Category: Neurology
Keywords: stroke, large vessel occlusion, basilar artery, posterior circulation, thrombectomy (PubMed Search)
Posted: 6/9/2021 by WanTsu Wendy Chang, MD
Click here to contact WanTsu Wendy Chang, MD
Bottom Line: There is no significant difference between endovascular thrombectomy and medical management for basilar artery occlusion strokes within 6 hours of symptom onset.
Category: Critical Care
Keywords: midodrine; septic shock; vasopressors; ICU LOS (PubMed Search)
Posted: 6/8/2021 by Kim Boswell, MD
Click here to contact Kim Boswell, MD
A recent pilot study was conducted in two centers (Mayo Clinic & Cleveland Clinic Affiliate) and aimed to evaluate if the administration of oral midodrine in early septic shock could decrease the use of IV vasopressors and decrease ICU and hospital length of stay (LOS). The study was a placebo-controlled, double blinded randomized trial.
This study enrolled:
The study did not find a statistical difference between the two groups in the use of vasopressors or ICU/Hospital LOS. However, there was a trend in the midodrine group which is suggestive of decreased vasopressor use and ICU/Hospital LOS.
It is Important to note the study was not powered to determine clinical significance. Overall the trend noted in the midodrine group should encourage further studies that are clinically powered to determine if there is a statistical difference and therefore a potential benefit to early initiation of oral midodrine in septic shock.
Lal, A, Trivedi, V, Rizvi, MS, et al. Oral Midodrine Administration During the First 24 Hours of Sepsis to Reduce the Need of Vasoactive Agents: Placebo-Controlled Feasibility Clinical Trial, Critical Care Explorations: May 2021 - Volume 3 - Issue 5 - p e0382
doi: 10.1097/CCE.0000000000000382
Category: Pharmacology & Therapeutics
Keywords: vancomycin, allergies (PubMed Search)
Posted: 6/5/2021 by Ashley Martinelli
(Updated: 2/2/2026)
Click here to contact Ashley Martinelli
Vancomycin infusion reactions can manifest as pruritus and an erythematous rash of the neck, face, and torso during or after a vancomycin infusion. This is a histamine reaction caused by degranulation of mast cells and basophils, and can be caused short infusion times <60 min. It is commonly treated with antihistamines and/or a slowing of the infusion rate.
Category: Critical Care
Keywords: Pressors, Vasopressin, Sepsis, Septic Shock (PubMed Search)
Posted: 5/31/2021 by Mark Sutherland, MD
Click here to contact Mark Sutherland, MD
Norepinephrine is widely considered the first-line vasopressor for patients in septic shock. Vasopressin is often added to norepinephrine in patients requiring escalating doses, but when to add vasopressin, and what exactly the benefit is (as opposed to just further titrating up the norepinephrine) remain unclear. Given the limited evidence for a patient-oriented benefit and the increasing cost of vasopressin, some centers are becoming more judicious in the use of vasopressin. A systematic review in AJEM October 2021 examined the literature on early (< 6 hours of diagnosis) addition of vasopressin to the management of septic shock patients, compared to either no vasopressin or starting it after 6 hours.
Improved with early vasopressin: Need for renal replacement therapy (RRT; secondary outcome)
No difference: mortality, ICU length of stay, hospital length of stay, new onset arrhythmias
Bottom Line: When, and if, to start vasopressin in patients requiring escalating doses of norepinephrine remains controversial. Based on the prior VASST trial, many providers will start vasopressin when norepi doses reach ~ 5-15 mcg/min (approx 0.1-0.2 mcg/kg/min), but there remains limited data to support this practice, and either starting vasopressin or continuing to titrate the norepinephrine as needed are both reasonable approaches in most patients.
1) Huang H, Wu C, Shen Q, Xu H, Fang Y, Mao W. The effect of early vasopressin use on patients with septic shock: A systematic review and meta-analysis. Am J Emerg Med. 2021 May 6;48:203-208. doi: 10.1016/j.ajem.2021.05.007. Epub ahead of print. PMID: 33975132.
2) Russell JA, Walley KR, Singer J, Gordon AC, Hébert PC, Cooper DJ, Holmes CL, Mehta S, Granton JT, Storms MM, Cook DJ, Presneill JJ, Ayers D; VASST Investigators. Vasopressin versus norepinephrine infusion in patients with septic shock. N Engl J Med. 2008 Feb 28;358(9):877-87. doi: 10.1056/NEJMoa067373. PMID: 18305265.
3) Lam SW, Barreto EF, Scott R, Kashani KB, Khanna AK, Bauer SR. Cost-effectiveness of second-line vasopressors for the treatment of septic shock. J Crit Care. 2020 Feb;55:48-55. doi: 10.1016/j.jcrc.2019.10.005. Epub 2019 Oct 23. PMID: 31706118.
Category: Toxicology
Keywords: NAC, gluthathione, acetaminophen toxicity (PubMed Search)
Posted: 5/27/2021 by Hong Kim, MD
Click here to contact Hong Kim, MD
What is the mechanism of action of N-acetylcysteine that is used to treat acetaminophen induced liver injury/toxicity?
Excess production of NAPQI via CYP 2E1 from acetaminophen overdose depletes gluthathione, which detoxifies NAPQI. Gluthathione consists of 3 amino acids: glutamate, cysteine and glycine. cysteine availability is the rate limiting step in gluthathione synthesis. hepatotoxicity occurs when gluthathione store is depleted below 30% of the baseline.
Thus NAC works by:
Goldfrank's Toxicologic Emergencies. Ch35 Acetaminophen A3: antidote in depth - N-acetylcysteine
Category: Critical Care
Posted: 5/25/2021 by Mike Winters, MBA, MD
Click here to contact Mike Winters, MBA, MD
Refractory Anaphylaxis
Krishnaswamy G. Critical care management of anaphylaxis: A conside definitive review. Crit Care Med. 2021.
Category: Pediatrics
Keywords: pediatric, cardiac arrest, metabolic acidosis, sodium bicarbonate (PubMed Search)
Posted: 5/21/2021 by Jenny Guyther, MD
(Updated: 2/2/2026)
Click here to contact Jenny Guyther, MD
During cardiac arrest, metabolic acidosis develops because of hypoxia-induced anaerobic metabolism and decreased acid excretion caused by inadequate renal perfusion. Sodium bicarbonate (SB) administration was considered as a buffer therapy to correct metabolic acidosis. However, SB has several side effects such as hypernatremia, metabolic alkalosis, hypocalcemia, hypercapnia, impairment of tissue oxygenation, intracellular acidosis, hyperosmolarity, and increased lactate production. The 2010 Pediatric Advanced Life Support (PALS) guideline stated that routine administration of SB was not recommended for cardiac arrest except in special resuscitation situations, such as hyperkalemia or certain toxidromes. An evidence update was conducted in the 2020 Pediatric Life Support (PLS) guideline and the recommendations of 2010 remain valid. This article was a systematic review and meta-analysis of observational studies of pediatric in hospital cardiac arrests. The primary outcome was the rate of survival to hospital discharge after in hospital cardiac arrests. The secondary outcomes were the 24-hour survival rate and neurological outcomes.
Chih-Yao Chang, Po-Han Wu, Cheng-Ting Hsiao, Chia-Peng Chang, Yi-Chuan Chen, Kai-Hsiang Wu. Sodium bicarbonate administration during in-hospital pediatric cardiac arrest: a systematic review and meta-analysis. Resuscitation. 2021. Available on line March 1. In Press.
Category: Neurology
Keywords: Lumbar puncture, LP, post-dural, headache, intracranial hypotension (PubMed Search)
Posted: 5/12/2021 by WanTsu Wendy Chang, MD
(Updated: 2/2/2026)
Click here to contact WanTsu Wendy Chang, MD
Bottom Line: The use of atraumatic needles is most effective in reducing the risk of post-LP headaches. These needles are easy to use and have similar rate of success as cutting needles.
Cognat E, Koehl B, Lilamand M, et al. Preventing post-lumbar puncture headache. Ann Emerg Med. 2021 May 6;S0196-0644(21)00151-7. Online ahead of print.
Follow me on Twitter @EM_NCC
Category: Critical Care
Keywords: COVID-19, tocilizumab, ICU, mechanical ventilation (PubMed Search)
Posted: 5/11/2021 by Lindsay Ritter, MD
(Updated: 2/2/2026)
Click here to contact Lindsay Ritter, MD
RECAP: RECOVERY trial is a large, randomized, open label, adaptive trial studying different treatments on COVID-19. Most well known is the use of dexamethasone which reduced mortality by 1/3 in COVID patients requiring mechanical ventilation and by 1/5 in those requiring oxygen, with no benefit on those patients not requiring oxygen.
They recently published results in the Lancet on the use of tocilizumab.
Population:
Inclusion:
Outcomes:
Results:
Conclusion:
RECOVERY Collaborative Group Tocilizumab in patients admitted to hospital with COVID-19 (RECOVERY): a randomised, controlled, open-label, platform trial. Lancet. 2021; 397: 1637-1645
Category: Orthopedics
Keywords: Epidural abscess, back pain, vertebral osteomyelitis (PubMed Search)
Posted: 5/8/2021 by Brian Corwell, MD
Click here to contact Brian Corwell, MD
Both erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP) are highly sensitive (84-100%) for spinal infections and are observed in >80% with vertebral osteomyelitis and epidural abscesses.
ESR
Most sensitive and specific serum marker, usually elevated in both spinal epidural abscess (SEA) and vertebral osteomyelitis.
ESR was elevated in 94-100% of patients with SEA vs. only 33% of non-SEA patients
Mean ESR in patients with SEA was significantly elevated (51-77mm/hour)
CRP
Not highly specific
Less useful for acute diagnosis since CRP levels rise faster and return to baseline faster than ESR (elevated CRP seen in 87% of patients with SEA as well as in 50% of patients with spine pain not due to a SEA)
Better used as a marker of response to treatment.
1) Colip CG, Lotfi M, Buch K, Holalkere N, Setty BN. Emergent spinal MRI in IVDU patients presenting with back pain: do we need an MRI in every case? Emerg Radiol 2018;25:247-56.
2) Davis DP, Salazar A, Chan TC, Vilke GM. Prospective evaluation of a clinical decision guideline to diagnose spinal epidural abscess in patients who present to the emergency department with spine pain. J Neurosurg Spine 2011;14:765-70.
Category: Critical Care
Keywords: cardiac arrest, massive pulmonary embolism, Venoarterial, ECMO (PubMed Search)
Posted: 5/4/2021 by Quincy Tran, MD, PhD
(Updated: 2/2/2026)
Click here to contact Quincy Tran, MD, PhD
Background:
Cardiac arrest from massive pulmonary embolism (PE) can be up to 90% (1). A recent systemic review evaluated the efficacy of Venoarterial-Extracorporeal Membrane Oxygenation (VA-ECMO) for PE-related cardiac arrest.
Results:
The authors screened 1115 articles and included 77 articles, including gray literature. The authors performed a quantitative analysis of a total of 301 patients.
Overall, 183/301 (61%) patients survived to hospital discharge, a significant improvement from 90%.
Patients who were cannulated during chest compression were associated with 7x higher odds of death (OR, 6.84; 95% CI, 1.53–30.58; p = 0.01), compared to those who were cannulated after ROSC. However, cannulation in the ED was not associated with improved outcomes, compared with other cannulation site.
No increased risk of death among patients who received tPA prior to VA-ECMO vs. those who did not (OR, 0.78; 95% CI, 0.39–1.54; p = 0.48).
Patients whose age > 65 years of age were associated with 3X risk of death, compared to those with age < 65 years (OR, 3.56; 95% CI, 1.29–9.87; p = 0.02).
Take-home points
Please consider “early” VA-ECMO for eligible patients who have cardiac arrest from massive PE. However, it will take great convincing to push the PERT team to cannulate for VA-ECMO while the patient is still receiving chest compression.
1.Lavonas EJ, Drennan IR, Gabrielli A, et al: Part 10: Special circumstances of resuscitation: 2015 American Heart Association guidelines update for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation 2015; 132:S501–S518.
2. Scott JH, Gordon M, Vender R, Pettigrew S, Desai P, Marchetti N, Mamary AJ, Panaro J, Cohen G, Bashir R, Lakhter V, Roth S, Zhao H, Toyoda Y, Criner G, Moores L, Rali P. Venoarterial Extracorporeal Membrane Oxygenation in Massive Pulmonary Embolism-Related Cardiac Arrest: A Systematic Review. Crit Care Med. 2021 May 1;49(5):760-769. doi: 10.1097/CCM.0000000000004828. PMID: 33590996.
Category: Critical Care
Keywords: cardiac arrest, massive pulmonary embolism, Venoarterial, ECMO (PubMed Search)
Posted: 5/4/2021 by Quincy Tran, MD, PhD
Click here to contact Quincy Tran, MD, PhD
Background:
Cardiac arrest from massive pulmonary embolism (PE) can be up to 90% (1). A recent systemic review evaluated the efficacy of Venoarterial-Extracorporeal Membrane Oxygenation (VA-ECMO) for PE-related cardiac arrest.
Results:
The authors screened 1115 articles and included 77 articles, including gray literature. The authors performed a quantitative analysis of a total of 301 patients.
Overall, 183/301 (61%) patients survived to hospital discharge, a significant improvement from 90%.
Patients who were cannulated during chest compression were associated with 7x higher odds of death (OR, 6.84; 95% CI, 1.53–30.58; p = 0.01), compared to those who were cannulated after ROSC. However, cannulation in the ED was not associated with improved outcomes, compared with other cannulation sites.
No increased risk of death among patients who received tPA prior to VA-ECMO vs. those who did not (OR, 0.78; 95% CI, 0.39–1.54; p = 0.48).
Patients whose age > 65 years of age were associated with 3X risk of death, compared to those with age < 65 years (OR, 3.56; 95% CI, 1.29–9.87; p = 0.02).
Take-home points
Please consider “early” VA-ECMO for eligible patients who have cardiac arrest from massive PE. However, it will take great convincing to push the PERT team to cannulate for VA-ECMO while the patient is still receiving chest compression.
1.Lavonas EJ, Drennan IR, Gabrielli A, et al: Part 10: Special circumstances of resuscitation: 2015 American Heart Association guidelines update for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation 2015; 132:S501–S518.
2. Scott JH, Gordon M, Vender R, Pettigrew S, Desai P, Marchetti N, Mamary AJ, Panaro J, Cohen G, Bashir R, Lakhter V, Roth S, Zhao H, Toyoda Y, Criner G, Moores L, Rali P. Venoarterial Extracorporeal Membrane Oxygenation in Massive Pulmonary Embolism-Related Cardiac Arrest: A Systematic Review. Crit Care Med. 2021 May 1;49(5):760-769. doi: 10.1097/CCM.0000000000004828. PMID: 33590996
Category: Pediatrics
Posted: 4/30/2021 by Rose Chasm, MD
(Updated: 2/2/2026)
Click here to contact Rose Chasm, MD
Layden, JE, et al. Pulmonary Illness Related to E-Cigarette Use in Illinois and Wisconsin. New England Journal of Medicine. September 2019.
Centers for Disease Control. Smoking and Tobacco Use. Office of Smoking and Health, National Center for Chronic Disease Prevention and Health Promotion. April 2021.
Category: Neurology
Keywords: functional neurological disorder, FND, stroke mimic, non-epileptic seizure (PubMed Search)
Posted: 4/28/2021 by WanTsu Wendy Chang, MD
Click here to contact WanTsu Wendy Chang, MD
Bottom Line: Functional neurological disorders (FND) are commonly encountered in the ED. A thorough neurological exam may reveal positive signs suggestive of FND. Early diagnosis and referral to specialists may improve outcomes.
Finkelstein SA, Cortel-LeBlanc MA, Cortel-LeBlanc A, Stone J. Functional neurological disorder in the emergency department. Acad Emerg Med. 2021 Apr 18 [Online ahead of print]
Follow me on Twitter @EM_NCC
Category: Orthopedics
Keywords: SEA, ESR, spinal infection (PubMed Search)
Posted: 4/24/2021 by Brian Corwell, MD
Click here to contact Brian Corwell, MD
Erythrocyte sedimentation rate (ESR) for spinal infection
Sensitive for spinal infection but not specific
Elevated ESR is observed in greater than 80% of patients with vertebral osteomyelitis and epidural abscess
ESR is the most sensitive and specific serum marker for spinal infection
Usually elevated in acute presentations of SEA and vertebral osteomyelitis
ESR was elevated in 94-100% of patients with SEA vs. only 33% of non-SEA patients
Mean ESR in patients with SEA was significantly elevated (51-77mm/hour)
Infection is unlikely in patients with an ESR less than 20 mm/h.
Incorporating ESR into an ED decision guideline may improve diagnostic delays and help distinguish patients in whom MRI may be performed on a non-emergent basis
1) Davis DP, et al. Prospective evaluation of a clinical decision guideline to diagnose spinal epidural abscess in patients who present to the emergency department with spine pain. J Neurosurg Spine 2011;14:765-767.
2) Reihsaus E, et al. Spinal epidural abscess: a meta-analysis of 915 patients. Neurosurg Rev 2000;23:175,204
Category: Critical Care
Keywords: COPD, emphysema, acute respiratory failure, hypoxia, oxygen saturation (PubMed Search)
Posted: 4/20/2021 by Kami Windsor, MD
Click here to contact Kami Windsor, MD
Supplemental oxygen therapy is frequently required for patients presenting with acute respiratory distress and COPD exacerbation. Over-oxygenation can derail compensatory physiologic responses to hypoxia,1 resulting in worsening VQ mismatch and, to a lesser degree, decreases in minute ventilation, that cause worsened respiratory failure.
The 2012 DECAF (Dyspnea, Eosinopenia, Consolidation, Acidaemia, and Atrial Fibrillation) score was found to predict risk of in-hospital mortality in patients admitted with acute COPD exacerbation.2,3 Data from the DECAF study’s derivation and external validation cohorts were examined specifically to look at outcome associated with varying levels of oxygen saturation.
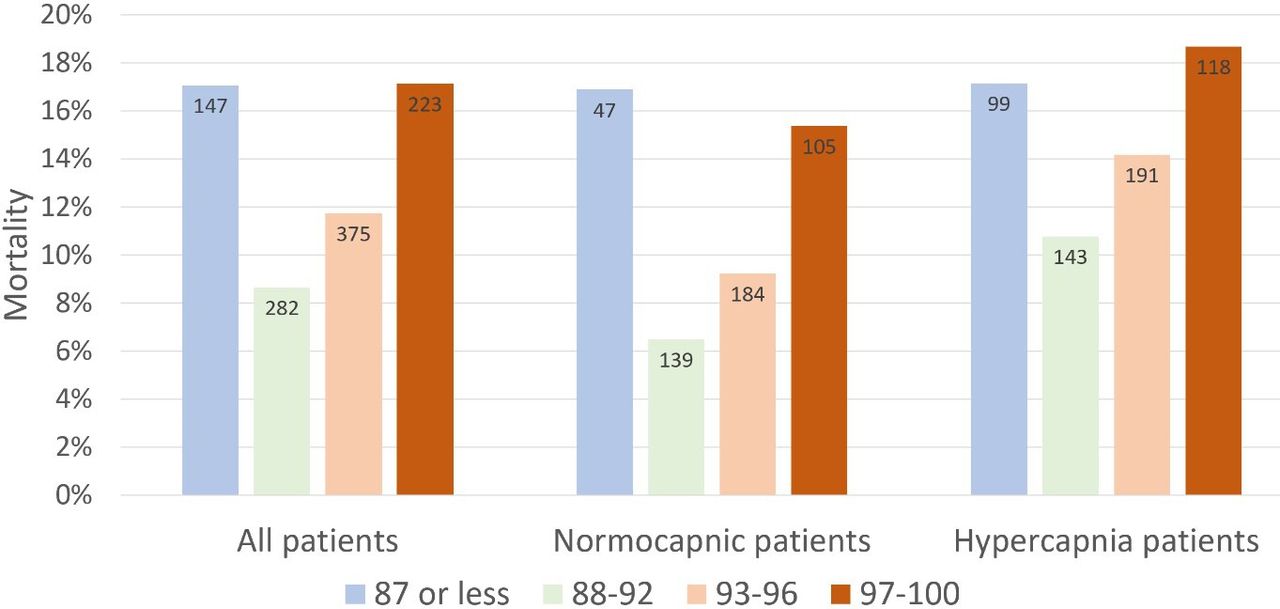
Bottom Line
In patients presenting to the ED with acute COPD exacerbation requiring oxygen supplementation, a target oxygen saturation of 88-92% is associated with the lowest in-hospital mortality, and higher oxygen saturations should be avoided independent of patients' PCO2 levels.
Category: Pediatrics
Keywords: stroke, altered mental status, TPA (PubMed Search)
Posted: 4/16/2021 by Jenny Guyther, MD
(Updated: 2/2/2026)
Click here to contact Jenny Guyther, MD
Baldovsky MD, Okada PJ. Pediatric stroke in the emergency department. J Am Coll Emerg Physicians Open. 2020 Oct 6;1(6):1578-1586. doi: 10.1002/emp2.12275. PMID: 33392566; PMCID: PMC7771757.
Category: Neurology
Keywords: acute ischemic stroke, alteplase, tPA, thrombolysis, error (PubMed Search)
Posted: 4/15/2021 by WanTsu Wendy Chang, MD
Click here to contact WanTsu Wendy Chang, MD
Bottom Line: Alteplase administration in acute ischemic stroke is associated with errors, most commonly with over-dosage of the medication.
Dancsecs KA, Nestor M, Bailey A, Hess E, Metts E, Cook AM. Identifying errors and safety considerations in patients undergoing thrombolysis for acute ischemic stroke. Am J Emerg Med. 2021;47:90-94.
Follow me on Twitter @EM_NCC
Category: Orthopedics
Keywords: Concussion, mTBI, exercise prescription (PubMed Search)
Posted: 4/10/2021 by Brian Corwell, MD
(Updated: 2/2/2026)
Click here to contact Brian Corwell, MD
A total of 367 patients were enrolled. Median age was 32 years Male 43%/Female 57%.
Result: There was no difference in the proportion of patients with postconcussion symptoms at 30 days. There were no differences in median change of concussion testing scores, median number of return PCP visits, median number of missed school or work days, or unplanned return ED visits within 30 days. Participants in the control group reported fewer minutes of light exercise at 7 days (30 vs 35).
Conclusion
Prescribing light exercise for acute mTBI, demonstrated no differences in recovery or health care utilization outcomes.
Extrapolating from studies in the athletic population, there may be a patient benefit for light exercise prescription.
Make sure that the patient is only exercising to their symptomatic threshold as we recommend with concussed athletes. Previous studies have shown that athletes with the highest post injury activity levels had poorer visual memory and reaction time scores than those with moderate activity levels.
Varner et al. A randomized trial comparing prescribed light exercise to standard management for emergency department patients with acute mild traumatic brain injury. Acad Emerg Med. 2021.
Category: Toxicology
Keywords: household spices, abuse, toxicity (PubMed Search)
Posted: 4/8/2021 by Hong Kim, MD
(Updated: 2/2/2026)
Click here to contact Hong Kim, MD
There are three commonly household spices that can be abuse/misused or cause toxicity after exposure.
Pure vanilla extract contains at least 35% ethanol by volume per US Food and Drug Administration standards
Nutmeg contains myristicin – serotonergic agonist that possess psychomimetic properties.
Clinical effects:
Cinnamon contains cinnamaldehyde and eugenol – local irritants.
Johnson-Arbor K et al. Stoned on spices: a mini-review of three commonly abuse housenold spices. Clin Toxicol (Phila) 2020
https://doi.org/10.1080/15563650.2020.1840579
