Category: Administration
Posted: 1/6/2024 by Robert Flint, MD
(Updated: 2/2/2026)
Click here to contact Robert Flint, MD
Since 2014, Medicare has payed for inpatient services for Medicare patients who’s admitting physician noted that hospital stay required at least 48 hours (measured as 2 midnights) or required specialty care that could not be performed as an out patient. This rule now will apply to Medicare Advantage insurance patients as well. Physicians will need to document their reasoning why a patient’s stay will likely require two midnights.
Jakob Emerson - Updated Friday, December 29th, 2023 Becker’s Payer Issues
Category: Critical Care
Posted: 1/2/2024 by Mark Sutherland, MD
Click here to contact Mark Sutherland, MD
As is well known, fluid resuscitation strategy ("liberal" vs “restrictive”) in sepsis is a controversial topic. An RCT in NEJM called CLOVERS that looked at this and found no difference was recently re-analyzed to answer the following question… should my choice of strategy change if the patient presents with an Acute Kidney Injury (AKI)?
For the most part, the answer is no. In the group with AKI, the restrictive group did slightly, but non-statistically-significantly, better. Interestingly, in the group without AKI, the relationship reversed, and in fact of the 4 groups (AKI vs no AKI, Restrictive vs Liberal), the no AKI but liberal strategy group did best (liberal vs restrictive in the no AKI group almost reached statistical significance in favor of the liberal strategy, but not quite).
Bottom Line: In septic patients presenting with an AKI, we don't know whether liberal or restrictive strategy is better, but either is probably reasonable. In patients presenting without an AKI, it may be more ok to lean more towards liberal fluid resuscitation than in non-AKI patients*.
*There are several important caveats here: 1) they didn't closely evaluate for potential side effects of over-resuscitation such as hypoxia or pulmonary edema (the primary outcome was need for renal replacement therapy), 2) as mentioned above, this trended towards but did not reach statistical significance, 3) this is one small study which did a subgroup secondary-analysis of a larger trial.
Category: Administration
Keywords: Personal growth. (PubMed Search)
Posted: 12/31/2023 by Robert Flint, MD
(Updated: 2/2/2026)
Click here to contact Robert Flint, MD
As the calendar flips to a new year, consider not setting goals or resolutions. Studies show unmet goals or having too many half finished projects leads to increased stress, anxiety and depression. Instead, consider approaching the new year looking for growth, introspection, and striving to achieve excellence. Understanding the why and what motivates you will lead to the correct what and how. Here are some questions to get you thinking about the why. May your New Year be filled with growth and excellence!
Category: Pharmacology & Therapeutics
Posted: 12/30/2023 by Robert Flint, MD
(Updated: 2/2/2026)
Click here to contact Robert Flint, MD
For the agitated geriatric patient, if verbal deescalation, distraction, and providing a safe quiet area do not work and you require chemical sedation use oral antipsychotics first. Follow this with IV or IM antipsychotics. Avoid benzodiazepines due to often worsening delirium or respiratory depression. For dosing, start low and go slow.
Emergency Medicine Clinics VOLUME 42, ISSUE 1, P135-149, FEBRUARY 2024
Michelle A. Fischer, MD, MPH Monica Corsetti, MD
Published:July 31, 2023DOI:https://doi.org/10.1016/j.emc.2023.06.016
Category: Trauma
Posted: 12/24/2023 by Robert Flint, MD
(Updated: 2/2/2026)
Click here to contact Robert Flint, MD
NEXUS criteria for blunt chest trauma patients who are over 14 years old, not intubated:
>60 years old
rapid deceleration defined as fall > 6 meters or motor vehicle crash >64 km/hour
chest pain
intoxication
abnormal alertness or mental status
distracting painful injury
tenderness to chest wall palpation
If abnormal chest X-Ray proceed to chest CT. Negative predictive value of 99.9% excluding major injury.
Category: Orthopedics
Posted: 12/23/2023 by Brian Corwell, MD
(Updated: 2/2/2026)
Click here to contact Brian Corwell, MD
Estimating the size of knee effusions
While this size range is typically easily detectable on exam. This may not apply to patients who are either very muscular or obese.
If the detection of a small to moderate sized effusion would change patient management
Consider ultrasound:
As compared to MRI (sensitivity of 81.3 % and a specificity of 100 %)
Draghi F, Urciuoli L, Alessandrino F, Corti R, Scudeller L, Grassi R. Joint effusion of the knee: potentialities and limitations of ultrasonography. J Ultrasound. 2015 Sep 18;18(4):361-71.
Category: EMS
Keywords: EMS, red, yellow, divert, capacity (PubMed Search)
Posted: 12/20/2023 by Jenny Guyther, MD
(Updated: 2/2/2026)
Click here to contact Jenny Guyther, MD
US hospitals have traditionally been concerned that without an ambulance diversion protocol that they would be overrun with EMS arrivals. EMS had been concerned that without diversion there would be extended wait times at the hospital. This study looked at EMS arrivals one year (2021) before the elimination of diversion and compared the number to one year after diversion elimination (2022).
This study of a single level 1 trauma center showed that there was NO difference between the number of EMS arrivals per day (84 vs 83, p = 0.08), time to room for ESI 2 patients, time to head CT in acute stroke patients OR ambulance turn around time (16 min vs 17 min, p = 0.15).
Aaron M. Burnett, Kari B. Haley, Matthew F. Milder, Bjorn K. Peterson, Joey Duren, Andrew Stevens, Danielle M. Hermes, Paul Nystrom, Joseph Lippert, Jennifer L. Moberg & Kurt M. Isenberger (2023) Elimination of Emergency Department Ambulance Divert during the COVID-19 Pandemic Was Not Associated with an Increase in the Average Number of Ambulance Arrivals per Day, Prehospital Emergency Care, DOI: 10.1080/10903127.2023.2271567
Category: Critical Care
Posted: 12/19/2023 by Mike Winters, MBA, MD
(Updated: 2/2/2026)
Click here to contact Mike Winters, MBA, MD
Acute-On-Chronic Liver Failure
Perricone G, et al. Intensive care management of acute-on-chronic liver failure. Critical Care. 2023;49:903-21.
Category: Ultrasound
Keywords: Obstetrics; POCUS; Transvaginal Ultrasound (PubMed Search)
Posted: 12/18/2023 by Alexis Salerno Rubeling, MD
Click here to contact Alexis Salerno Rubeling, MD
By performing a Point-of-Care Transvaginal Ultrasound (TVUS), we can decrease length of stay for patients with early pregnancy. Moreover, if an ectopic pregnancy is identified, we can decrease time to the OR for these patients.
Begin by discussing the exam with the patient and ensuring they have emptied their bladder. Apply a probe cover and add sterile lubricant to the outside of the probe tip. You can save time by performing a TVUS immediately after the pelvic speculum exam for swab collection.
Gently introduce the transducer with the marker upward, directed towards the ceiling. As you slowly advance, the uterus will be visualized in a sagittal orientation. Fan through the uterus by moving the probe handle left and right.
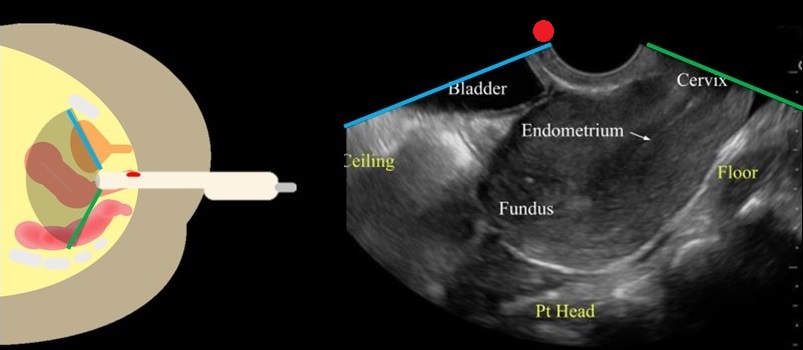
Image From: doi: 10.1016/j.emc.2022.12.006.
Rotate the transducer so that the marker is directed towards the patient's right side. Fan through the uterus by lifting the probe handle up and down.
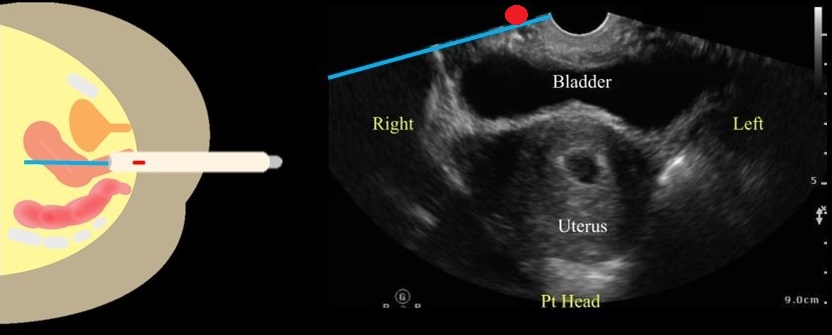
Image From: doi: 10.1016/j.emc.2022.12.006.
If a gestational sac is found, you should measure the gestational age and if present, fetal heart rate.
Tilt the transducer towards the patient's left or right side to visualize the adnexa. The adnexa will be located medially to the iliac vessels.
Remove the transducer and follow your department protocol for high level disinfection.
Salerno A, Lewiss RE. Rekindling the Relevance of Obstetrical Transvaginal POCUS: Overcoming Barriers to Ensure Patient-Centered Care. POCUS J. 2023 Nov 27;8(2):106-108. doi: 10.24908/pocus.v8i2.16855. PMID: 38099157; PMCID: PMC10721291.
King SA, Salerno A, Sommerkamp S. Ultrasound in Pregnancy. Emerg Med Clin North Am. 2023 May;41(2):337-353. doi: 10.1016/j.emc.2022.12.006. Epub 2023 Feb 9. PMID: 37024168.
Category: Trauma
Posted: 12/17/2023 by Robert Flint, MD
(Updated: 2/2/2026)
Click here to contact Robert Flint, MD
This commentary offers another reminder that there is significant bias in which trauma patients receive alcohol testing when that decision is made on a case by case basis. Age, sex, socioeconomic, race, injury pattern, all have been shown to influence provider ordering. Trauma systems should have pre-defined ordering criteria to eliminate this bias. The importance of gathering this testing information is to provide intervention and treatment to those in need. First we have to identify all patients in need.
Vanessa Cubas1, David N Naumann Addressing biases in alcohol testing for trauma patients: what is the solution? Emergency Medicine Journal. Volume 40 Issue 11. https://doi.org/10.1136/emermed-2023-213419
Category: Pediatrics
Keywords: fever, SBI, infants (PubMed Search)
Posted: 12/15/2023 by Jenny Guyther, MD
(Updated: 2/2/2026)
Click here to contact Jenny Guyther, MD
Urinary tract infection (UTI) is the leading cause of fever without a source in infants younger than 3 months. This data was collected from patients who presented to the emergency department with fever without a source over a 16 year period. Out of 2850 patients, 20.8% were diagnosed with a UTI, the majority of which grew E coli. Of those patients who were diagnosed with UTI, these patients were more likely to have a history of renal/GU problems, have a fever of at least 39C (38% vs 29%) or poor feeding (13% vs 8.7%). However, 48% had none of these risk factors. Also 6.1% of patients with a febrile UTI had another invasive bacterial infection. These patients were more likely to be < 1 month, be "irritable" per parents and have an elevated procalcitonin and CRP.
Bottom line: A lack of risk factors can not exclude a UTI in febrile infants < 3 months. A diagnosis of UTI also does not definitively exclude an additional invasive bacterial infection in a subset of these children.
Lejarzegi, Ainara MD*; Fernandez-Uria, Amaia MD*; Gomez, Borja MD, PhD*; Velasco, Roberto MD, PhD†; Benito, Javier MD, PhD*; Mintegi, Santiago MD, PhD*. Febrile Urinary Tract Infection in Infants Less Than 3 Months of Age. The Pediatric Infectious Disease Journal ():10.1097/INF.0000000000003947, April 24, 2023. | DOI: 10.1097/INF.0000000000003947
Category: Pharmacology & Therapeutics
Posted: 12/14/2023 by Ashley Martinelli
(Updated: 2/2/2026)
Click here to contact Ashley Martinelli
Bottom Line: Droperidol is an effective alternative to haloperidol in the treatment of gastroparesis although most patients will also receive prokinetic agents as well such as metoclopramide. It may also have some analgesic benefit.
Prior studies have demonstrated the efficacy and safety of haloperidol in the management of gastroparesis. A recent retrospective study was conducted to assess the impact of droperidol as it is an effective antiemetic similar to haloperidol.
This study enrolled 233 patients. Visits were matched with their most recent ED visit > 7 prior where droperidol was not administered.
Most patients were female, 51% African American, and the median age was 40. Doses ranged from 0.625 mg – 2.5 mg with the most common dose being 1.25 mg.
Results:
Stirrup N, Jones G, Arthus J, Lewis Z. Droperidol undermining gastroparesis symptoms (DRUGS) in the emergency department. American Journal of Emergency Medicine. 2024;75:42-45.
Category: Critical Care
Keywords: Critical Care, Burn, Resuscitation (PubMed Search)
Posted: 12/13/2023 by Lucas Sjeklocha, MD
Click here to contact Lucas Sjeklocha, MD
Bottom line: In the 2023 updated Clinical Practice Guideline, the American Burn Association recommends 2ml/kg/%TBSA (for burns >20% TBSA)as initial starting point for fluid administration in the first 48 hours, guided by clinical factors with consideration of supplemental albumin to limit fluid administration. Fresh frozen plasma should be considered in the context of a clinical trial. Vitamin C and advanced hemodynamic monitoring are not recommended as they have not demonstrated improved outcomes.
Summary: Burn care has a paucity of high-quality research about some of the fundamental questions for resuscitation. The American Burn Association since 2010 has endorsed fluid volumes for patients with >20% TBSA (i.e. those predicted to develop burn shock) from 2ml/kg/%TBSA to 4ml/kg/%TBSA as a starting point for fluid resuscitation. Further clinical studies since then have demonstrated that lower volumes of fluid targeting urine output and other physiological variables are effective without demonstrating clear improvement in patient centered outcomes. Further adjuncts such as albumin or fresh frozen plasma have demonstrated reduced fluid administration but no improvement in patient-centered outcomes. While “fluid creep” is increasingly recognized, demonstrating benefits in clinical trials will likely remain elusive as overall practice continues to shift towards less fluids and the adjunctive use of colloid will likely continue to expand. In addition to ABA CPGs and resources, the Joint Trauma System also has several useful resources for burn care.
Sources:
https://doi.org/10.1093/jbcr/irad125
https://jts.health.mil/assets/docs/cpgs/Burn_Care_11_May_2016_ID12.pdf
Category: Trauma
Keywords: soft tissue injury, trauma, (PubMed Search)
Posted: 12/10/2023 by Robert Flint, MD
(Updated: 2/2/2026)
Click here to contact Robert Flint, MD
Here are three good resources to learn about a soft tissue injury seen in high velocity blunt trauma patients called Morel-Lavallee lessions.
“Morel Lavallee lesions are soft tissue injuries seen in high-velocity trauma and are usually associated with underlying fractures of the pelvis, acetabulum, or proximal femur. Often these injuries are not immediately diagnosed due to the distracting concomitant bony injuries. However, identification of such injuries is important as they may pose as an independent risk factor for surgical site infection. The clinical findings include soft tissue swelling, bruise/ ecchymosis, fluctuance, and compressibility in the swelling. The diagnosis is usually established on physical examination, however, radiological investigations including ultrasonography and CT might help. The management options include nonoperative treatment, percutaneous aspiration, and open debridement.” 1
“Morel-Lavallée lesions are often the result of skin and subcutaneous tissue quickly tearing away from the underlying fascia. This allows a range of fluids to fill the space in the form of hemolymphatic masses. The two most common sites are the prepatellar plate of the knee and the lateral fascia of the hip.” 2
“ML lesion is often undiagnosed during initial presentation of a trauma patient, and emergency physicians and trauma surgeons should be aware of the possibility of occurrence of this injury. MRI is the imaging modality of choice, and the presence or absence of a capsule is an important imaging finding that guides appropriate therapy. Early diagnosis and management will help prevent long-term morbidity and complications in these patients.”3
Category: EMS
Keywords: EMS, trauma, emergency medical services, (PubMed Search)
Posted: 12/6/2023 by Ben Lawner, MS, DO
(Updated: 2/2/2026)
Click here to contact Ben Lawner, MS, DO
BACKGROUND
EMS systems differ in staffing and composition. The Japanese model utilizes “doctor cars” which bring a physician and nurse to the scene of a critical patient encounter. Personnel on the “doctor cars” are able to perform advanced therapies such as REBOA, finger thoracostomy, and chest tube thoracostomy. As physician EMS fellowships continue to expand in the United States, it is helpful to examine the utility of physician response incorporated into prehospital emergency care.
THE STUDY
A nationwide retrospective cohort study including over 370,000 patients examined the impact of Japan “doctor cars” upon in hospital survival. Doctor cars responded to 2361 trauma patients, and traditional Ground Emergency Medical Services (GEMS) units cared for 46,783 trauma patients. The study’s primary outcome was survival to discharge.
The adjusted odds ratio for survival was significantly higher in the exposure group served by the doctor cars. The study suggests that there may be a role for augmenting ground EMS personnel in the response to critical injuries. Via logistic regression, the study controlled for multiple other variables such as age, sex, prehospital vital signs, out of hospital time, and injury severity score (ISS).
BOTTOM LINE
This study is far from definitive but contributes to a growing body of literature addressing how EMS physicians integrate into prehospital systems.
Hayashi T, Matsuo K, Furuya S, Nakajima Y, Hitomi S, Ogawa K, Suzuki H, Yamamoto D, Asami M, Sakamoto S, Kamiyama J, Okuda Y, Minami K, Teshigahara K, Gokita M, Yasaka K, Taguchi S, Kiyota K. Impact of physician-staffed ground emergency medical services-administered pre-hospital trauma care on in-hospital survival outcomes in Japan. Eur J Trauma Emerg Surg. 2023 Nov 24. doi: 10.1007/s00068-023-02383-w. Epub ahead of print. PMID: 37999771.
Category: Critical Care
Keywords: vasopressor, norepinephrine, timing, septic shock (PubMed Search)
Posted: 12/5/2023 by Quincy Tran, MD, PhD
(Updated: 2/2/2026)
Click here to contact Quincy Tran, MD, PhD
Settings: systemic review and meta-analysis
Participants: 2 RCTs, 21 observational studies. Fifteen studies were published between 2020-2023.
There was a total of 25721 patients with septic shock
Outcome measurement: Primary outcome was short-term mortality (ICU, hospital, 28-day, 30-day). Secondary outcomes included ICU LOS, Hospital LOS, time to achieve MAP > 65 mm Hg,
Study Results:
Composite outcome of short term mortality:
Secondary outcome:
Discussion:
Conclusion:
More and more studies, although a RCT is still necessary, are showing that early initiation of vasopressor within 1-6 hours of septic shock would be more beneficial to patients with septic shock.
Ye E, Ye H, Wang S, Fang X. INITIATION TIMING OF VASOPRESSOR IN PATIENTS WITH SEPTIC SHOCK: A SYSTEMATIC REVIEW AND META-ANALYSIS. Shock. 2023 Nov 1;60(5):627-636. doi: 10.1097/SHK.0000000000002214. Epub 2023 Sep 2. PMID: 37695641.
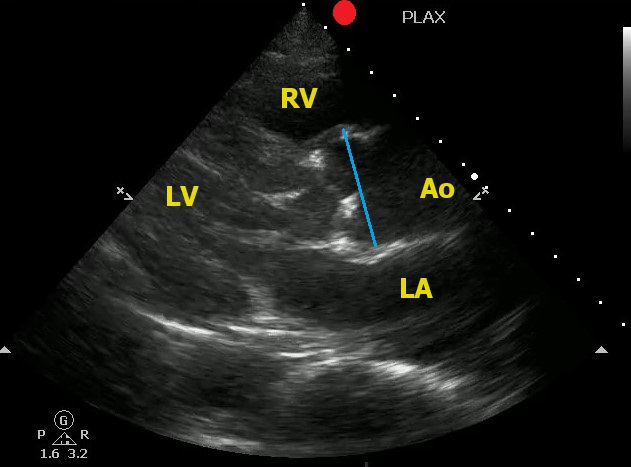
Category: Vascular
Keywords: aortic aneurysm; point-of-care ultrasound; pocus; aortic dissection (PubMed Search)
Posted: 12/4/2023 by Alexis Salerno Rubeling, MD
(Updated: 2/2/2026)
Click here to contact Alexis Salerno Rubeling, MD
Point-of-Care Ultrasound can help to identify signs of thoracic aortic dissection.
One view to help in your assessment is the Parasternal Long Axis View.
To correctly measure the aortic root:
Here is an example of an aortic root aneurysm:
Kennedy Hall M, Coffey EC, Herbst M, Liu R, Pare JR, Andrew Taylor R, Thomas S, Moore CL. The "5Es" of emergency physician-performed focused cardiac ultrasound: a protocol for rapid identification of effusion, ejection, equality, exit, and entrance. Acad Emerg Med. 2015 May;22(5):583-93. doi: 10.1111/acem.12652.
Category: Trauma
Keywords: prehospital, EDTCO2, mortality (PubMed Search)
Posted: 12/3/2023 by Robert Flint, MD
Click here to contact Robert Flint, MD
A retrospective study of 2 years of data from 24 trauma centers looking at end tidal CO2 as a predictor of mortality in trauma patients found:
"A total of 1,324 patients were enrolled. ETCO2 was better in predicting mortality than shock index (SI) and systolic blood pressure (SBP). Prehospital lowest ETCO2 , SBP , and SI were all predictive of Mass Transfusion."
Another data point to consider when setting up trauma triage protocols and looking for patients who will require intensive interventions early.
Campion EM, Cralley A, Sauaia A, Buchheit RC, Brown AT, Spalding MC, LaRiccia A, Moore S, Tann K, Leskovan J, Camazine M, Barnes SL, Otaibi B, Hazelton JP, Jacobson LE, Williams J, Castillo R, Stewart NJ, Elterman JB, Zier L, Goodman M, Elson N, Miner J, Hardman C, Kapoen C, Mendoza AE, Schellenberg M, Benjamin E, Wakam GK, Alam HB, Kornblith LZ, Callcut RA, Coleman LE, Shatz DV, Burruss S, Linn AC, Perea L, Morgan M, Schroeppel TJ, Stillman Z, Carrick MM, Gomez MF, Berne JD, McIntyre RC, Urban S, Nahmias J, Tay E, Cohen M, Moore EE, McVaney K, Burlew CC. Prehospital end-tidal carbon dioxide is predictive of death and massive transfusion in injured patients: An Eastern Association for Surgery of Trauma multicenter trial. J Trauma Acute Care Surg. 2022 Feb 1;92(2):355-361. doi: 10.1097/TA.0000000000003447. PMID: 34686640.
Category: Quality Assurance/Quality Improvement
Keywords: Checklists, Patient Safety, Quality (PubMed Search)
Posted: 12/2/2023 by Brent King, MD
Click here to contact Brent King, MD
The Bottom Line: Investigators studying the use of a pre-intubation checklist versus "usual care" found no differences in important outcomes such as oxygen saturation and first pass success. However, the study was conducted as a part of a larger study, was unblinded, and not well controlled.
The investigators who conducted the multicenter CHECK UP trial, a study of head up intubation in ICU patients, reviewed the care of 262 ICU patients who were intubated. Some intubation attempts were guided by a pre-intubation checklist and some were not. The authors found no difference between the groups in lowest SPO2, number of intubation attempts, etc. However, the study was unblinded and largely observational. In many cases, the elements of a checklist had been incorporated into routine practice.
Take Home Point: While the authors found no differences in outcomes, this study does little to prove or disprove the value of pre-intubation checklists. Not only was the study essentially uncontrolled, the untoward events being studied are unusual in the hands of experienced clinicians.
Comment: Pre-procedural checklists make intuitive sense to me. They help us to avoid cultural drift. I am certainly not ready to abandon the use of a pre-intubation checklist based upon this study
Janz DR, Semler MW, Joffe AM, et al. A multicenter, randomized trial of a checklist for endotracheal intubation of critically ill adults. Chest 2018;153:816-824.
Category: Pediatrics
Posted: 12/1/2023 by To-Lam Nguyen, MD
Click here to contact To-Lam Nguyen, MD
Since Christmas is coming up, let's talk about Hemophilia A (factor VIII deficiency) and Hemophilia B (factor IX deficiency, also known as Christmas disease)
Deficiencies in Factors VIII and IX are the most common severe inherited bleeding disorders.
Pathophysiology:
Clinical Manifestations:
Lab findings and diagnosis
Genetics
Classification
trauma to induce bleeding
Treatment
Summary:
Kliegman R, Stanton B, St. Geme JW, Schor NF, Behrman RE. Nelson Textbook of Pediatrics. Edition 20. Elsevier; 2016. Accessed December 1, 2023. https://search.ebscohost.com/login.aspx?direct=true&db=cat01362a&AN=hshs.004567758&site=eds-live
