Category: Neurology
Keywords: CNS, PNS, UMN, LMN, reflex, Babinski, tone (PubMed Search)
Posted: 10/14/2020 by WanTsu Wendy Chang, MD
Click here to contact WanTsu Wendy Chang, MD
| Central Nervous System | Peripheral Nervous System | |
| Pattern of Symptoms | • Hemibody involvement • Weakness of UE extensors • Weakness of LE flexors | • Distal involvement in polyneuropathy • Distal and proximal involvement in polyradiculoneuropathy • Proximal involvement in polyradiculopathy • Sensory often precedes motor symptoms • Pure proximal>distal weakness may be due to myopathy or NMJ disorder |
| Sensory Symptoms | • Central poststroke pain (hyperalgesia, allodynia) • Sensory level in spinal cord pathology • Proprioception involved early in dorsal column disorders | • Neuropathic pain (burning, tingling, shock-like) • Ascending sensory loss involving distal BLE>BUE in polyneuropathy • Proprioception involved late in polyneuropathy |
| Reflexes | • Hyperreflexia in affected limb(s) after acute period • Positive Babinski’s sign | • Hyporeflexia in affected limb(s) |
| Tone | • Increased after acute period | • Decreased |
Category: Critical Care
Posted: 10/13/2020 by Mike Winters, MBA, MD
(Updated: 2/2/2026)
Click here to contact Mike Winters, MBA, MD
Blood Pressure Management in Acute Ischemic Stroke
Herpich F, et al. Management of acute ischemic stroke. Crit Care Med. 2020; 48(11):1654-1663.
Category: Orthopedics
Keywords: Carpal Tunnel Syndrome, neuropathy (PubMed Search)
Posted: 10/10/2020 by Brian Corwell, MD
(Updated: 2/2/2026)
Click here to contact Brian Corwell, MD
Carpal Tunnel Syndrome (CTS)
The hallmark of classic CTS: pain or paresthesia (numbness and tingling) in a distribution that includes the median nerve territory, with involvement of the first three digits and the radial half of the fourth digit.
The symptoms of CTS are typically worse at night and often awaken patients from sleep.
Fixed sensory loss is usually a late finding
Involves the median-innervated fingers BUT spares the thenar eminence.
This pattern occurs because the palmar sensory cutaneous nerve arises proximal to the wrist and passes over, rather than through, the carpal tunnel.
Consider a more proximal lesion in cases involving sensory loss in the thenar eminence
Example: pronator syndrome
Category: Pharmacology & Therapeutics
Keywords: nitroglycerin, hypotension, PDE5 inhibitors (PubMed Search)
Posted: 10/3/2020 by Ashley Martinelli
Click here to contact Ashley Martinelli
Nitroglycerin is a potent vasodilator used most commonly for the treatment of angina and ACS. It can also be administered as a continuous infusion for acute management of a hypertensive emergency or sympathetic crashing acute pulmonary edema.
Most are aware of asking men for history of medications for erectile dysfunction (PDE5 inhibitors: sildenafil, tadalafil, vardenafil) but many overlook the fact that men and women may be on these medications chronically for pulmonary hypertension. Men can also be on these medications for the treatment of BPH. Be broad in your history taking and do not limit the discussion to erectile dysfunction or a specific gender.
Drug interaction:
-PDE5 inhibitors prevent the breakdown of cGMP
-Nitrates are nitric oxide donors that increase the production of cGMP
-The combination can lead to excessive vasodilation
If accidentally co-administered:
There is no antidote for this medication error. Support the patient with Trendelenburg positioning, fluid administration, and if needed, vasopressors such as norepinephrine until blood pressure stabilizes.
How long should you wait to administer nitrates after a patient takes a PDE5 Inhibitor?
Sildenafil and vardenafil: 24 h after last dose*
Tadalafil > 48 h after last dose*
*Even if acute ACS event
Schwartz BG, Kloner RA. Drug interactions with phosphodiesterase-5 inhibitors used for the treatment of erectile dysfunction or pulmonary hypertension. Circulation. 2010;122:88-95.
Category: Pediatrics
Keywords: uncomplicated appendicitis (PubMed Search)
Posted: 10/1/2020 by Cathya Olivas Michels, MD
Click here to contact Cathya Olivas Michels, MD
Acute appendicitis is the most common etiology requiring urgent abdominal surgery in children in the United States. Peak incidence occurs in the second decade of life, with male patients being more commonly affected than female patients. Classic manifestations of appendicitis occur in school-aged children and adolescents, but are often absent in younger children. Infants and young children <5 years are more likely to present with nonspecific or atypical findings, resulting in delays in diagnosis and higher rates of perforation.
Diagnosis is aided by clinical factors, lab findings, and ultrasound (+/- CT or MRI if ultrasound is equivocal).
Historically, the standard of care for acute appendicitis has been urgent operative management. However, in the past several years, there has been increasing literature supporting nonoperative management (antibiotics only) in adult patients with acute uncomplicated appendicitis. Additionally, there is a growing body of evidence demonstrating the safety and efficacy of nonoperative management for uncomplicated appendicitis in children.
Hartford and Woodward provide a review of the current literature on the nonoperative management of uncomplicated appendicitis in children. They conclude:
- The majority of recent prospective studies demonstrate early treatment success (0-30 days) of approximately 90% in pediatric patients undergoing nonoperative management.
- Factors associated with failure of nonoperative management in pediatric appendicitis: longer duration of symptoms (>48 hours), younger age (<5 years), and presence of appendicolith.
- Nonoperative management has been associated with
o Lower healthcare costs at 1 year
o Fewer disability days at 1 year
o No significantly different rate of complicated appendicitis
- Most trials to date involve a 24-48 hour initial course of broad spectrum IV antibiotics followed by oral antibiotics for a total of >/= 7 days as nonoperative management. Currently, there is no consensus on antibiotic regimen.
Bottom Line: Given the current evidence, nonoperative management may be a viable treatment option for low risk pediatric patients with uncomplicated appendicitis. The literature is not conclusive, thus we as medical providers in conjunction with our surgical colleagues, should consider numerous factors when discussing treatment options for acute appendicitis with patients and their families.
Hartford, E. A. & Woodward, G. A. Appendectomy or Not? An Update on the Evidence for Antibiotics Only Versus Surgery for the Treatment of Acute Appendicitis in Children. Pediatric Emergency Care 36, 6 (2020).
2.
Minneci, P. C. et al. Association of Nonoperative Management Using Antibiotic Therapy vs Laparoscopic Appendectomy With Treatment Success and Disability Days in Children With Uncomplicated Appendicitis. JAMA 324, 581 (2020).
3.
Minneci, P. C. et al. Effectiveness of Patient Choice in Nonoperative vs Surgical Management of Pediatric Uncomplicated Acute Appendicitis. JAMA Surg 151, 408 (2016).
Category: Critical Care
Keywords: Cardiac arrest, transport, EMS (PubMed Search)
Posted: 9/29/2020 by Lindsay Ritter, MD
Click here to contact Lindsay Ritter, MD
Historically, there has been debate on transporting outside hospital cardiac arrests, as well a trauma, with the question of whether to "scoop and run" or "stay and play".
Could hasty transportation of cardiac arrest patients put a damper on resuscitation quality?
A recent propensity-matched study in JAMA analyzed 192 EMS agencies across 10 N American sites.
Methods:
-Resuscitation Outcomes Consortium Cardiac Epidemiologic Registry, which counted 43,969 consecutive cases of nontraumatic adult EMS-treated OHCA (median age 67, 37% of whom were women) in 2011-2015.
-25% of these patients were transported to the hospital
-Matched 1:1 with patients in refractory arrest who were resuscitated on scene
-Primary outcome was survival to hospital discharge, secondary outcome survival to hospital discharge with a favorable neurological status
Results:
-Duration of out-of-hospital resuscitation was only 6 minutes longer in the intra-arrest transport group (29.1 and 22.9 minutes; not a statistically significant difference)
-Survival to hospital discharge was 3.8% for patients who underwent intra-arrest transport and 12.6% for those who received on-scene resuscitation
-In the propensity-matched cohort, which included 27,705 patients, survival to hospital discharge occurred in 4.0% of patients who underwent intra-arrest transport vs 8.5% who received on-scene resuscitation (risk difference, 4.6% [95% CI, 4.0- 5.1])
-Favorable neurological outcome occurred in 2.9% of patients who underwent intra-arrest transport vs 7.1% who received on-scene resuscitation (risk difference, 4.2% [95% CI, 3.5%-4.9%])
-Intra-arrest transport during resuscitation was associated with worse odds of survival to hospital discharge compared to on-scene resuscitation (4% vs 8.5%, RR 0.48, CI 0.43-0.54)
-Findings persisted across subgroups of initial shockable rhythm vs. non-shockable rhythms (most common initial rhythm was aystole), as well as EMS witness arrests vs. unwitnessed arrests
Conclusion:
-This study does not support the routine transportation of patients in cardiac arrest during rescuscitation.
-The neurologically intact survival benefit associated with on-scene resuscitation is both impressive and intriguing.
-However, what implications could this have on ECPR?
Limitations:
-Potential bias due to observational nature of study
-Duration of resuscitations very similar, unknown exactly how long transport times were or if this was in urban or rural populations
-External validity not generalizable due to heterogeneity of patient populations and EMS systems
-Further randomized clinical trials are required
Grunau B, Kime N, Leroux B, et al. Association of Intra-arrest Transport vs Continued On-Scene Resuscitation With Survival to Hospital Discharge Among Patients With Out-of-Hospital Cardiac Arrest. JAMA. 2020;324(11):1058–1067. doi:10.1001/jama.2020.14185
Category: Orthopedics
Keywords: Elder abuse, bruising, trauma (PubMed Search)
Posted: 9/26/2020 by Brian Corwell, MD
(Updated: 2/2/2026)
Click here to contact Brian Corwell, MD
Physical injury patterns associated with physical elder abuse
Elder abuse is both common and underrecognized
Between 5 and 10% of US older adults are victims of elder abuse annually
For many older adults, contact with a health care provider may represent their only contact outside the home
Differentiating physical elder abuse from unintentional trauma can be very difficult
A recent study compared these two groups with a case-control design
Study cases: 100 successfully prosecuted physical elder abuse cases from a single urban ED
Physical abuse victims were more likely to have:
Bruising (78% vs. 54%)
Injuries to maxillofacial, dental or neck region (67% vs. 28%)
Particularly the LEFT side
Neck injuries 6x more common is assault
Ear injuries occurred in assault but not in falls
Absence of fracture (8% vs. 22%)
Less likely to have lower extremity injuries (9% vs. 41%)
22% of victims had no visible injuries
Most common mechanism assault with hands or fists and pushing or shoving causing a fall
Take home: Consider elder abuse especially in cases of the above red flags
Rosen T, et al. Identifying Injury Patterns Associated With Physical Elder Abuse: Analysis of Legally Adjudicated Cases. Ann Emerg Med. 2020 Sep;76(3):266-276.
Category: Toxicology
Keywords: Black urine, toxicological cause (PubMed Search)
Posted: 9/24/2020 by Hong Kim, MD
Click here to contact Hong Kim, MD
What medication ingestion can lead to black urine?
There are many medical disorder and ingestion that can lead to change in urine colors.
Black discoloration of urine can be caused by:
Medication
Medical condition
Aycock, RD et al. Abnormal Urine Color. Southern Medical Journal 2012;105;43-47.
Category: Neurology
Keywords: cerebral venous thrombosis, CVT, symptoms, treatment, endovascular (PubMed Search)
Posted: 9/23/2020 by WanTsu Wendy Chang, MD
Click here to contact WanTsu Wendy Chang, MD
Bottom Line: Severity of CVT presentation depends on the location and clot burden. Anticoagulation is key, though consider endovascular intervention if patient does not improve or deteriorates despite anticoagulation.
Follow me on Twitter @EM_NCC
Category: Critical Care
Keywords: IPH, blood pressure management, outcome (PubMed Search)
Posted: 9/22/2020 by Quincy Tran, MD, PhD
Click here to contact Quincy Tran, MD, PhD
A retrospective study analyzed data from 757 patients with spontaneous intraparenchymal hemorrhage.
Within the first 6 hours of admission, patients who had systolic blood pressure reduction between 40 – 60 mm Hg (OR 1.9, 95% CI 1.1-3.5) or reduction ≥ 60 mm Hg (OR 1.9, 95%CI 1.01-3.8) were associated with almost double likelihood of poor discharge functional outcome (defined as modified Rankin Scale 3-6).
Additionally, large systolic blood pressure reduction ≥ 60 mm Hg in patients with large hematoma (≥ 30.47 ml) was associated with higher likelihood of very poor functional outcome (mRS 5-6).
Take home points: while more studies are still needed to confirm these observations, perhaps we may not want to drop blood pressure in patients with spontaneous intraparenchymal hemorrhage too much and too fast.
The Magnitude of Blood Pressure Reduction Predicts Poor In-Hospital Outcome in Acute Intracerebral Hemorrhage.
Afshin A Divani, Xi Liu, Alexander Petersen, Simona Lattanzi, Craig S Anderson, Wendy Ziai, Michel T Torbey, Tom J Moullaali, Michael L James, Alibay Jafarli, Stephan A Mayer, Jose I Suarez, J Claude Hemphill, Mario Di Napoli.
Neurocrit Care. 2020 Oct;33(2):389-398. doi: 10.1007/s12028-020-01016-z.
Category: Critical Care
Posted: 9/18/2020 by Caleb Chan, MD
Click here to contact Caleb Chan, MD
Systematic review and meta-analysis of 5 studies with a total of 929 patients comparing early vs. late initiation of norepinephrine in patients with septic shock
Primary outcome:
Secondary outcome:
Caveat:
Take home point:
Early norepinephrine usage may improve mortality in septic shock
Li Y, Li H, Zhang D. Timing of norepinephrine initiation in patients with septic shock: a systematic review and meta-analysis. Crit Care. 2020;24(1):488.
Category: Pediatrics
Keywords: prepubertal vaginal bleeding, mass (PubMed Search)
Posted: 9/18/2020 by Jenny Guyther, MD
(Updated: 2/2/2026)
Click here to contact Jenny Guyther, MD
- Urethral prolapse will appear as a protrusion of the distal urethra through the urinary meatus causing a “doughnut” sign.
- Risk factors include trauma, UTI, anatomical differences, and increased intraabdoiminal pressure from cough or constipation. There is a higher incidence in people of African descent.
- The chief complaint may include urethral mass and vaginal bleeding.
- There is a bimodal age distribution (prepuberty and postmetapause) due to a relative estrogen deficiency.
-Treatment is with estrogen cream and sitz baths for 4- 6 weeks.
McCaskill A, Inabinet C, Tomlin K et al. Prepubertal Genital Bleeding: Examination and Differential Diagnosis in Pediatric Female Patients. The Journal of Emergency Medicine 2018; 55(4): 97-100.
Category: Orthopedics
Keywords: Spine fracture, decision rule (PubMed Search)
Posted: 9/12/2020 by Brian Corwell, MD
(Updated: 2/2/2026)
Click here to contact Brian Corwell, MD
A recent study looked at thoracic spinal fractures in the era of the trauma panscan
NEXUS Chest CT Study from 2011 to 2014 at 9 Level I trauma centers.
Goal: To describe the identification rate and types of thoracic spine fractures.
Inclusion: age over 14 years, blunt trauma occurring within 6 hours of ED presentation, and chest CT imaging during ED evaluation.
11,477 subjects, 217 (1.9%) had a thoracic spine fracture
The majority of spine fractures in patients who had both chest x-ray and CT were observed on CT only (91%). 50% had more than 1 thoracic spinal level involved (mean 2.1). 22% had associated cervical fractures and 25% had associated lumbar fractures.
64% had vertebral body fractures
45% had posterior column fractures
28% had compression fractures
6% had burst fractures
Many patients (62%) had associated thoracic injuries such as
Rib fractures (45%)
PTX (36%)
Clavicle fracture (18%)
Scapular fracture (17%)
Hemothorax (15%)
100 patients had clinically significant thoracic spine fractures.
Thoracic spine fractures are relatively uncommon in adult patients with blunt trauma.
If thoracic spine fracture is suspected clinically, radiography is not an effective screen and clinician should consider CT. If not suspected, guidelines discourage ordering CT to screen for this injury because of effective screening instruments, the diagnosis of clinically insignificant injuries and radiation exposure.
All clinically significant thoracic spine fractures would have been detected by the NEXUS Chest CT decision instrument.
https://www.mdcalc.com/nexus-chest-ct-decision-instrument-ct-imaging
Bizimungu R, Sergio Alvarez, Baumann BM, et al. Thoracic Spine Fracture in the Panscan Era. Ann Emerg Med. 2020;76(2):143-148.
Category: Toxicology
Keywords: ECMO, poisoning, trend in US (PubMed Search)
Posted: 9/10/2020 by Hong Kim, MD
(Updated: 2/2/2026)
Click here to contact Hong Kim, MD
Extracorporeal membrane oxygenation use is increasing in the US for acute poisoning.
A retrospective study of the National Poison Data System from 2000 to 2018 identified 407 ECMO cases (332 adults – age > 12 years, 75 pediatric – age < 12 years). Increase in ECMO use were more notable in adult population.
Characteristics
Intentional exposure
Most common class of drug/poison exposure in adults
Most common class of drug/poison exposure in children
Most common states that used ECMO for poisoning
Conclusion
Category: Neurology
Keywords: cerebral venous thrombosis, CVT, prothrombotic, headache (PubMed Search)
Posted: 9/10/2020 by WanTsu Wendy Chang, MD
Click here to contact WanTsu Wendy Chang, MD
Bottom Line: The incidence of CVT is increasing with rate of increase higher in males and older females. Consider CVT beyond traditional risk factors.
Follow me on Twitter @EM_NCC
Category: Critical Care
Keywords: resuscitation, ultrasound, VExUS, venous congestion (PubMed Search)
Posted: 9/8/2020 by Kami Windsor, MD
Click here to contact Kami Windsor, MD
While the invasive monitoring of central venous pressure (CVP) in the critically ill septic patient has gone the way of also transfusing them to a hemoglobin of 10 mg/dL, it remains that an elevated CVP is associated with higher mortality1,2 and renal failure.2,3
Extrapolating from existing data looking at hepatic vein, portal vein, and renal vein pulsatility as measures of systemic venous hypertension and congestion,4,5,6 Beaubien-Souligny et al. developed the venous excess ultrasound (VExUS) grading system incorporating assessment of all 3, plus the IVC, using US to stage severity of venous congestion in post-cardiac surgery patients.7 They evaluated several variations, determining that the VExUS-C grading system was most predictive of subsequent renal dysfunction.
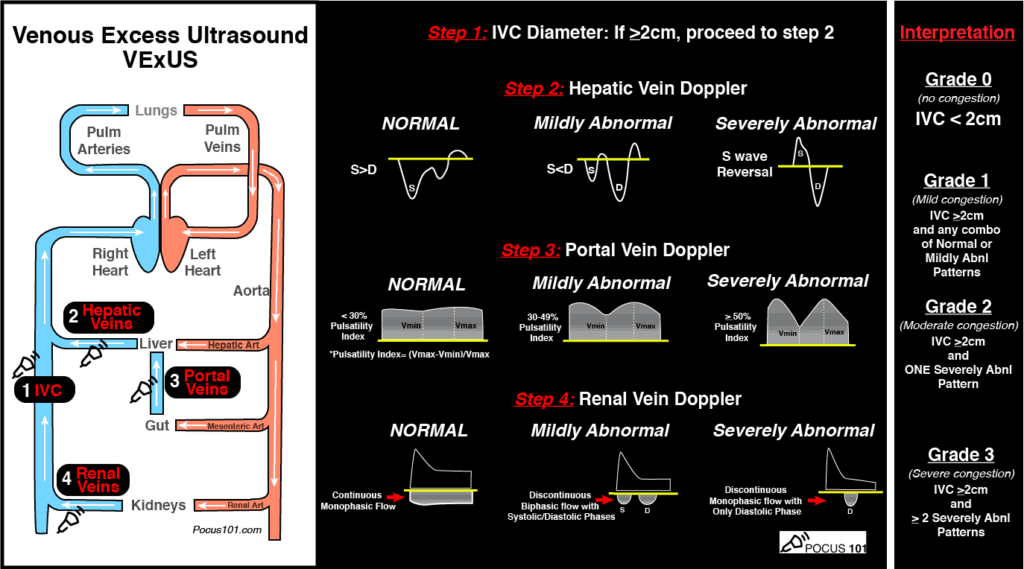
(Image from www.pocus101.com)
High Points
VExUS Grade 3 (severe) venous congestion:
Caveats
Clinical Uses
A great how-to can be found here:
https://www.pocus101.com/vexus-ultrasound-score-fluid-overload-and-venous-congestion-assessment/
1. Li DK, Wang XT, Liu DW. Association between elevated central venous pressure and outcomes in critically ill patients. Ann Intensive Care. 2017;7(1):83. doi:10.1186/s13613-017-0306-1
2. Chen KP, Cavender S, Lee J, et al. Peripheral Edema, Central Venous Pressure, and Risk of AKI in Critical Illness. Clin J Am Soc Nephrol. 2016;11(4):602-608.
3. Chen CY, Zhou Y, Wang P, Qi EY, Gu WJ. Elevated central venous pressure is associated with increased mortality and acute kidney injury in critically ill patients: a meta-analysis. Crit Care. 2020;24(1):80. doi:10.1186/s13054-020-2770-5
4. Iida N, Seo Y, Sai S, et al. Clinical Implications of Intrarenal Hemodynamic Evaluation by Doppler Ultrasonography in Heart Failure. JACC Heart Fail. 2016;4(8):674-682. doi:10.1016/j.jchf.2016.03.016
5. Ikeda Y, Ishii S, Yazaki M, et al. Portal congestion and intestinal edema in hospitalized patients with heart failure. Heart Vessels. 2018;33(7):740-751. doi:10.1007/s00380-018-1117-5.
6. Beaubien-Souligny W, Benkreira A, Robillard P, et al. Alterations in Portal Vein Flow and Intrarenal Venous Flow Are Associated With Acute Kidney Injury After Cardiac Surgery: A Prospective Observational Cohort Study. J Am Heart Assoc. 2018;7(19):e009961. doi:10.1161/JAHA.118.009961
7. Beaubien-Souligny W, Rola P, Haycock K, et al. Quantifying systemic congestion with Point-Of-Care ultrasound: development of the venous excess ultrasound grading system. Ultrasound J. 2020;12(1):16. doi:10.1186/s13089-020-00163-w
Category: Pharmacology & Therapeutics
Keywords: esmolol, cardiac arrest, ventricular tachycardia, ventricular fibrillation (PubMed Search)
Posted: 9/5/2020 by Ashley Martinelli
(Updated: 2/2/2026)
Click here to contact Ashley Martinelli
| | Beta-blockade N=22 | Control N= 44 | OR/CI |
| Temporary ROSC, n (%) | 19 (86.4) | 14 (31.8) | OR 14.46, 95% CI 3.63-57.57 |
| Sustained ROSC, n (%) | 13 (59.1) | 10 (22.7) | OR 5.76, 95% CI 1.79-18.52 |
| Survival with neurological function, n (%) | 6 (27.3) | 4 (9.1) | OR 4.42; 95% CI 1.05-18.56 |
Category: Pediatrics
Keywords: button battery, pediatrics, esophageal injuries (PubMed Search)
Posted: 9/4/2020 by Prianka Kandhal, MD
Click here to contact Prianka Kandhal, MD
Ingestion of a button battery is a can't-miss diagnosis with a very high risk for causing severe esophageal injury. There are about 3000 button battery ingestions per year, and this is increasing because electronics are becoming more and more prevalent.
Severe damage to the esophagus occurs within 2 hours. On your lateral view, the end with narrowing is the negative end, which triggers a hydrolysis reaction that results in an alkaline caustic injury and, ultimately, liquefactive necrosis.
Children can present with nonspecific symptoms and if the ingestion was not witnessed, they are at high risk for delays in diagnosis. Additionally, in the community setting, there can be further delays in definitive treatment (endoscopic removal) due to difficulty in calling teams in or transporting to other facilities.
Anfang et al. looked into ways to mitigate damage to esophageal tissue. They did an in vitro study on porcine esophageal tissue, measuring the pH with different substances applied. They tried apple juice, orange juice, gatorade, powerade, pure honey, pure maple syrup, and carafate. They then repeated the study in vivo on piglets with button batteries left in the esophagus and ultimately did gross and histological examination of the esophageal tissue.
Honey and carafate demonstrated protective effects both in vitro and in vivo. They neutralized pH changes, decreased full-thickness esophageal injury, and decreased outward extension of injury into deep muscle.
Take Home Point: If a child is found to have a button battery in the esophagus, while definitive management is still emergent endoscopic removal, early and frequent ingestion of honey (outside of the hospital) and Carafate (in the hospital) may help reduce the damage done to the tissue in the interim. The authors recommend 10ml every 10 minutes.
Anfang RR, Jatana KR, Linn RL, et al. pH-Neutralizing Esophageal Irrigations as a Novel Mitigation Strategy for Button Battery Injury. The Laryngoscope. 2019; 129:49-57.
Category: Critical Care
Keywords: Renal Replacement Therapy (PubMed Search)
Posted: 9/1/2020 by Kim Boswell, MD
(Updated: 2/2/2026)
Click here to contact Kim Boswell, MD
STARRT-AKITrial
The Standard versus Accelerated initiation of Renal Replacement Therapy in Acute Kidney Injury
The development of acute kidney injury (AKI) in the critical care setting portends a greater morbidity and mortality for patients. Additionally, it places the patient at high risk of complications and requires a greater use of resources. Several studies in the past have examined if the timing of initiation of renal replacement therapy (RRT) would result in a mortality benefit, but have failed to demonstrate consistent outcomes.
The STARRT-AKI trial was a multinational, randomized controlled trial designed to determine if early initiation of RRT in critically ill adult patients with AKI lowered the risk of 90-day mortality. The Kidney Disease Improving Global Outcomes (KDIGO) classification was used to define AKI and over 2900 patients were randomly assigned to two groups over a 4 year period. Exclusion criteria included: recent RRT, a renal transplant within the preceding year, advanced CKD, an overdose necessitating RRT, or a strong suspicion of obstruction or autoimmune/vascular cause of their AKI.
Groups:
Outcomes/Results:
Take home points:
Timing of Initiation of Renal-Replacement Therapy in Acute Kidney Injury. STARRT-AKI Investigators; Canadian Critical Care Trials Group, the Australian and New Zealand Intensive Care Society Clinical Trials Group, the United Kingdom Critical Care Research Group, the Canadian Nephrology Trials Network, and the Irish Critical Care Trials Group, Bagshaw SM, Wald R, Adhikari NKJ, et al. N Engl J Med. 2020 Jul 16;383(3):240-251.
Category: Neurology
Keywords: trigeminal neuralgia, TN, tic douloureux, neuropathic facial pain (PubMed Search)
Posted: 8/26/2020 by WanTsu Wendy Chang, MD
Click here to contact WanTsu Wendy Chang, MD
Bottom Line: New onset trigeminal neuralgia needs workup for its etiology. Carbamazepine and oxcarbazepine can be effective for symptom management though continuous or long-lasting pain exacerbations are difficult to treat.
Follow me on Twitter @EM_NCC
