incident and made it three times more likely that the physician would be cited for unprofessional behavior. Burned out physicians were also three times more likely to have low patient satisfaction scores.
Burned-out physicians in their 20's and 30's were particularly at risk for involvement in patient safety incidents and burned-out trainees were more often cited for poor professionalism than older physicians, especially those in their 50's and beyond.
The bottom line: Physican burnout is a serious and growing problem. It has numerous potentially serious consequences for both physicians and patients. Physicians working in high-pressure specialties like emergency medicine and critical care have the highest risk for burnout.
Hodkinson A, Zhou A, Johnson J, et al. Associations of physician burnout with career engagement and quality of patient care: systematic review and meta-analysis. BMJ 2022;378:e070442. (http://dx.doi.org/10.1136/bmj-2022-070442)
Category: EMS
Keywords: Cardiac arrest, resuscitation, emergency medical services (PubMed Search)
Posted: 8/2/2023 by Ben Lawner, MS, DO
Click here to contact Ben Lawner, MS, DO
There is room for improvement with respect to rates of meaningful neurological survival in patients experiencing out of hospital cardiac arrest. Post resuscitation blood pressure goals remain a matter of debate. Though a MAP of >65 mm Hg is often cited as "desirable" in the post cardiac arrest setting, some experts have advocated for a higher MAP goal to increase cerebral perfusion pressure and improve outcomes.
This study was a retrospective review and meta-analysis that examined post cardiac arrest patients with MAP goals < 70 mm Hg and > 70 mm Hg. Over 1000 patients were included in the final meta-analysis. The primary outcome was pooled mortality. Secondary outcomes included neurologically meaningful survival, dysrhythmia, and acute kidney injury. The study detected no statistically significant difference in survival. Neurological outcomes were also similar between the two groups of resuscitated patients with out of hospital cardiac arrest. However, the study revealed statistically significant decreases in ICU length of stay and mechanical ventilation time.
As with any retrospective review, there are important limitations to consider. Among them: Few RCTs were included and all of them were conducted in European countries. Generalizability may be limited given the differences in emergency medical services systems and resuscitation protocols.
Study authors recommend tailoring resuscitation goals to the individual patient since arrest physiology, comorbidities, and other factors influence a patient's post cardiac arrest course.
Bottom line:
There is insufficient evidence to recommend arbitrary MAP goals in patients resuscitated from out of hospital cardiac arrest.
Lim SL, Low CJW, Ling RR, Sultana R, Yang V, Ong MEH, Chia YW, Sharma VK, Ramanathan K. Blood Pressure Targets for Out-of-Hospital Cardiac Arrest: A Systematic Review and Meta-Analysis. J Clin Med. 2023 Jul 5;12(13):4497. doi: 10.3390/jcm12134497. PMID: 37445530; PMCID: PMC10342823.
Category: Obstetrics & Gynecology
Keywords: POCUS, OB, Ectopic Pregnancy (PubMed Search)
Posted: 7/31/2023 by Alexis Salerno Rubeling, MD
Click here to contact Alexis Salerno Rubeling, MD
Ectopic pregnancy ranges from 3 to 13% in symptomatic first-trimester ED patients.
The discriminatory zone is defined as the level of Bhcg above which an intrauterine pregnancy can be reliably detected using ultrasound. (1,500 mIU/mL for transvaginal ultrasound and 3,000 mIU/mL for transabdominal ultrasound)
One study found that an intrauterine pregnancy was visualized with as low as 1,440 mIU/mL and patients with an interdeterminate pelvic ultrasound who were found to have an ectopic pregnancy had a Bhcg greater than 3,000 mIU/mL only 35% of the time.
Bottom Line: If you have a symptomatic patient with an empty uterus and a bhcg above the discriminatory zone, they have a higher risk for ectopic pregnancy. However, if your patient is symptomatic, they should still have further evaluation for ectopic pregnancy even if they have a bhcg lower than the discriminatory zone.
Wang R, Reynolds TA, West HH, Ravikumar D, Martinez C, McAlpine I, Jacoby VL, Stein JC. Use of a β-hCG discriminatory zone with bedside pelvic ultrasonography. Ann Emerg Med. 2011 Jul;58(1):12-20. doi: 10.1016/j.annemergmed.2010.12.023. Epub 2011 Feb 18. PMID: 21310509.
Category: Airway Management
Keywords: major adverse event, airway, management, cardiovascular collapse (PubMed Search)
Posted: 7/30/2023 by Robert Flint, MD
(Updated: 2/2/2026)
Click here to contact Robert Flint, MD
This systemic review and meta analysis looked at major adverses events (hypoxia, cardiovascular instability, or cardiac arrest) in patients intubated in emergency departments, ICU’s, or medical floors. They found nearly 1/3 of patents had an event. ICU intubation and patients with pre-existing hemodynamic compromise had the highest rate of adverse outcomes. This study gives further support to the concept of maximizing resuscitation pre-intubation and to anticipate a major event peri-intubation. Be prepared and don't be surprised when something doesn't go as planned.
Category: Orthopedics
Keywords: Ortho, bohler angle, fracture. (PubMed Search)
Posted: 7/27/2023 by Robert Flint, MD
Click here to contact Robert Flint, MD
"The normal value for the Böhler angle is between 25° and 40° 1. Although there is wide variation between individuals, there is relatively little variation between the left and right feet of a single individual 2. A reduced Böhler angle can be seen in displaced intra-articular calcaneal fractures. The degree of reduction in the Böhler angle is an indicator of the severity of calcaneal injury, and the degree to which the Böhler angle is restored at surgery is correlated with functional outcome 3."
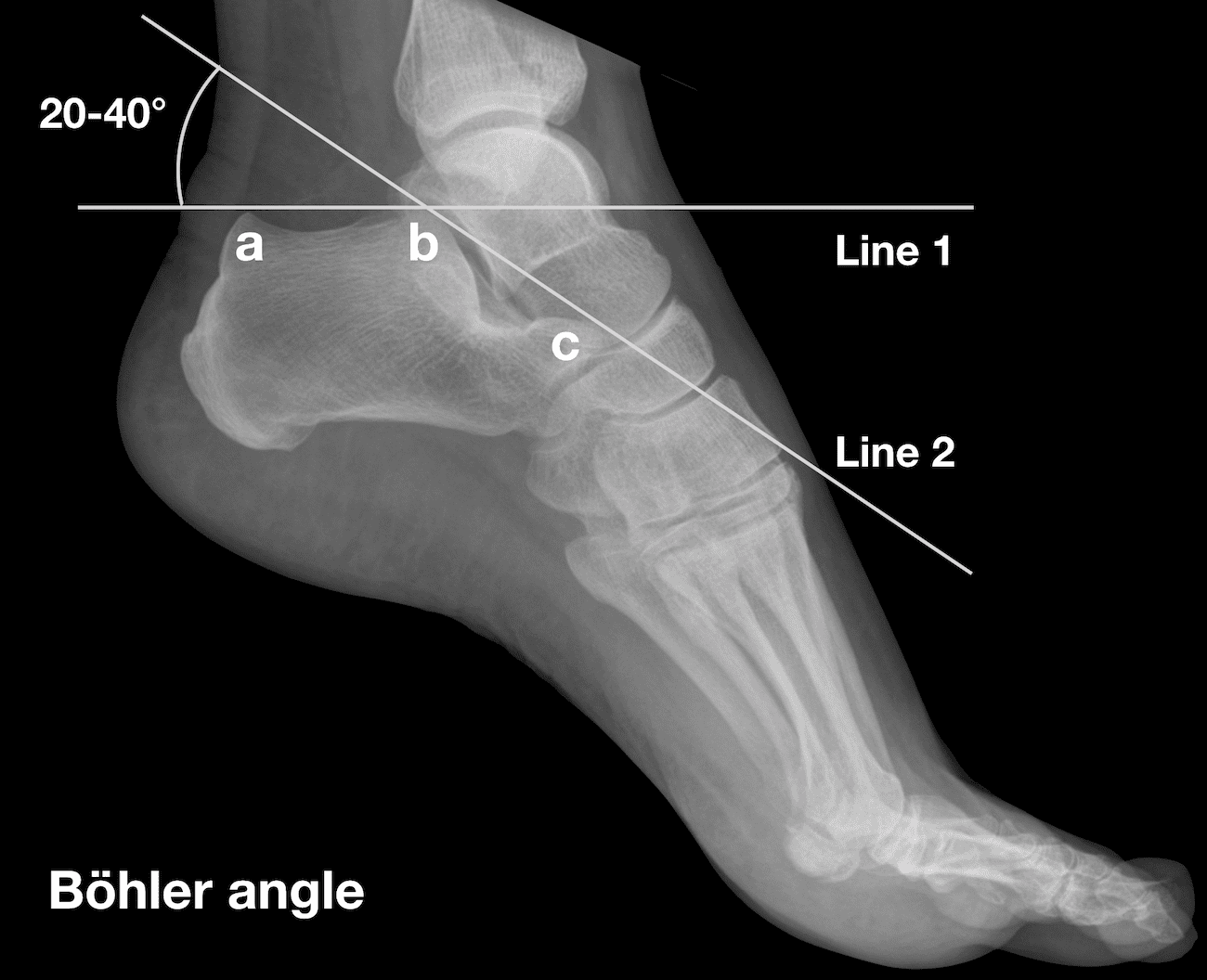
Amini B, Worsley C, Weerakkody Y, et al. Böhler angle. Reference article, Radiopaedia.org (Accessed on 27 Jul 2023) https://doi.org/10.53347/rID-1002
Category: Administration
Keywords: age, attrition, gender, workforce (PubMed Search)
Posted: 7/26/2023 by Mercedes Torres, MD
Click here to contact Mercedes Torres, MD
In a recent study of emergency physicians (EPs) who left the workforce between 2013 and 2020, authors sought to investigate their age and number of years since residency graduation for males and females.
A total of 25,839 (70.2%) male and 10,954 (29.8%) female EPs were included.
Female gender (adjusted odds ratio 2.30) was significantly associated with attrition from the workforce.
Of those who left the workforce, the median number of years after residency that males left was 17.5, as compared with only 10.5 years for females.
Furthermore, among those who exhibited attrition, one in 13 males and one in 10 females exited clinical practice within 5 years of residency graduation.
As authors emphasize, these data identify widespread gender-based disparities regarding EM workforce attrition that are critical to address to ensure stability, longevity, and diversity in the EP workforce.
Gettel CJ, Courtney DM, Agrawal P, et al. Emergency medicine physician workforce attrition
differences by age and gender. Acad Emerg Med. 2023;00:1- 9. doi:10.1111/acem.14764
Category: Critical Care
Keywords: OHCA, ROSC, cardiac arrest, resuscitation, CT, pan-scan, computed tomography (PubMed Search)
Posted: 7/25/2023 by Kami Windsor, MD
Click here to contact Kami Windsor, MD
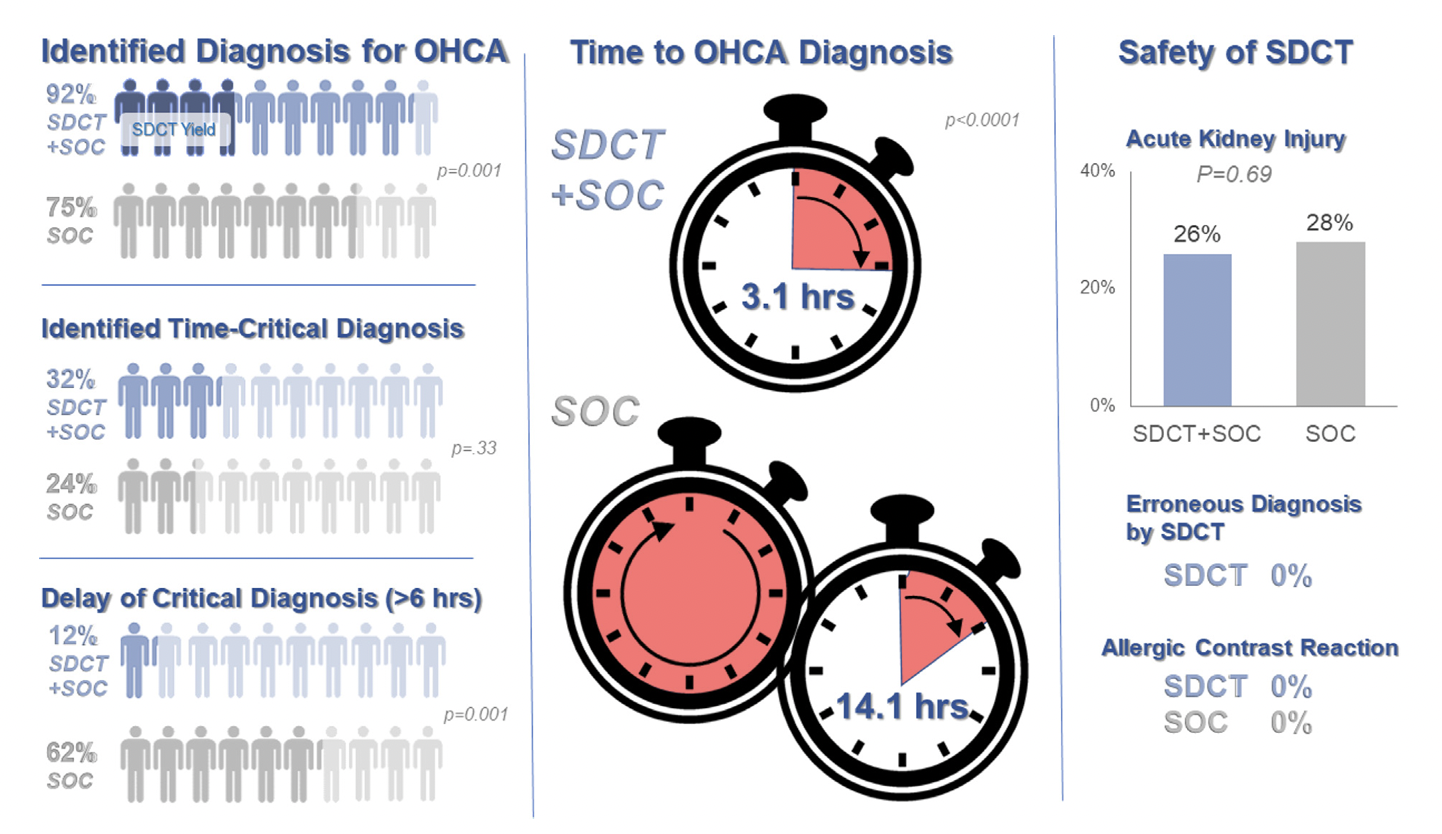
Background: Prior evidence1,2 has suggested that early “pan-scan” after ROSC provides clinically-relevant information that assists in the care of the patient in question, when the cause of OHCA is unclear.
The recent CT FIRST trial looked at patients pre- and post- implementation of a protocol for head-to-pelvis CT within 6 hours of ROSC for adult patients without known cause or evidence of possible cardiac etiology, stable enough for scan. *Patients with GFR <30 were excluded from assignment to CT, although were included in the post/CT cohort if their treating doctors ordered CT scans based on perceived clinical need. To balance this, a similar number of patients with GFR <30 were included in the pre/“standard of care” cohort.
Outcomes After Protocol (Pre- vs. Post-):
Bottom Line: Early pan-CT allows for earlier definitive diagnosis and stabilization without increase in adverse events. While this earlier diagnosis does not seem to yield better survival, earlier stabilization may provide some benefits in terms of resource allocation and disposition, a notable benefit during our current crisis of staffing shortages and ED boarding.
Category: Trauma
Keywords: radiology, transfer, trauma, imaging, rural (PubMed Search)
Posted: 7/23/2023 by Robert Flint, MD
(Updated: 2/2/2026)
Click here to contact Robert Flint, MD
Evaluating trauma patients at Level 3 or 4 centers, rural hospitals, and non-trauma centers is difficult. Understanding the amount of work-up to perform prior to transfer is important. Summers, et al suggest less is more when it comes to imaging. The receiving facility often repeats imaging leading to time delays, additional radiation exposure, and increased costs. Chest X-ray and FAST exam may be all that is indicated in centers that do not have the resources to care for injures identified on CT imaging prior to transfer.
Summers LN, Harry ML, Colling KP. Evaluating our progress with trauma transfer imaging: repeat CT scans, incomplete imaging, and delayed definitive care. Emerg Radiol. 2021 Oct;28(5):939-948. doi: 10.1007/s10140-021-01938-x. Epub 2021 May 28. PMID: 34050410.
Category: Orthopedics
Keywords: shoulder pain, labrum tear (PubMed Search)
Posted: 7/22/2023 by Brian Corwell, MD
(Updated: 2/2/2026)
Click here to contact Brian Corwell, MD
SLAP tear/lesion – Superior labral tear oriented anterior to posterior
Glenoid labrum – A rim of fibrocartilaginous tissue surrounding the glenoid rim, deepening the “socket” joint.
Integral to shoulder stability.
https://aosm.in/storage/2019/05/ch-shoulder-slap.jpg
O’Brien’s test aka active compression test for superior labral pathology.
2 parts – generally performed with the patient standing.
The patient’s shoulder is raised to 90 degrees with full elbow extension and approximately 30 degrees of adduction across the midline.
Resistance is applied, using an isometric hold.
Test in both full internal and external rotation
-This alters the position and rotation of the humerus against the glenoid
A positive test is when pain is elicited when the shoulder is in internal rotation with forearm pronation (thumb to floor) and much less or no pain when in external rotation (supination).
Note: AC joint pain may test similarly but will localize to different area of shoulder
The presence of similar, reproducible deep and diffuse glenohumeral joint pain is most indicative of a true positive test.
https://i0.wp.com/musculoskeletalkey.com/wp-content/uploads/2020/03/f50-02-9780323287845.jpg?w=960
Category: Administration
Keywords: racial disparity, substance use disorder (PubMed Search)
Posted: 7/22/2023 by Kevin Semelrath, MD
(Updated: 2/2/2026)
Click here to contact Kevin Semelrath, MD
Substance use disorder is now known to be a function of brain disease and not a moral failure. Patients with substance use disorder are highly complex and often use the ED at a higher frequency than those without the disorder. However, these patients are also frequently the target of implicit bias and stigmatizing behavior from the healthcare team that can lead to worsened outcomes. Add on top of that a racial disparity, and we can see how this group of patients can have really bad health outcomes.
This study looked at the length of time to treatment of patients with SUD, to see if there was a difference within this group based on racial or ethnic differences. It did find that black patients with SUD did wait on average 35% longer in the ED before being seen or treated. This difference was statistically significant.
While this study wasn't designed to identify the causes of such a disparity, it does raise concern for implicit bias being in effect among not only the healthcare workers, but ingrained into the healthcare systems themselves.
Patient's with SUD are a vulnerable group of patients, and black patients with SUD are experiencing a disparity in time to treatment. This should remind us all to seek out ways to remove these biases and disparities from the systems where we work.
Category: Pediatrics
Keywords: fever, limp, bacteremia, osteomyelitis, septic joint (PubMed Search)
Posted: 7/21/2023 by Jenny Guyther, MD
(Updated: 2/2/2026)
Click here to contact Jenny Guyther, MD
El Helou R, Landschaft A, Harper MB, Kimia AA. Bacteremia in Children With Fever and Acute Lower Extremity Pain [published online ahead of print, 2023 Apr 4]. Pediatrics. 2023;e2022059504. doi:10.1542/peds.2022-059504
