Category: Critical Care
Keywords: COVID-19, Anticoagulation, Thromboembolism (PubMed Search)
Posted: 4/7/2021 by Mark Sutherland, MD
Click here to contact Mark Sutherland, MD
Two items from the recent INSPIRATION trial UMEM pearl were very well pointed out by our own Dr. Michael Scott and require clarification. Thank you to all our readers for their close attention, and please know that we always appreciate you reaching out with questions/comments.
Category: Critical Care
Keywords: COVID-19, Anticoagulation, Thromboembolism (PubMed Search)
Posted: 4/7/2021 by Mark Sutherland, MD
Click here to contact Mark Sutherland, MD
COVID-19 is generally regarded as a hypercoagulable state, and the role of pulmonary emboli and other VTE in COVID remains unclear. As a result, how to optimally provide prophylactic anticoagulation in COVID-19 patients who are not known to have VTE has been a point of debate.
The INSPIRATION trial looked at 600 patients admitted to academic ICUs in Iran, and compared what is often-referred to as "intermediate-dose" prophylaxis (in this case 1 mg/kg daily of enoxaparin) to standard dose prophylaxis (40 mg/day of enoxaparin). The study utilized a combined endpoint of venous thromboembolism, arterial thromboembolism, need for ECMO, or mortality. As a reminder, composite endpoints can skew results. However, the dose and type of anticoagulant chosen is similar to many academic centers around the world, and pharmacy guidelines often recommend providing this type of "intermediate-dose" prophylaxis in COVID-19 patients, sometimes based on clinical status, d-dimer or other coagulation-related patient-data. As with many things with COVID-19, this practice is based on limited data.
There was no significant difference between groups in the primary outcome (45.7% in intermediate ppx group vs 44.1% in standard group), and while safety outcomes were similar (major bleeding in 2.5% in the intermediate ppx group vs 1.4% in standard group), the intermediate regimen failed to demonstrate non-inferiority to the standard regimen for major bleeding.
Intermediate vs standard-dose ppx was similar in this study with a small, but statistically significant increase in major bleeding in the intermediate-dose group.
Bottom Line: Although this study had methodologic flaws and there are external validity concerns, the INSPIRATION trial supports the notion that standard dose (e.g. 40 mg/g/kg/day enoxaparin) and intermediate-dose (e.g. 1 mg/kg/day enoxaparin) VTE prophylaxis are equivalent in critically ill COVID-19 patients who do not already have a known VTE in terms of preventing negative VTE outcomes. Intermediate-dose may be associated with increased bleeding. As more critically ill patients require ED boarding, the dose of VTE prophylaxis may remain controversial, but the need to start it remains an important consideration.
INSPIRATION Investigators, Sadeghipour P, Talasaz AH, Rashidi F, Sharif-Kashani B, Beigmohammadi MT, Farrokhpour M, Sezavar SH, Payandemehr P, Dabbagh A, Moghadam KG, Jamalkhani S, Khalili H, Yadollahzadeh M, Riahi T, Rezaeifar P, Tahamtan O, Matin S, Abedini A, Lookzadeh S, Rahmani H, Zoghi E, Mohammadi K, Sadeghipour P, Abri H, Tabrizi S, Mousavian SM, Shahmirzaei S, Bakhshandeh H, Amin A, Rafiee F, Baghizadeh E, Mohebbi B, Parhizgar SE, Aliannejad R, Eslami V, Kashefizadeh A, Kakavand H, Hosseini SH, Shafaghi S, Ghazi SF, Najafi A, Jimenez D, Gupta A, Madhavan MV, Sethi SS, Parikh SA, Monreal M, Hadavand N, Hajighasemi A, Maleki M, Sadeghian S, Piazza G, Kirtane AJ, Van Tassell BW, Dobesh PP, Stone GW, Lip GYH, Krumholz HM, Goldhaber SZ, Bikdeli B. Effect of Intermediate-Dose vs Standard-Dose Prophylactic Anticoagulation on Thrombotic Events, Extracorporeal Membrane Oxygenation Treatment, or Mortality Among Patients With COVID-19 Admitted to the Intensive Care Unit: The INSPIRATION Randomized Clinical Trial. JAMA. 2021 Mar 18. doi: 10.1001/jama.2021.4152. Epub ahead of print. PMID: 33734299.
Category: Pharmacology & Therapeutics
Keywords: Pyelonephritis, Outpatient, Fluoroquinolones, TMP-SMX, Beta-lactams (PubMed Search)
Posted: 4/3/2021 by Wesley Oliver
Click here to contact Wesley Oliver
While fluoroquinolones have fallen out of favor for many indications due to the ever growing list of adverse effects, they still play an important role in the outpatient treatment of pyelonephritis. Fluoroquinolones and TMP-SMX are the preferred agents due to higher failure rates with beta-lactams.
Preferred Therapies:
Ciprofloxacin 500 mg PO BID*
Levofloxacin 750 mg PO daily*
TMP-SMX 1 DS tab PO BID**
*Consider a single dose of long-acting parenteral agent, such as ceftriaxone, if community prevalence of fluoroquinolone resistance >10%.
**Consider a single dose of long-acting parenteral agent, such as ceftriaxone, if using TMP-SMX.
Alternative Therapies#:
Cefpodoxime 200 mg PO BID
Cefdinir 300 mg PO BID
#Beta-lactams are not preferred agents due to higher failure rates when compared to fluoroquinolones. Consider a single dose of long-acting parenteral agent, such as ceftriaxone, if using beta-lactams.
Duration of Therapy: 10-14 days
Take Home Point:
Utilize ciprofloxacin, levofloxacin, or TMP-SMX over beta-lactams when discharging patients with oral antibiotics for pyelonephritis.
Gupta K, Hooton TM, Naber KG, et al. International clinical practice guidelines for the treatment of acute uncomplicated cystitis and pyelonephritis in women: A 2010 update by the Infectious Diseases Society of America and the European Society for Microbiology and Infectious Diseases. Clin Infect Dis 2011; 52:e103.
Urinary Tract Infections. UMMS Clinical Practice Guidelines. Sanford Guide, 2021. Accessed April 2, 2021. https://webedition.sanfordguide.com/en/umms/syndromes/urinary-tract-infections.
Category: Critical Care
Posted: 3/30/2021 by Mike Winters, MBA, MD
Click here to contact Mike Winters, MBA, MD
Improving Compliance with Lung-Protective Ventilation
Tallman CMI, et al. Impact of provding a tape measure on the provision of lung-protective ventilation. West J Emerg Med. 2021; 22:389-93.
Category: Toxicology
Keywords: diphenhydramine overdose, seizure, ventricular dysrhythmia, severe toxicity (PubMed Search)
Posted: 3/25/2021 by Hong Kim, MD
Click here to contact Hong Kim, MD
Diphenhydramine is commonly involved in overdose or misused. Although it is primarily used for its anti-histamine property, it also has significant antimuscarinic effect.
A recent retrospective study investigated the clinical characteristics associated with severe outcomes in diphenhydramine overdose using the multi-center Toxicology Investigators Consortium (ToxIC) Registry.
Severe outcomes were defined as any of the following:
Results
863 cases of isolated diphenhydramine ingestion were identified between Jan 1, 2010 to Dec 31, 2016
Most common symptoms:
Factors associated with severe outcome
Conclusion
Hughes AR et al. Clinical and patient characteristics associated with severe outcome in diphenhydramine toxicity. Clin Toxicol (Phila) 2021.
Category: Pediatrics
Keywords: Chest pain, ischemia, pediatrics, myocarditis (PubMed Search)
Posted: 3/19/2021 by Jenny Guyther, MD
(Updated: 2/2/2026)
Click here to contact Jenny Guyther, MD
Even though acute myocardial ischemia (AMI) does not present as commonly in the pediatric patient as in the adult and the literature is limited, it is reasonable to obtain a troponin when acute cardiac ischemia is suspected based on the history and physical exam.
Recreational drugs including cocaine, amphetamine, cannabis, Spice, and K2 (cannabis derivatives) have been shown to result in myocardial injury including AMI. Coronary vasospasm secondary to drug use is well documented in the pediatric population. While cocaine use is a known risk factor for coronary vasospasm, the same condition has been reported in pediatric patients after marijuana use.
In a study of pediatric patients with blunt chest trauma, 3 of 4 patients with electrocardiographic or echocardiographic evidence of cardiac injury had elevations in troponin I above 2.0 ng/mL. Cardiac troponins are an accurate tool for screening for cardiac contusion after blunt chest trauma in pediatric patients even with limited data.
Cardiac troponins are also useful in the evaluation for myocarditis. In one study, myocarditis was the most common diagnosis (27%) in pediatric ED patients presenting with chest pain and an increased troponin. Eisenberg et al showed a 100% sensitivity and an 85% specificity for myocarditis using a troponin of 0.01 ng/mL or greater as a cut off. A normal troponin using this cutoff can be used to exclude myocarditis. Abnormal troponin in the first 72 hours of hospitalization in pediatric patients with viral myocarditis is associated with subsequent need for extracorporeal membrane oxygenation and IVIg.
Bottom line: Troponin can be used in pediatric patients with clinical concern for cardiac ischemia, cardiac contusion and myocarditis
Brown JL, Hirsh DA, Mahle WT. Use of troponin as a screen for chest pain in the pediatric emergency department. Pediatr Cardiol. 2012;33(2):337-342. doi:10.1007/s00246-011-0149-8
Drossner DM, Hirsh DA, Sturm JJ, et al. Cardiac disease in pediatric patients presenting to a pediatric ED with chest pain. Am J Emerg Med. 2011;29(6):632-638. doi:10.1016/j.ajem.2010.01.011
Thankavel PP, Mir A, Ramaciotti C. Elevated troponin levels in previously healthy children: value of diagnostic modalities and the importance of a drug screen. Cardiol Young. 2014;24(2):283-289. doi:10.1017/S1047951113000231
Yolda? T, Örün UA. What is the Significance of Elevated Troponin I in Children and Adolescents? A Diagnostic Approach. Pediatr Cardiol. 2019;40(8):1638-1644. doi:10.1007/s00246-019-02198-w
Adams JE, Dávila-Román VG, Bessey PQ, Blake DP, Ladenson JH, Jaffe AS. Improved detection of cardiac contusion with cardiac troponin I. Am Heart J. 1996;131(2):308-312. doi:10.1016/s0002-8703(96)
Hirsch R, Landt Y, Porter S, et al. Cardiac troponin I in pediatrics: normal values and potential use in the assessment of cardiac injury. J Pediatr. 1997;130(6):872-877. doi:10.1016/s0022-3476(97)
Eisenberg MA, Green-Hopkins I, Alexander ME, Chiang VW. Cardiac troponin T as a screening test for myocarditis in children. Pediatr Emerg Care. 2012;28(11):1173-1178. doi:10.1097/PEC.
Category: Toxicology
Keywords: occupational poisoning (PubMed Search)
Posted: 3/18/2021 by Hong Kim, MD
(Updated: 2/2/2026)
Click here to contact Hong Kim, MD
There are different occupational hazards depending on the nature of one’s trade/skill/employment. Although healthcare providers may not always inquire about patient’s occupation, knowledge of a patient’s occupation may provide insightful information when caring for patients with acute poisoning.
From a recent retrospective study of National Poison Data System, the top 10 occupational toxicants were:
Top 10 occupational toxicants associated with fatalities were:
Downs JW et al. Descriptive epidemiology of clincally signifcant occupational poisonings, United States, 2008-2018. Clin Toxicol (Phila). 2021. PMID: 33703981
Category: Critical Care
Posted: 3/16/2021 by Lindsay Ritter, MD
Click here to contact Lindsay Ritter, MD
The PARAMEDIC2 trial in NEJM 2018 studied the outcomes of the use of epinephrine in outside hospital cardiac arrest (OHCA) on survival and neurological outcome.
Methods: Conducted in Britain, randomized 8007 patients to receive either epinepherine 1mg (n=4012) or placebo (n=3995) as part of standard CPR for out-of-hosptial arrest. Their primary outcome was survival at 30 days and their secondary outcomes included length of stay as well as neurological outcomes at 30 days and 3 months.
Results: The epinepherine group had improved survival to hospital admission (23% vs. 8%), at 30 days (3.2% vs. 2.4%) or at 3 months (3% vs. 2.2%). Favourable neurological outcomes, however, had no statistical difference at both hospital discharge and at 3 months.
Bottom line: Epinephrine improves ROSC, though with poor neurological outcomes.
Important facts:
Recently, a follow up of the PARAMEDIC2 trial was completed in Resuscitation.
They reported long-term survival, quality of life, functional and cognitive outcomes at 3, 6 and 12-months.
Results: At 6 months, 78 (2.0%) of the patients in the adrenaline group and 58 (1.5%) of patients in the placebo group had a favourable neurological outcome (adjusted odds ratio 1.35 [95% confidence interval: 0.93, 1.97]). 117 (2.9%) patients were alive at 6-months in the adrenaline group compared with 86 (2.2%) in the placebo group (1.43 [1.05, 1.96], reducing to 107 (2.7%) and 80 (2.0%) respectively at 12-months (1.38 [1.00, 1.92]). Measures of 3 and 6-month cognitive, functional and quality of life outcomes were reduced, but there was no strong evidence of differences between groups.
Bottom line: Epinephrine improves survival at 12 months, but poor neurological outcomes remain.
Haywood KL, Ji C, Quinn T, Nolan JP, Deakin CD, Scomparin C, Lall R, Gates S, Long J, Regan S, Fothergill RT, Pocock H, Rees N, O'Shea L, Perkins GD. Long term outcomes of participants in the PARAMEDIC2 randomised trial of adrenaline in out-of-hospital cardiac arrest. Resuscitation. 2021 Mar;160:84-93. doi: 10.1016/j.resuscitation.2021.01.019. Epub 2021 Jan 30. PMID: 33524488.
Perkins GD, Ji C, Deakin CD, Quinn T, Nolan JP, Scomparin C, Regan S, Long J, Slowther A, Pocock H, Black JJM, Moore F, Fothergill RT, Rees N, O'Shea L, Docherty M, Gunson I, Han K, Charlton K, Finn J, Petrou S, Stallard N, Gates S, Lall R; PARAMEDIC2 Collaborators. A Randomized Trial of Epinephrine in Out-of-Hospital Cardiac Arrest. N Engl J Med. 2018 Aug 23;379(8):711-721. doi: 10.1056/NEJMoa1806842. Epub 2018 Jul 18. PMID: 30021076.
Category: Orthopedics
Keywords: patellofemoral, knee, pain (PubMed Search)
Posted: 3/13/2021 by Michael Bond, MD
(Updated: 2/2/2026)
Click here to contact Michael Bond, MD
Bottom Line: In a recent meta-analysis the risk factors for patellofemoral syndrome are weak hip abduction strength, quadricep weakness in military recruits, and increased hip strength in adolescence.
PatelloFemoral Syndrome: Patellofemoral pain is not clearly understood and is believed to be multi-factorial. Numerous factors have been proposed including muscle weakness, damage to cartilage, patella maltracking, as well as others. Patient often complain of anterior knee that is aggravated by walking up and down stairs or squatting. Patellofemoral pain is extremely common. In the general population the annual prevalence for patellofemoral pain is approximately 22.7%, and in adolescents it is 28.9%.
Though commonly taught, the following have no evidence to support that they are a risk factor for patellofemoral syndrome: Age, Height, Weight, BMI, Body Fat or Q Angle of patella
Category: Neurology
Keywords: Idiopathic intracranial hypertension, IIH, pseudotumor cerebri, obesity, healthcare utilization (PubMed Search)
Posted: 3/10/2021 by WanTsu Wendy Chang, MD
Click here to contact WanTsu Wendy Chang, MD
Bottom Line: The incidence and prevalence of IIH is increasing, likely related to rising rate of obesity. This has also been associated with more healthcare utilization compared to the general population.
Category: Critical Care
Keywords: sepsis recognition, antibiotics administration, mortality, (PubMed Search)
Posted: 3/10/2021 by Quincy Tran, MD, PhD
(Updated: 2/2/2026)
Click here to contact Quincy Tran, MD, PhD
Background:
The association between time intervals of ED antibiotic administration and outcome has been controversial. While single studies showed there was increased mortality associated with delayed antibiotic administration (1-3). A meta-analysis of 13 studies and 33000 patients showed that there was no mortality difference between septic patients receiving immediate Abx (< 1 hour) vs. those receiving early abx (1-3 hours) (4).
Since delay in recognition of sepsis (defined as ED triage to Abx order) and delay in antibiotics delivery (Abx order to administration) contribute to total delay of Abx administration, a new retrospective study (3) attempted to investigate the contributions of either factor to hospital mortality.
Results:
The study used generalized linear mixed models and involved 24000 patients.
For All patients and outcome of hospital mortality:
Recognition delay (ED triage to Abx order): OR 2.7 (95% CI 1.5-4.7)*
Administration delay at 2-2.5 hours (Abx order to administration): OR 1.5 (1.1-2.0)
These results was associated with non-statistical significance in patients with septic shocks.
Conclusion:
Delayed recognition of sepsis was associated with higher hospital mortality. Longer delay of abx administration was also associated with increased risk of hospital mortality.
1.Kumar A, Roberts D, Wood KE, et al: Duration of hypotension before initiation of effective antimicrobial therapy is the critical determinant of survival in human septic shock. Crit Care Med. 2006; 34:1589–1596
2. Ferrer R, Martin-Loeches I, Phillips G, et al: Empiric antibiotic treatment reduces mortality in severe sepsis and septic shock from the first hour: Results from a guideline-based performance improvement program. Crit Care Med 2014; 42: 1749–1755
3. Seymour CW, Gesten F, Prescott HC, et al: Time to treatment and mortality during mandated emergency care for sepsis. N Engl J Med 2017; 376:2235–2244.
4. Rothrock SG et al. Outcome of immediate versus early antibiotics in severe sepsis and septic shock: A systematic review and meta-analysis. Ann Emerg Med 2020 Jun 24; [e-pub]. (https://doi.org/10.1016/j.annemergmed.2020.04.042)
Category: Pharmacology & Therapeutics
Posted: 3/7/2021 by Ashley Martinelli
(Updated: 2/2/2026)
Click here to contact Ashley Martinelli
Tranexamic acid (TXA) is an antifibrinolytic medication that has been trialed in previous small studies to treat epistaxis. The data to this point has not reliably shown a reduction in bleeding at 30 minutes, but has demonstrated an increased rate of discharge at 2 hours and a reduction in re-bleeding events.
The NoPAC study was the largest study to date on TXA for epistaxis. It was a double-blind, placebo-controlled, randomized study of TXA in adult patients with persistent atraumatic epistaxis to determine if TXA use decreased the rate of anterior nasal packing. Patients were excluded if they had trauma, out of hospital nasal packing, allergy to TXA, nasopharyngeal malignancy, hemophilia, pregnancy, or if they were referred to ENT.
Eligible patients completed 10 minutes of first aid measures followed by 10 minutes of topical vasoconstrictor application prior to randomization to either placebo of 200mg TXA soaked dental rolls inserted in the nare.
496 patients were enrolled. The average patient was 70 years old with stable vitals 150/80mmHg, HR 80 bpm with >60% on oral anticoagulants.
TXA did not reduce the need for anterior nasal packing: 100 (41.3% placebo) vs 111 (43.7% TXA) OR 1.11 (0.77-1.59). There were no differences in the rates of adverse events.
Bottom Line: TXA does not improve rates of anterior nasal packing for patients with persistent epistaxis.
Reuben A, Appelboam A, Stevens KN, et al. The use of tranexamic acid to reduce the need for nasal packing in epistaxis (NoPAC): Randomized controlled trial. Ann Emerg Med 2021;1-10. https://doi.org/10.1016/j.annemergmed.2020.12.013
Category: Toxicology
Keywords: massive acetaminophen overdose, standard NAC, hepatotoxicity (PubMed Search)
Posted: 3/4/2021 by Hong Kim, MD
Click here to contact Hong Kim, MD
Recently, there has been questions if standard n-acetylcysteine (NAC) dose is adequate for massive acetaminophen (APAP) overdose (ingestion of > 32 gm or APAP >300 mcg/mL).
A retrospective study from a single poison center (1/1/2010 to 12/31/2019) investigated the clinical outcome of massive APAP overdose (APAP > 300 mcg/mL at 4 hour post ingestion) treated with standard dosing of NAC.
Results
1425 cases of APAP overdose identified; 104 met the criteria of massive APAP overdose.
Among cases that received NAC within 8 hours post ingestion (n=44)
Among cases that received NAC > 8 hours post ingestion (n=60)
Odds of hepatotoxicity
Conclusion
Category: Critical Care
Posted: 3/2/2021 by Caleb Chan, MD
(Updated: 2/2/2026)
Click here to contact Caleb Chan, MD
Clinical Question:
Methods:
Results:
Take-home points:
Hughes CG, Mailloux PT, Devlin JW, et al. Dexmedetomidine or propofol for sedation in mechanically ventilated adults with sepsis. N Engl J Med. Published online February 2, 2021:NEJMoa2024922.
Category: Orthopedics
Keywords: Distal radius fracture, wrist, splint (PubMed Search)
Posted: 2/27/2021 by Brian Corwell, MD
(Updated: 2/2/2026)
Click here to contact Brian Corwell, MD
Home management versus PCP follow-up of patients with distal radius buckle (torus) fractures
A recent study investigated outcomes of patients with distal radius buckle fractures who were randomized to
Versus
Noninferior study
Torus/buckle fractures of the distal radius are the most common fractures in childhood occurring on average in 1 in 25 children
This is a stable fracture typically treated with removable wrist splint and very rarely require orthopedic intervention
Outcome: functional recovery at 3 weeks
Randomized controlled trial at a tertiary care children’s hospital
All radiographs reviewed by pediatric radiologist with MSK specialization
149 patients. Mean age 9.5 years. 54.4% male
Telephone follow-up at 3 and 6 weeks following ED discharge by blinded interviewer
Primary outcome was comparison of Activities Scale for Kids-performance scores between groups at 3 weeks
Outcomes: Home management performance score was 95.4% and PCP follow-up group was 95.9%. Mean cost savings were $100.10.
Conclusion: Home management is at least as good as PCP follow-up with respect to functional recovery in ED patients with distal radius buckle fractures.
Colaco et al. Home management versus primary care physician follow-up of patients with distal radius buckle fractures: A randomized controlled trial. Ann Emerg Med. 2021
Category: Neurology
Keywords: Bell's palsy, facial palsy, Lyme disease, Borrelia burgdorferi (PubMed Search)
Posted: 2/24/2021 by WanTsu Wendy Chang, MD
(Updated: 2/2/2026)
Click here to contact WanTsu Wendy Chang, MD
Bottom Line: In a Lyme-endemic area, the incidence of positive Lyme tests and Bell’s palsy are highest in the Lyme months. This seasonal variation may help guide the management of patients with Bell’s palsy.
Pacheco A, Rutler O, Valenzuela I, Feldman D, Eskin B, Allegra JR. Positive tests for Lyme disease and emergency department visits for Bell’s Palsy patients. J Emerg Med. 2020;59(6):820-827.
Follow me on Twitter @EM_NCC
Category: Critical Care
Keywords: HACOR, NIV, noninvasive ventilation, acute respiratory failure (PubMed Search)
Posted: 2/2/2021 by Kami Windsor, MD
(Updated: 2/23/2021)
Click here to contact Kami Windsor, MD
Background: In respiratory failure due to COPD and cardiogenic pulmonary edema, noninvasive positive pressure ventilation decreases need for intubation and improves mortality,1 while its utility in other scenarios such as ARDS and pneumonia has yet to be proven.1,2 We know that patients on NIV with delays to needed intubation have a higher mortality,1,3 but intubation and mechanical ventilation come with risks that it is preferable to avoid if possible.
So how and when can we determine that NIV is not working?
The HACOR (Heart rate, Acidosis, Consciousness, Oxygenation, Respiratory rate) score at 1 hour after NIV initiation has been demonstrated to be highly predictive of NIV failure requiring intubation.4,5
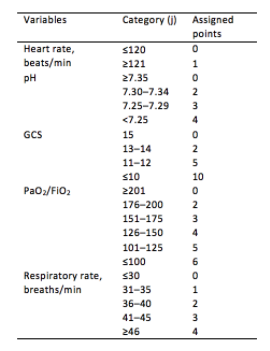
Initial development/validation: Score > 5 after 1 hour of NIV corresponds to >80% risk of NIV failure4
Earlier intubation (before 12 hours) in these patients = better survival
External validation: Score > 8 after 1 hour of NIV most predictive of eventual NIV failure 5
Average score @ 1-hour of patients with NIV success = 3.8
Score remained predictive at 6, 12, 24, 48 hours as well & mortality worsened as delay to intubation time increased
Baseline, pre-NIV score not predictive
Better predictive agreement in pneumonia and ARDS
Bottom Line:
Patients on NIV require close reassessment to prevent worsened survival due to intubation delay should invasive mechanical ventilation be indicated.
A HACOR score >8 after 1 hour of NIV should prompt intubation in most instances, with strong consideration given to a score >5.
*Note: ABGs were obtained for PaO2 assessment in the above studies -- the use of SpO2 was not evaluated -- but we are often not obtaining ABGs in our ED patients with acute respiratory failure. The following chart provides an estimated SpO2 to PaO2 conversion.
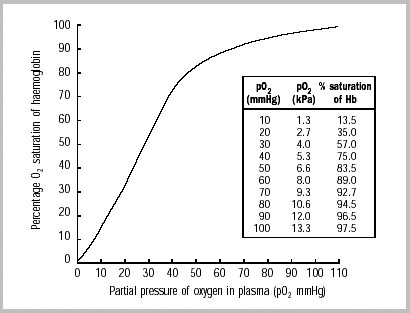
WHO 2001
Caveats:
Category: Pediatrics
Keywords: Congestive heart failure, trouble breathing, basic natriuretic peptide (PubMed Search)
Posted: 2/19/2021 by Jenny Guyther, MD
(Updated: 2/2/2026)
Click here to contact Jenny Guyther, MD
In children with known congenital heart disease, BNP measurements are higher in those patients with heart failure compared to those without heart failure.
The utility of BNP in differentiating a cardiac from pulmonary pathology in patients with respiratory distress has been studied in pediatrics. In one study involving 49 infants with respiratory distress, the patients with a final diagnosis of heart failure had a higher mean BNP concentration than those patients with other causes. Also, there is a suggestion that the relative change in NT proBNP levels may be useful in patients with underlying pulmonary hypertension. However, currently there is not enough literature to support the routine use of BNP or NT proBNP in acute management.
Bottom line: BNP can be useful in your patient with congenital heart disease who is decompensating and may be used in a patient where there is difficulty in differentiating a primary respiratory from cardiac etiology.
Davis GK, Bamforth F, Sarpal A, et al. B-type natriuretic peptide in pediatrics. Clin Biochem. 2006 Jun;39(6):600-5.
Nir A, Lindinger A, Rauh M, et al. NT-pro-B-type natriuretic peptide in infants and children: reference values based on combined data from four studies. Pediatr Cardiol. 2009 Jan;30(1):3-8.
Ten Kate CA, Tibboel D, Kraemer US. B-type natriuretic peptide as a parameter for pulmonary hypertension in children. A systematic review. Eur J Pediatr. 2015 Oct;174(10):1267-75.
Category: Toxicology
Keywords: Haloperidol, ondansetron, cannabis hyperemesis syndrome (PubMed Search)
Posted: 2/18/2021 by Hong Kim, MD
Click here to contact Hong Kim, MD
Patients with cannabis hyperemesis syndrome experience recurrent/protracted nausea/vomiting. Cases of cannabis hyperemesis syndrome may increase as cannabis use becomes more common in the United States.
A randomized control trial (triple-blind) was conducted to compare haloperidol (0.05 or 0.1 mg/kg) IV or ondansetron 8 mg IV. Primary outcome was reduction of abdominal pain and nausea from baseline (on a 10 cm visual analog scale) 2 hours after treatment.
Results
Conclusion
Ruberto AJ. et al. Intravenous haloperidol versus ondansetron for cannabis hyperemesis syndrome (HaVOC): a randomized controlled trial. Annals of Emergency Medicine. Nov 2020
https://doi.org/10.1016/j.annemergmed.2020.08.021
Category: Orthopedics
Keywords: diabetes, exercise, weight loss (PubMed Search)
Posted: 2/13/2021 by Brian Corwell, MD
(Updated: 2/2/2026)
Click here to contact Brian Corwell, MD
What time of day is best for exercise to achieve weight loss goals?
Working out in the morning has traditionally held the edge, especially if done on an empty stomach.
Upon walking, elevated levels of cortisol and GH will aid in fat metabolism.
Switching to a morning workout may also decrease appetite throughout the day.
Morning exercise may also induce significant circadian phase?shifting effects. Patients report feeling more alert in the morning and get more tired at night. This may “force” people to get increased rest as poor sleep quality and duration has been associated with weight gain.
Moderate intensity aerobic exercise has been shown to cause immediate mood improvement and mental productivity. These effects can last up to 12 hours and may be a simple aid to combat job stress.
However, a recent small study looked at this question with a group of men at high risk for Type 2 diabetes.
Those that exercised in the morning had better blood sugar control and lost more abdominal fat than those who exercised in the morning.
Study: 32 adult males (58 ± 7 years) at risk for or diagnosed with type 2 diabetes performed 12 weeks of supervised exercise training either:
In the morning (8.00–10.00 a.m., N = 12) OR
In the afternoon (3.00–6.00 p.m., N = 20)
Test: Graded cycling test with ECG monitoring until exhaustion
Results: Compared to those who trained in the morning, participants who trained in the afternoon experienced superior beneficial effects of exercise training on peripheral insulin sensitivity, insulin?mediated suppression of adipose tissue lipolysis, fasting plasma glucose levels, exercise performance and fat mass.
Conclusion: Metabolically compromised patients may benefit from shifting their exercise routine to the afternoon from the morning. Ultimately, any exercise is great in this population, but this study may be worth sharing to your patients.
Mancilla R, Brouwers B, Schrauwen-Hinderling VB, Hesselink MKC, Hoeks J, Schrauwen P. Exercise training elicits superior metabolic effects when performed in the afternoon compared to morning in metabolically compromised humans. Physiol Rep. 2021 Jan;8(24):e14669.
