Category: Toxicology
Keywords: acetaminophen overdose, fomepizole, NAC (PubMed Search)
Posted: 7/19/2023 by Natasha Tobarran, DO
(Updated: 2/2/2026)
Click here to contact Natasha Tobarran, DO
Acetaminophen (APAP) is the leading cause of acute liver failure worldwide. Standard treatment for APAP overdose is with N-acetylcysteine (NAC), which is highly effective if given within 8 hours of ingestion. However, in delayed presenters or massive ingestions patients can still develop hepatotoxicity. Adjunctive therapies can be considered in these cases including augmented NAC dosing, renal replacement, and fomepizole.
A small amount of APAP is metabolized to N-acetyl-p-benzoquinone imine (NAPQI) by cytochrome 2E1. In therapeutic doses, the body is able to detoxify the NAPQI using glutathione. In overdose, glutathione stores get depleted and NAPQI can cause hepatotoxicity. Mitochondrial damage in APAP overdose is mediated by the c-Jun-N-terminal Kinase (JNK) pathway.
NAC works to replenish glutathione stores and detoxify NAPQI. In large overdoses, increased dosing of NAC may be necessary. Fomepizole is typically used for its alcohol dehydrogenase inhibitor property to treat methanol and ethylene glycol poisoning. Fomepizole is also a cytochrome 2E1 and JNK inhibitor and can be used in APAP overdose to block the formation of NAPQI and mitigate mitochondrial damage. Dialysis can be used to eliminate APAP from the body completely in massive overdoses or if significant acidosis or renal failure.
This study is a case series of 14 patients treated for APAP overdose between 2017 – 2021 at a tertiary hospital
Limitations of the study:
In summary:
Stephanie L. Link, Garrett Rampon, Stephen Osmon, Anthony J. Scalzo & Barry H. Rumack (2022) Fomepizole as an adjunct in acetylcysteine treated acetaminophen overdose patients: a case series, Clinical Toxicology, 60:4, 472-477, DOI: 10.1080/15563650.2021.1996591
Category: EMS
Keywords: handoff, communication, adverse outcomes (PubMed Search)
Posted: 7/19/2023 by Jenny Guyther, MD
Click here to contact Jenny Guyther, MD
Sumner BD, Grimsley EA, Cochrane NH, et al. Videographic Assessment of the Quality of EMS to ED Handoff Communication During Pediatric Resuscitations. Prehosp Emerg Care. 2019;23(1):15-21. doi:10.1080/10903127.2018.
Category: Critical Care
Keywords: Central Lines, Platelets, Bleeding (PubMed Search)
Posted: 7/18/2023 by Mark Sutherland, MD
(Updated: 2/2/2026)
Click here to contact Mark Sutherland, MD
Central Venous Catheter (CVC; aka central line) placement is a common procedure in both the ED and ICU, and while overall quite safe, does carry some risk. In particular, many of us regularly are confronted with the challenge of placing a line in a patient with profound thrombocytopenia, which can result in significant bleeding. In these cases, should we give platelets before we place the line?
Van Baarle et al published a randomized study in NEJM comparing an empiric 1u platelet transfusion vs no transfusion in patients with a platelet count of 10,000-50,000, prior to line placement. The study included both HD and non-HD (e.g. TLC) lines, from all three major access sites, in patients in their ICU or hematology ward. They found statistically fewer serious bleeding events in the transfusion group (4.8%) vs no transfusion group (11.9%). The study wasn't powered to look at more patient oriented outcomes like mortality, but I'm sure we can all agree less bleeding is probably a good thing. Also importantly, this study did not evaluate the risks/benefits of delaying line placement to obtain platelets when the line is urgently needed, so I would not recommend extending this to conclude platelets must be given before line placement if the line is needed for something highly time-sensitive (e.g. only available access to infuse pressors in a hypotensive patient).
Bottom Line: It is probably beneficial and appropriate to provide prophylactic platelet transfusion prior to CVC placement in patients with a platelet count less than 50,000, assuming circumstances allow.
van Baarle FLF, van de Weerdt EK, van der Velden WJFM, Ruiterkamp RA, Tuinman PR, Ypma PF, van den Bergh WM, Demandt AMP, Kerver ED, Jansen AJG, Westerweel PE, Arbous SM, Determann RM, van Mook WNKA, Koeman M, Mäkelburg ABU, van Lienden KP, Binnekade JM, Biemond BJ, Vlaar APJ. Platelet Transfusion before CVC Placement in Patients with Thrombocytopenia. N Engl J Med. 2023 May 25;388(21):1956-1965. doi: 10.1056/NEJMoa2214322. PMID: 37224197.
https://www.nejm.org/doi/10.1056/NEJMoa2214322
Category: Trauma
Keywords: access, IO, IV, resucitation (PubMed Search)
Posted: 7/9/2023 by Robert Flint, MD
Click here to contact Robert Flint, MD
This study found that time to intraosseous was faster than time to peripheral IV. This lead to quicker resuscitation time. This was particularly true in pateints that arrived without a pre-hospital IV.
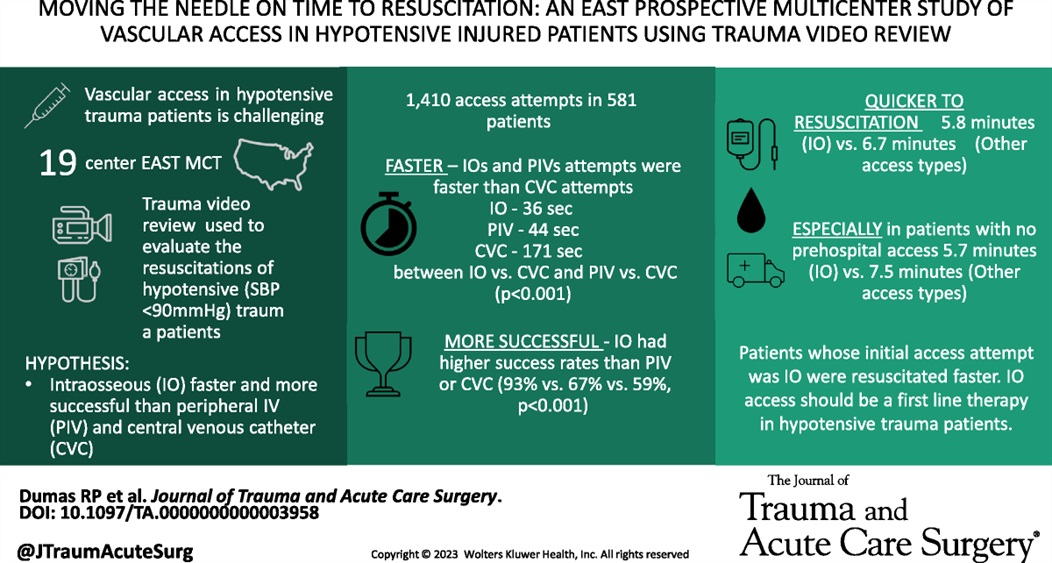
Dumas, Ryan P. MD; Vella, Michael A. MD; Maiga, Amelia W. MD; Erickson, Caroline R. MD; Dennis, Brad M. MD; da Luz, Luis T. MD, MSc; Pannell, Dylan MD; Quigley, Emily BSN; Velopulos, Catherine G. MD; Hendzlik, Peter; Marinica, Alexander DO; Bruce, Nolan MD; Margolick, Joseph MD; Butler, Dale F. MD; Estroff, Jordan MD; Zebley, James A. MD; Alexander, Ashley MD; Mitchell, Sarah MD; Grossman Verner, Heather M. MS; Truitt, Michael MD; Berry, Stepheny MD; Middlekauff, Jennifer BSN; Luce, Siobhan MD; Leshikar, David MD; Krowsoski, Leandra MD; Bukur, Marko MD; Polite, Nathan M. DO; McMann, Ashley H. MD; Staszak, Ryan MD; Armen, Scott B. MD; Horrigan, Tiffany MD; Moore, Forrest O. MD; Bjordahl, Paul MD; Guido, Jenny MD; Mathew, Sarah MD; Diaz, Bernardo F. MD; Mooney, Jennifer MD; Hebeler, Katherine MD; Holena, Daniel N. MD. Moving the needle on time to resuscitation: An EAST prospective multicenter study of vascular access in hypotensive injured patients using trauma video review. Journal of Trauma and Acute Care Surgery 95(1):p 87-93, July 2023. | DOI: 10.1097/TA.0000000000003958
Category: Pediatrics
Keywords: Pediatrics, infectious disease, fever, bacteremia (PubMed Search)
Posted: 7/14/2023 by Kathleen Stephanos, MD
(Updated: 2/2/2026)
Click here to contact Kathleen Stephanos, MD
This study attempts to answer the age old question: What is the importance of fever in pediatric illnesses?
The authors' goal was to assess if response to antipyretics was associated with bacteremia. This article retrospectively reviewed 6,319 febrile children in whom blood cultures were sent and found that 3.8% had bacteremia. They then looked at the fever curve in response to antipyretics for these two groups in the emergency department over 4 hours. The study concluded that patients with bacteremia have a higher rate of persistent fever despite antipyretics. It is important to note the limitations of this study. As this was retrospective, it is unclear what clinical findings resulted in blood cultures being sent - most febrile children did not have any drawn (23,999 were excluded for this reason). They did not assess other vital signs, and did not address other bacterial infections (UTI, cellulitis, meningitis, otitis media, etc). Additionally, while patients with bacteremia did have a higher likelihood of fever, the majority of patients in both groups had fever resolution within 4 hours, and both groups had some children with persistent fevers.
Overall, this does seem to support the decision to consider obtaining further testing in those children with a persistent fever, but also emphasizes the importance of not using fever resolution alone as support for discharge to home or exclusion of bacteremia from the differential.
Baker AH, Monuteaux MC, Michelson KA, Neuman MI. Resolution of Fever in the Pediatric Emergency Department and Bacteremia. Clin Pediatr (Phila). 2023;62(5):474-480.
Category: Pharmacology & Therapeutics
Keywords: Calcium, Massive transfusion protocol, Citrate, Blood products (PubMed Search)
Posted: 7/13/2023 by Wesley Oliver
(Updated: 2/2/2026)
Click here to contact Wesley Oliver
Citrate is an anticoagulant added to blood products to maintain stability for storage. With the administration of large volumes of blood products, citrate binds to ionized calcium, which can cause hypocalcemia. Evidence for specific calcium administration during massive transfusion protocols is limited; however, a proposed strategy has been to administer calcium gluconate 2 grams for every 2-4 units of red blood cells.
Robinson, et al. performed a retrospective analysis attempting to determine the optimal Citrate:Ca ratio (a novel ratio created for this study) to reduce 30-day mortality. They did not find any differences in mortality; however, they found a Citrate:Ca ratio of 2-3 produced a normalized ionized calcium level with 24 hours of a massive transfusion protocol.
Based on their calculations, this would equate to supplementing 1 g of calcium gluconate for every 3 units of red blood cells given.
***Reminder: Based on the amount of elemental calcium in each gram of calcium gluconate (4.7 mEq) and calcium chloride (13.6 mEq); 3 g calcium gluconate=1 g calcium chloride.***
Bottom Line: Supplementing with calcium gluconate 1 g for every 3 units of red blood cells should be sufficient to maintain normal ionized calcium levels after a massive transfusion protocol.
Robinson A, Rech MA, DeChristopher PJ, Vaughn A, Rubino J, Bannister E, Moore ME, Chang K. Defining the optimal calcium repletion dosing in patients requiring activation of massive transfusion protocol. Am J Emerg Med. 2023 May 13;70:96-100.
Category: Toxicology
Keywords: CO (PubMed Search)
Posted: 7/13/2023 by Mak Moayedi, MD
(Updated: 2/2/2026)
Click here to contact Mak Moayedi, MD
Age >36
LOC
Prolonged exposure (>24hrs)
COHgb level >25%
Weaver LK, Valentine KJ, Hopkins RO. Carbon monoxide poisoning: risk factors for cognitive sequelae and the role of hyperbaric oxygen. American journal of respiratory and critical care medicine. 2007;176(5):491-497. doi:10.1164/rccm.200701-026OC
Category: Trauma
Keywords: pelvic fracture, binder, hemorrhage (PubMed Search)
Posted: 7/9/2023 by Robert Flint, MD
Click here to contact Robert Flint, MD
Pelvic fractures can be a major source of life threatening hemorrhage. Suspect fracture with significant force/mechanism. Signs are pelvic tenderness (no need to “rock” the pelvis), bruising at perineum, and hypotension in the setting of major trauma. Major classifications of pelvic fractures are lateral compression, anterior posterior (wide public ramus, open book), and vertical sheer (fall from height). An appropriately applied pelvic binding device can be lifesaving. The biggest mistake in applying these devices is to apply them too high. Maximum pressure is achieved with application directly across the greater trochanters.
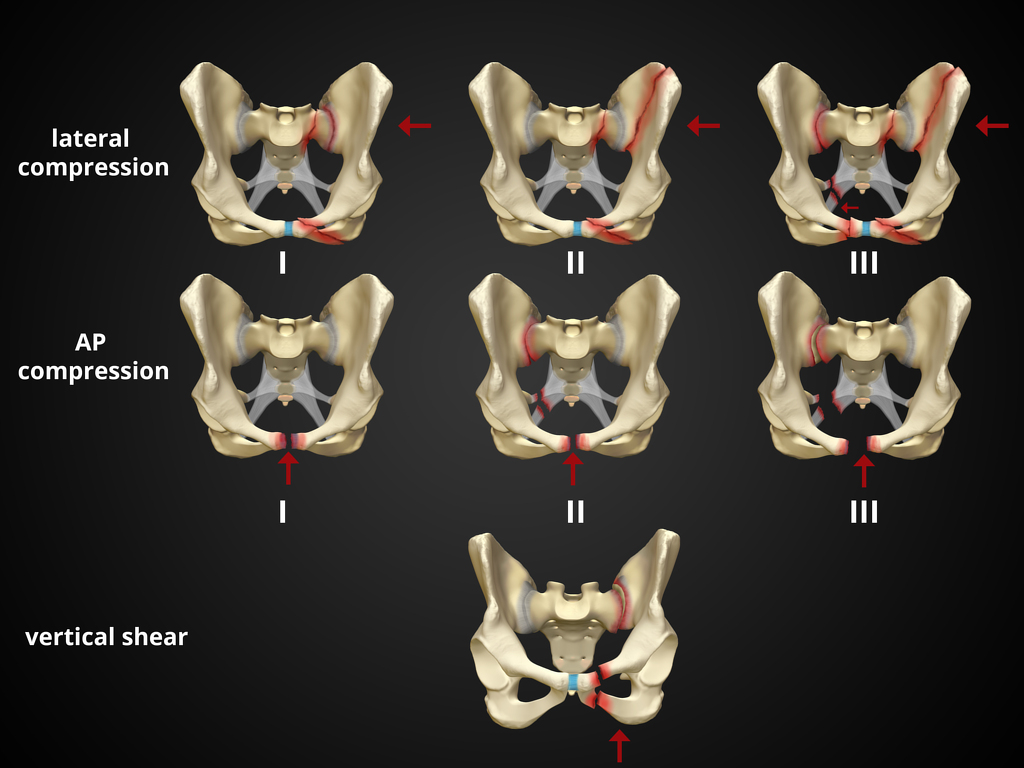
1. https://radiopaedia.org/cases/pelvic-fracture-diagrams
2. Bonner TJ, Eardley WGP, Newell N, et al. Accurate placement of a pelvic binder improves reduction of unstable fractures of the pelvic ring. J Bone Joint Surg Br. 2011;93-B(11):1524-1528. doi:10.1302/0301-620X.93B11.27023
Category: Orthopedics
Keywords: blurry vision, head trauma (PubMed Search)
Posted: 7/8/2023 by Brian Corwell, MD
Click here to contact Brian Corwell, MD
Multiple vision disorders may occur after concussion including injury to the systems that control binocular vision including: Convergence insufficiency and Accommodation insufficiency
In order to obtain a single binocular vision, simultaneous movement of both eyes in opposite directions is required.
To look at an object close by such as when reading, the eyes must rotate towards each other (convergence).
Convergence insufficiency is the reduced ability to converge enough for near vision and is a common visual dysfunction seen after concussion.
One of both eyes may also turn outward.
May lead to complaints with reading such as diplopia, blurry vision, eyestrain, and skipping words or losing one's place.
Patient or parent may also report other difficulties such as becoming more easily fatigued when reading, needing to squint and/or having disinterest in reading.
Take home: consider testing convergence in patients with some of these complaints in setting of acute or subacute head trauma.
Master CL, Bacal D, Grady MF, Hertle R, Shah AS, Strominger M, Whitecross S, Bradford GE, Lum F, Donahue SP; AAP SECTION ON OPHTHALMOLOGY; AMERICAN ACADEMY OF OPHTHALMOLOGY; AMERICAN ASSOCIATION FOR PEDIATRIC OPHTHALMOLOGY AND STRABISMUS; and AMERICAN ASSOCIATION OF CERTIFIED ORTHOPTISTS. Vision and Concussion: Symptoms, Signs, Evaluation, and Treatment. Pediatrics. 2022 Aug 1;150(2):e2021056047.
Category: Pediatrics
Keywords: burns, pediatric (PubMed Search)
Posted: 7/7/2023 by Jenny Guyther, MD
(Updated: 2/2/2026)
Click here to contact Jenny Guyther, MD
Kliegman, R. M., MD, Stanton, B. F., MD, St Geme, J., MD, & Schor, N. F., MD PhD. (2015). Nelson Textbook of Pediatrics (20th ed.). Elsevier Health Sciences.
Category: Toxicology
Keywords: cannabis exposure, pediatric, toxicity, NPDS (PubMed Search)
Posted: 7/6/2023 by Hong Kim, MD
(Updated: 2/2/2026)
Click here to contact Hong Kim, MD
Medical Cannabis is permitted in 39 states and Washington DC while 18 sates and Washington DC has legalized recreational cannabis use. As cannabis products become more available, pediatric exposure has also increased.
A retrospective study of National Poison Data System involving children < 6 years from 2017 and 2021 showed: Pre-COVID (2017-2019) & COVID (2020-2021)
Common Clinical effects
Disposition
Conclusion
Tweet MS, Nemanich A, Wahl M. Pediatric Edible Cannabis Exposures and Acute Toxicity: 2017–2021. Pediatrics. 2023;151(2):e2022057761
Category: Gastrointestional
Keywords: POCUS, Appendicitis, Pregnancy (PubMed Search)
Posted: 7/3/2023 by Alexis Salerno Rubeling, MD
Click here to contact Alexis Salerno Rubeling, MD
POCUS can be used to screen for appendicitis.
A recent study showed a sensitivity of 66.7% (CI 95% 47.1–82.7), and a specificity of 96.8% (CI 95% 83.3–99.9) during pregnancy, with the highest sensitivity in the first trimester.
2 methods to locate the appendix are:
1) have your patient point to the area where it hurts the most
2) perform a lawnmower technique over the right lower quadrant looking for the right psoas mucle and the iliac vessels. The appendix will usually be near these structures.
Sometimes it is easiest to use your curvilinear probe to identify an area of inflammation and then change to the linear probe for better visualization.
On ultrasound, appendicitis is defined as a non-compressible blind pouch with an outer diameter greater than 6 mm. On short axis the inflammed appendix will look like a target sign:
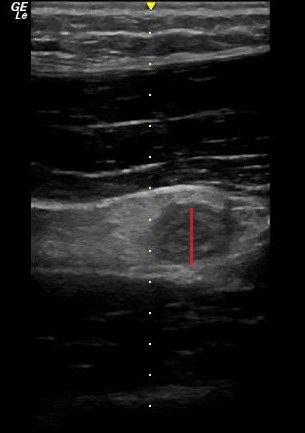
Abgottspon D, Putora K, Kinkel J, Süveg K, Widmann B, Hornung R, Minotti B. Accuracy of Point-of-care Ultrasound in Diagnosing Acute Appendicitis During Pregnancy. West J Emerg Med. 2022 Oct 23;23(6):913-918. doi: 10.5811/westjem.2022.8.56638
Category: Trauma
Keywords: shock index, trauma, pre-hospital (PubMed Search)
Posted: 7/2/2023 by Robert Flint, MD
(Updated: 2/2/2026)
Click here to contact Robert Flint, MD
Shock index (heart rate/systolic blood pressure) has been used to predict trauma outcomes. This study from American Journal of Emergency Medicine looked at 89,000 pre-hospital patients who had a normal shock index on arrival at an emergency department. They then looked for those with abnormal pre-hospital shock index vs. those without an abnormal shock index and compared outcomes. Those with an abnormal pre-hospital shock index had worse outcomes than those with normal pre-hospital shock index.
Bottom line: A good handoff from pre-hospital to emergency department staff is critical because any abnormal shock index predicts a worse outcome than those with a normal shock index.
Yoshie Yamada Sayaka Shimizu, et al Prehospital shock index predicts 24-h mortality in trauma patients with a normal shock index upon emergency department arrival Am J Emerg Med 2023 May 10;70:101-108 doi: 10.1016/j.ajem.2023.05.008.
Category: Ophthamology
Keywords: Optho. (PubMed Search)
Posted: 6/16/2023 by Robert Flint, MD
(Updated: 6/29/2023)
Click here to contact Robert Flint, MD
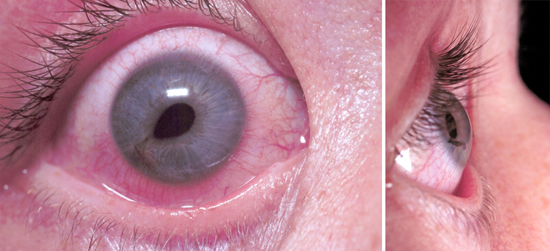
What is this called? What does it indicate? Treatment?
Tear Drop pupil. Globe rupture/corneal laceration. Protect the eye with a commercially available shield (Fox, etc) or if none is available use a paper/sytroform cup that can be cut to length to allow taping in place. Start IV antibiotics and emergency opthamology referal.
1. https://www.jems.com/patient-care/traumatic-eye-injury-management-principl-0/
2. https://eyesoneyecare.com/resources/ophthalmic-emergencies-open-globe-injuries/
Category: Administration
Keywords: predictive rule, EHR, utilization, AI (PubMed Search)
Posted: 6/16/2023 by Robert Flint, MD
(Updated: 2/2/2026)
Click here to contact Robert Flint, MD
Author- Steve Schenkel, MD MPP Professor of Emergency Mediciner at UMEM:
A recent Annals of Emergency Medicine Publication (here https://www.annemergmed.com/article/S0196-0644(22)01276-8/fulltext) tested a predictive rule for Likelihood to Occupy an Inpatient Bed associated with a common Electronic Health Record.
At the individual patient level, the score performed ok. Depending on the chosen threshold, it traded off sensitivity and specificity and generally became more accurate the longer the patient was in the ED.
The authors and the associated editorial (here https://www.annemergmed.com/article/S0196-0644(22)01401-9/fulltext) suggest a different, potentially more beneficial use: to allow aggregate prediction of admissions across an entire department and therefore prompt earlier planning to prevent crowding on account of boarding.
The takeaway: Administrative prediction rules oriented toward individual patients may be more meaningfully used to predict resource needs, including in-patient beds, across the ED population.
Category: Critical Care
Keywords: NEWS, MEWS, IEWS, international Early Warning Score, mortality (PubMed Search)
Posted: 6/27/2023 by Quincy Tran, MD, PhD
(Updated: 2/2/2026)
Click here to contact Quincy Tran, MD, PhD
Settings: Retrospective data from 3 Dutch EDs (development of the score), 2 Denmark ED (for validation of the score). The novel score (International Early Warning Score) will be composed of the National Early Warning Score (NEWS) + Age +Sex
Components of the National Early Warning Score:
Participants: All adult patients in the Netherlands Emergency department Evaluation Database (NEED) and Danish Multicenter Cohort (DMC).
Outcome measurement: in-hospital mortality, including death in EDs.
Study Results:
Discussion:
Conclusion:
This multicenter study showed that IEWS perform better than the NEWS for predicting in-hospital mortality for ED patients.
Candel BGJ, Nissen SK, Nickel CH, Raven W, Thijssen W, Gaakeer MI, Lassen AT, Brabrand M, Steyerberg EW, de Jonge E, de Groot B. Development and External Validation of the International Early Warning Score for Improved Age- and Sex-Adjusted In-Hospital Mortality Prediction in the Emergency Department. Crit Care Med. 2023 Jul 1;51(7):881-891. doi: 10.1097/CCM.0000000000005842. Epub 2023 Mar 23. PMID: 36951452; PMCID: PMC10262984.
Category: Orthopedics
Keywords: POCUS, Hip Fractures, Nerve Blocks, Administration (PubMed Search)
Posted: 6/26/2023 by Alexis Salerno Rubeling, MD
(Updated: 2/2/2026)
Click here to contact Alexis Salerno Rubeling, MD
The use of a fascia iliaca compartment block has been shown to reduce pain, decrease length of stay and decrease the opiate requirements for patients with hip fractures.
Check out this page on how to perform this procedure.
Fascia iliac blocks can be challenging to implement routinely in the emergency department. Studies show that 2.5% of eligible patients, despite departmental implementation, receive a block.
One recently published article showed that large scale multi-disciplinary implementation can increase the use of fascia iliac blocks. After implementation, the study team found that 54% of eligible patients received a fascia iliac block.
This article is interesting as it provides helpful resources including physician and nursing protocols for performing this block.
Downs T, Jacquet J, Disch J, Kolodychuk N, Talmage L, Krizo J, Simon EL, Meehan A, Stenberg R. Large-scale Implementation of Fascia Iliaca Compartment Blocks in an Emergency Department. West J Emerg Med. 2023 May 3;24(3):384-389. doi: 10.5811/westjem.58793. PMID: 37278790; PMCID: PMC10284502.
Category: Trauma
Keywords: lidocaine, trauma, rib fractures (PubMed Search)
Posted: 6/25/2023 by Robert Flint, MD
(Updated: 2/2/2026)
Click here to contact Robert Flint, MD
Use of intravenous lidocaine has been proposed as an adjunct/replacement for opioids in trauma patients with rib fractures. These small studies show a signal that the use of lidocaine decreased the need for opiate pain medication in this cohort of patients. Larger studies are needed, however, trauma surgeons maybe reaching for intravenous lidocaine in patients they are admitting with rib fractures. Also, transdermal lidocaine patches have been shown to have a similar effect in this patient cohort. “In admitted trauma patients with acute rib fractures not requiring continuous intravenous opiates, lidocaine patch use was associated with a significant decrease in opiate utilization during the patients’ hospital course.” 3
1. Patton, Petrease MD, MSc; Vogt, Kelly MD, MSc; Priestap, Fran MSc; Parry, Neil MD; Ball, Ian M. MD, MSc. Intravenous lidocaine for the management of traumatic rib fractures: A double-blind randomized controlled trial (INITIATE program of research). Journal of Trauma and Acute Care Surgery 93(4):p 496-502, October 2022. | DOI: 10.1097/TA.0000000000003562
2. Jeff Choi , Kirellos Zamary, Nicolas B. Barreto, Lakshika Tennakoon, Kristen M. Davis, Amber W. Trickey, David A. Spain. Intravenous lidocaine as a non-opioid adjunct analgesic for traumatic rib fractures. Published: September 28, 2020 https://doi.org/10.1371/journal.pone.0239896
3. Johnson M, Strait L, Ata A, et al. Do Lidocaine Patches Reduce Opioid Use in Acute Rib Fractures? The American SurgeonTM. 2020;86(9):1153-1158. doi:10.1177/0003134820945224
Category: Administration
Keywords: concussion recovery (PubMed Search)
Posted: 6/24/2023 by Brian Corwell, MD
(Updated: 2/2/2026)
Click here to contact Brian Corwell, MD
How much screen time after concussion?
Adolescents spent more than 7 hours daily on screen time during the pandemic.
Historically, experts recommended screen time abstinence to various degrees after concussion.
Prior study: RCT of concussion patients (ages 12 to 25) found that those who abstain from screen time for the first 48 hours recovered 4.5 days sooner than those who were permitted screen time.
Population: 633 children and adolescents with acute concussion and 334 with orthopedic injuries aged 8 to 16, recruited from 5 Canadian pediatric emergency departments.
Post concussion symptoms were measured at 7 to 10 days, weekly for three months, and biweekly for three to six months post injury. Screen time was measured.
Results: Screen time was a significant predictor of post concussion symptom recovery with both parent reported somatic and self-reported cognitive symptoms.
There may be an effect of low to moderate screen time (Goldilocks effect) demonstrating that those in the 25th to 50th percentiles had less severe symptoms than those on the higher end of screen time use or those who minimally use of screens!
Low and high screen time were both associated with relatively more severe symptoms in the concussion group compared to the orthopedic injury group during the first 30 days post recovery but not after 30 days.
Conclusion: The association of early screen time with post concussion symptoms is not linear. Recommending moderation in screen time may be the best approach to clinical management.
Children need to strike a balance between avoiding boredom, deconditioning, isolation, and overexerting themselves physically or cognitively.
Cairncross M, al. Early Postinjury Screen Time and Concussion Recovery. Pediatrics. 2022
Category: EMS
Keywords: ambulance, crash, response, fatality, collision (PubMed Search)
Posted: 6/22/2023 by Jenny Guyther, MD
Click here to contact Jenny Guyther, MD
Prehosp Emerg Care. 2023;27(4):455-464. doi:10.1080/10903127.2022.
