Category: Toxicology
Keywords: chloroquine, hydroxychloroquine (PubMed Search)
Posted: 3/26/2020 by Hong Kim, MD
Click here to contact Hong Kim, MD
COVID-19 pandemic has brought two old medications – chloroquine and Hydroxychloroquine – back from the past.
A couple in Arizona self-medicated with chloroquine this week and experienced chloroquine toxicity; the man died and his wife was admitted to the ICU.
https://www.cnn.com/2020/03/23/health/arizona-coronavirus-chloroquine-death/index.html
Chloroquine and hydroxychloroquine overdose result in cardiotoxicity by Na and K channel blockade (similar to other membrane stabilizing agents such as TCAs, loperamide, etc.). Onset of toxicity is usually within 1 – 3 hours after ingestion.
Other symptoms of toxicity include: nausea/vomiting, respiratory depression/apnea, altered mental status and seizure. Hypokalemia is often encountered.
Use of sodium bicarbonate is controversial due to worsening of hypokalemia. Instead, administration of high dose diazepam and epinephrine (EPI) infusion has shown to decrease mortality (see below).
Riou B et al. NEJM 1988 DOI: 10.1056/NEJM198801073180101
Survival:
Clemessy JL et al. Crit Care Med 1996. DOI:10.1097/00003246-199607000-00021
Treatment: 87% received at least one of the interventions below.
Mortality
Bottom line
Category: Neurology
Keywords: Coronavirus, SARS, SARS-CoV, COVID-19, SARS-CoV-2 (PubMed Search)
Posted: 3/25/2020 by WanTsu Wendy Chang, MD
(Updated: 2/2/2026)
Click here to contact WanTsu Wendy Chang, MD
Bottom Line: SARS-CoV has been associated with CNS involvement. Given their similar pathogenesis and finding of hyposmia in COVID-19, SARS-CoV-2 may be associated with risk of CNS involvement.
Follow me on Twitter @EM_NCC
Category: Critical Care
Keywords: COVID-19 (PubMed Search)
Posted: 3/24/2020 by Mark Sutherland, MD
Click here to contact Mark Sutherland, MD
Within the past few days we completed a review of complications of COVID-19, to describe what sequelae and clinical patterns, besides the obvious (URI, respiratory failure, ARDS, sepsis, etc), are noted in the literature. This review, along with a plethora of other information focusing on critical care of the COVID-19 patient, will be posted in the next few days to http://covid19.ccproject.com/. Below are the key points from that review:
Acute cardiovascular complications appear to be the most common and concerning sequelae:
-Acute myocardial injury (7-17% of hospitalized patients in one study),
-Myocarditis (primary cause of death in 7% of COVID deaths in one study),
-Arrhythmias (16.7% of hospitalized and 44.4% of ICU patients in one study),
-Venous thromboembolism (incidence unknown).
Concerns for sudden cardiac death, even after recovery, have been raised but are not well documented in the literature. Proposed mechanisms include respiratory compromise, myocarditis, malignant tachydysrhythmias, heart failure, and coronary plaque instability (i.e. Type 1 MI) secondary to inflammation
Co-infection and secondary infection rates are unknown but estimates range from 4.8% to 21%, with higher rates in sicker patients. Viral co-infection is more common than bacterial co-infection, but both may be seen. The ability to rule out COVID-19 by a positive multiplex respiratory viral panel is questionable.
Cytokine release syndrome and secondary HLH are both described complications, but their incidence is unknown. The relation of this finding to purported benefits of tocilizumab (which is also a therapy for HLH) is unknown.
Other extrapulmonary complications are relatively typical of sepsis, such as kidney injury, abnormal LFTs, and delirium
If anyone would like a copy of the full document, which details known complications by organ system, please feel free to email me at msutherland@som.umaryland.edu. Thanks to David Gordon for organizing the project.
Everyone stay safe, and be sure to take care of each other, as well as our patients.
Category: Pediatrics
Keywords: pandemic, coronavirus, pediatric (PubMed Search)
Posted: 3/20/2020 by Jenny Guyther, MD
(Updated: 2/2/2026)
Click here to contact Jenny Guyther, MD
Category: Toxicology
Keywords: acetaminophen overdose, methemoglobinemia (PubMed Search)
Posted: 3/19/2020 by Hong Kim, MD
Click here to contact Hong Kim, MD
Methemoglobinemia occurs when iron in the hemoglobin is converted from ferrous (2+) to ferric (3+) state, frequently by substance exposure. There are many medications and chemicals that can induce methemoglobinemia.
Common agents that induce methemoglobinemia include:
Acetaminophen has not been associated with methemoglobinemia. However, two cases of methemoglobinemia in massive acetaminophen overdose were recently reported. Both patients were not on any medication known to cause methemoglobinemia.
Case 1: 54 year-old man with DM, HTN, cognitive impairment and no hx of G6PD deficiency hospitalized for altered mental status
Case 2: 64 year-old man with dementia, polysubstance abuse, depression and hypertension hospitalized from nursing home for altered mental status.
Conclusion
Rainprakaisang T. et al. Methemoglobinemia assoicated with massive acetaminophen ingestion: a case series. Clin Toxicolo (Phila). 2019.
https://doi.org/10.1080/15563650.2019.1657883
Category: Critical Care
Keywords: ARDS COVID19 (PubMed Search)
Posted: 3/17/2020 by Robert Brown, MD
(Updated: 2/2/2026)
Click here to contact Robert Brown, MD
This week we anticipate treating more COVID19 cases as they progress to ARDS. The World Health Organization issued guidelines on 3/13/20 for treating Severe Acute Respiratory Infection (SARI) due to COVID19.
How to identify ARDS?
No different than before COVID. Order a CXR, ABG, and perform bedside ultrasound evaluation of cardiac function and volume status. If there are bilateral opacifications you cannot explain entirely with volume overload, nodules, or lobar collapse, AND if the ratio of PaO2/FiO2 is < 300 (mild), < 200 (moderate), or < 100 (severe), then treat for ARDS.
***While you are waiting for your blood gas, SpO2/FiO2 <315 suggests ARDS.
What is the oxygen goal?
During resuscitation: > 93%
Once stabilized: > 89%
What is the expected clinical course?
Patients experience RAPID deterioration to respiratory failure. You should expect to intubate. This should be performed with N95 protection and should be done by the person with greatest first pass success.
Be CONSERVATIVE with fluids. Do not give a 30mL/kg bolus. Give 250-500mL bolus and re-evaluate. Excess fluid results in prolonged hypoxia and mechanical ventilation.
Should empiric treatments change?
No. Co-infection with influenza, bacterial pneumonia, and all other pathogens is possible, so you should continue to cover all suspected pathogens and de-escalate as microbiology labs result.
Should ventilator settings change?
No. Use lung protective volumes and permissive hypercapnia. The volume is based on the patient's height, not weight. A quick way to do this? Measure the height in cm. Subtract 100 for a man and subtract 110 for a woman and this is the ideal body weight. Provide 6mL/kg of tidal volume with a goal plateau pressure < 30. Use the high PEEP strategy from the ARDSnet trial and even consider clamping the ET tube when transitioning from machine to bag for transport in order to preserve PEEP.
Do patients benefit from proning?
Yes. 12-16 hours/day for severe ARDS. Not true in pregnancy as a whole, though early pregnancy may still benefit.
Is ECMO beneficial in refractory cases?
Unknown. In the case of MERS-CoV, ECMO reduced mortality.
Are corrticosteroids useful?
No. Do not administer steroids routinely to these patients. You may give steroids where indicated, including cases of refractory shock following pressors.
Clinical Management of Severe Acute Respiratory Infection (SARI) when COVID 19 disease is suspected: interim guidance, 13 March 2020
Arabi YM, Arifi AA, Balkhy HH, Najm H, Aldawood AS, Ghabashi A et al. Clinical course and outcomes of critically ill patients with Middle East respiratory syndrome coronavirus infection. Ann Intern Med. 2014;160(6):38997.
Category: Airway Management
Keywords: Epidural abscess, back pain (PubMed Search)
Posted: 3/14/2020 by Brian Corwell, MD
(Updated: 2/2/2026)
Click here to contact Brian Corwell, MD
Laboratory studies are not often indicated in the early evaluation of low back pain.
Complete blood counts (CBC) have poor sensitivity and specificity for infection. White blood cell (WBC) counts, have poor sensitivity and specificity for infection. They may be elevated and a left shift or bandemia may be present and increase suspicion for infection, but a lack of these does not rule out infection. Elevated WBC counts are only found in two-thirds of patients with SEA.
Both erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP) are highly sensitive (84-100%) for spinal infections and are observed in >80% with vertebral osteomyelitis and epidural abscesses. However, elevated CRP was found in 87% of patients with an epidural abscess as well as half of patients with spine pain not due to an epidural abscess, so is not highly specific.
CRP levels rise rapidly and decrease rapidly with improvement in disease and may be better used to follow response to treatment. ESR is the most sensitive and specific serum marker of infection. ESR is elevated in 94-100% of patients with an epidural abscess compared to only 33% of those without an epidural abscess. Infection is unlikely in patients with an ESR less than 20 mm/h. Although an elevated ESR (>20 mm/h) is the most specific serum test for infection, it also may indicate occult malignancy (sensitivity, 78%; specificity, 67%).
If infection is suspected, obtain two sets of blood cultures, as a causative pathogen may be identified in ~50% of patients.
Category: Critical Care
Posted: 3/10/2020 by Caleb Chan, MD
(Updated: 2/2/2026)
Click here to contact Caleb Chan, MD
(*It is important to note that many of the percentages in these early studies will change as more asymptomatic or minimally symptomatic patients are identified with increased testing)
Epidemiology
Among more than 44,000 confirmed cases of COVID-19 in China as of Feb 11, 2020:
- 30–69 years: ~78%
- severely or critically ill: ~19%
Case-fatality proportion:
-60-69 years: 3.6%
-70-79 years: 8%
-≥80 years: 14.8%.
-With no underlying medical conditions: overall case fatality of 0.9%
-With comorbidities:
-cardiovascular disease (10.5%), diabetes (7%)
-chronic respiratory disease, hypertension, and cancer (6% each)
Presentation
For patients admitted to the hospital, many non-specific signs and symptoms:
- fever (77–98%) and cough (46%–82%) were most common
- of note, gastrointestinal symptoms (~10%) such as diarrhea and nausea present prior to developing fever and lower respiratory tract signs and symptoms.
Diagnosis
No general lab tests have great sensitivity or specificity
A normal CT scan does NOT rule out COVID-19 infection
-In an early study, 20/36 (56%) of patients imaged 0-2 days (‘early’) after symptom onset had a normal CT with complete absence of ground-glass opacities and consolidation
Treatment-
Mainstay of treatment will be management of hypoxemia including early intubation if necessary. However, specifically:
-Steroid therapy is controversial and the WHO is currently recommending against it unless it is being administered for another reason
-has not been associated with any benefit
-associated with possible harm in previous smaller studies with SARS and MERS
-associated with prolonged viremia
-intravenous remdesivir (a nucleotide analogue prodrug with promising in-vitro results against SARS-CoV and MERS-CoV) is available for compassionate use
-lopinavir-ritonavir has been used without any associated benefit
Al-tawfiq JA, Al-homoud AH, Memish ZA. Remdesivir as a possible therapeutic option for the COVID-19. Travel Med Infect Dis. 2020;:101615.
Bernheim A, Mei X, Huang M, et al. Chest CT Findings in Coronavirus Disease-19 (COVID-19): Relationship to Duration of Infection. Radiology. 2020;:200463.
Holshue ML, Debolt C, Lindquist S, et al. First Case of 2019 Novel Coronavirus in the United States. N Engl J Med. 2020;
Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;
Russell CD, Millar JE, Baillie JK. Clinical evidence does not support corticosteroid treatment for 2019-nCoV lung injury. Lancet. 2020;395(10223):473-475.
Wu Z, Mcgoogan JM. Characteristics of and Important Lessons From the Coronavirus Disease 2019 (COVID-19) Outbreak in China: Summary of a Report of 72?314 Cases From the Chinese Center for Disease Control and Prevention. JAMA. 2020;
Young BE, Ong SWX, Kalimuddin S, et al. Epidemiologic Features and Clinical Course of Patients Infected With SARS-CoV-2 in Singapore. JAMA. 2020;
https://www.cdc.gov/coronavirus/2019-ncov/hcp/clinical-guidance-management-patients.html
Category: Pharmacology & Therapeutics
Keywords: Pneumonia, MRSA, Antibiotics (PubMed Search)
Posted: 3/7/2020 by Wesley Oliver
Click here to contact Wesley Oliver
Empirical Anti-MRSA vs Standard Antibiotic Therapy and Risk of 30-Day Mortality
A recent article published in JAMA Internal Medicine questioned the utility of empiric anti-MRSA pneumonia therapy. It was a retrospective multicenter cohort study conducted in the Veteran’s Health Administration healthcare system that looked at 88,605 patients with community-onset pneumonia. They compared 30-day mortality of patients hospitalized for pneumonia receiving empirical anti-MRSA therapy plus standard therapy against standard therapy alone. Secondary outcomes analyzed development of kidney injury and secondary infections with C. difficile, VRE, or gram-negative rods. They also analyzed subgroups: ICU admission, MRSA risk factors, positive MRSA surveillance test, and positive MRSA culture on admission.
Anti-MRSA Therapy: Vancomycin (98%), Linezolid (2%)
Standard Therapy: Beta-lactam + macrolide/tetracycline, or respiratory fluoroquinolone
Outcomes
Mortality: aRR=1.4 [95% CI, 1.3-1.5]
Kidney Injury: aRR=1.4 [95% CI, 1.3-1.5]
Secondary C. difficile: aRR=1.6 [95% CI, 1.3-1.9]
Secondary VRE: aRR=1.6 [95% CI, 1.0-2.3]
Secondary gram-negative rods: aRR=1.5 [95% CI, 1.2-1.8]
Mortality in Subgroups
ICU: aRR=1.3 [95% CI, 1.2-1.5]
MRSA Risk Factors*: aRR=1.2 [95% CI, 1.1-1.4]
Positive MRSA Surveillance: aRR=1.6 [95% CI, 1.3-1.9]
MRSA Detected on Culture: aRR=1.1 [95% CI, 0.8-1.4]
*MRSA Risk Factors
-History of MRSA infection/colonization within the past year
-Or 2 of the following: previous hospitalization, nursing home residence, and previous intravenous antibiotic therapy
Take-Home Point
Empirical anti-MRSA therapy did not decrease mortality for any groups of patients hospitalized for pneumonia. Given that healthcare-associated pneumonia is no longer a definition supported by the IDSA/ATS, be judicious in your use of anti-MRSA therapy in community-onset pneumonia and reserve for those patients at higher risk for MRSA, such as those with post-influenza pneumonia.
Jones BE, Ying J, Stevens V, et al. Empitical anti-MRSA vs standard antibiotic therapy and risk of 30-day mortality in patients hospitalized for pneumonia [published online ahead of print, February 17, 2020]. JAMA Intern Med. doi: 10.1001/jamainternmed.2019.7495.
Metlay JP, Waterer GW, Long AC, et al. Diagnosis and treatment of adults with community-acquired pneumonia. An official clinical practice guideline of the American Thoracic Society and Infectious Diseases Society of America. Am J Resp Crit Care. 2019;200:e45-e67.
Smith C. Is Empiric Anti-MRSA Pnumonia Therapy Harmful? https://journalfeed.org/article-a-day/2020/is-empiric-anti-mrsa-pneumonia-therapy-harmful. March 4, 2020. Accessed March 6, 2020.
Category: Critical Care
Keywords: sedation, light sedation, no sedation, mechanically ventilated patients (PubMed Search)
Posted: 2/26/2020 by Quincy Tran, MD, PhD
(Updated: 3/3/2020)
Click here to contact Quincy Tran, MD, PhD
Settings: Multicenter randomized controlled trial
Patients: 710 patients
Intervention: 345 patients. no sedative but only boluses of morphine as clinically indicated (Sedation group)
Comparison: 356 patients. light sedation with daily interruption (Nonsedation group)
Outcome: all-cause mortality at 90 days after randomization
Study Results:
42.4% of nonsedation group died vs 37% of sedation group (95% confidence interval [CI], −2.2 to 12.2; P = 0.65).
Number of ventilator-free days for nonsedation group was 27 days vs. 26 for sedation group.
Discussion:
This study did not agree with previous studies that lighter sedation was associated with shorter length of stay on mechanical ventilation , ICU or hospital. The authors attributed to the findings that RASS score was not significantly different between the 2 groups.
Conclusion:
Critically ill adult patients receiving mechanical ventilation, there was no difference in 90-day mortality between patients receiving light sedation or no sedation.
Olsen HT, Nedergaard HK, Strøm T1, Oxlund J, Wian KA, Ytrebø LM1, Kroken BA, Chew M, Korkmaz S, Lauridsen JT, Toft P.
Nonsedation or Light Sedation in Critically Ill, Mechanically Ventilated Patients.
N Engl J Med. 2020 Feb 16. doi: 10.1056/NEJMoa1906759. [Epub ahead of print]
Category: Neurology
Keywords: traumatic brain injury, antiplatelet, anticoagulation, CT, neuroimaging (PubMed Search)
Posted: 2/26/2020 by WanTsu Wendy Chang, MD
Click here to contact WanTsu Wendy Chang, MD
Bottom Line: Patients on warfarin or a combination of aspirin and clopidogrel have increased risk of significant intracranial injury after blunt head trauma. Aspirin or clopidogrel monotherapy do not appear to be risk factors.
Follow me on Twitter @EM_NCC
Category: Airway Management
Keywords: MRI, back pain (PubMed Search)
Posted: 2/22/2020 by Brian Corwell, MD
Click here to contact Brian Corwell, MD
Cauda Equina Syndrome is a medical emergency that is considered in all patients who present to the ED with lower back pain.
Clinical presentation is variable in nature and may include some combination of lower back pain, bowel or bladder dysfunction, sexual dysfunction, saddle anesthesia with motor/sensory abnormalities.
MRI is the gold standard for diagnosis
Many of us have encountered a scenario where a patient with high clinical suspicion returns with scan negative MRI.
Studies have attempted to characterize this population.
Patients in the scan negative group had an increased prevalence of functional disorders (37% vs. 9%), functional neurologic disorders (12% vs. 0%), and psychiatric comorbidities (53% vs. 20%).
Further study is needed to characterize this association.
Hospitals may consider individualized neurologic and psychiatric referral for certain patients who are scan negative in the future.
Is scan-negative cauda equina syndrome a functional neurological disorder? A pilot study. Gibson et al., Eur J Neurol 2020, Feb 19.
Is scan-negative cauda equina syndrome a functional neurological disorder? A pilot study. Gibson et al., Eur J Neurol 2020, Feb 19.
Category: Pediatrics
Keywords: cardiac arrest, prehospital, epinephrine (PubMed Search)
Posted: 2/21/2020 by Jenny Guyther, MD
(Updated: 2/2/2026)
Click here to contact Jenny Guyther, MD
Matsuyama et al. Pre-Hospital Administration of Epinephrine in Pediatric Patients with Out-of-Hospital Cardiac Arrests. JACC: 75 (2); 2020.
Category: Critical Care
Keywords: ACS, abdominal compartment syndrome, intraabdominal hypertension, emergent laparotomy (PubMed Search)
Posted: 2/18/2020 by Kami Windsor, MD
Click here to contact Kami Windsor, MD
With ED-boarding of critically-ill patients becoming more common, it is likely that ED physicians may find themselves caring for a patient who develops ACS – that is, abdominal compartment syndrome. While intraabdominal hypertension (IAH) is common and is defined as intraabdominal pressure > 12 mmHg, ACS is defined as a sustained intraabdominal pressure > 20mmHg with associated organ injury.
WHY you need to know it:
ACS → Increased mortality & recognition is key to appropriate management
WHO is at risk:
HOW it kills:
→ Lactic acidosis, respiratory acidosis, multisystem organ failure, cardiovascular collapse & death
WHEN to consider it:
WHAT to do:
Bottom Line: Abdominal compartment syndrome is an affliction of the critically ill, is assosciated with worsened mortality, and requires aggressive measures to lower the intraabdominal pressure while obtaining emergent surgical consultation for potential emergent laparotomy.
Gottlieb M, Koyfman A, Long B. Evaluation and Management of Abdominal Compartment Syndrome in the Emergency Department. J Emerg Med. 2019. https://doi.org/10.1016/j.jemermed.2019.09.046
Category: Pediatrics
Keywords: avulsion fracture, orthopedics, pelvic injury, trauma (PubMed Search)
Posted: 2/14/2020 by Mimi Lu, MD
(Updated: 2/15/2020)
Click here to contact Mimi Lu, MD
A 15 y.o. female presents to your emergency department with sudden onset hip pain after winding up to kick a soccer ball during her game today. You see a well-developed female in obvious discomfort, with tenderness to palpation over her lateral hip and pain with passive ROM at the hip. You obtain this x-ray. What is your diagnosis?
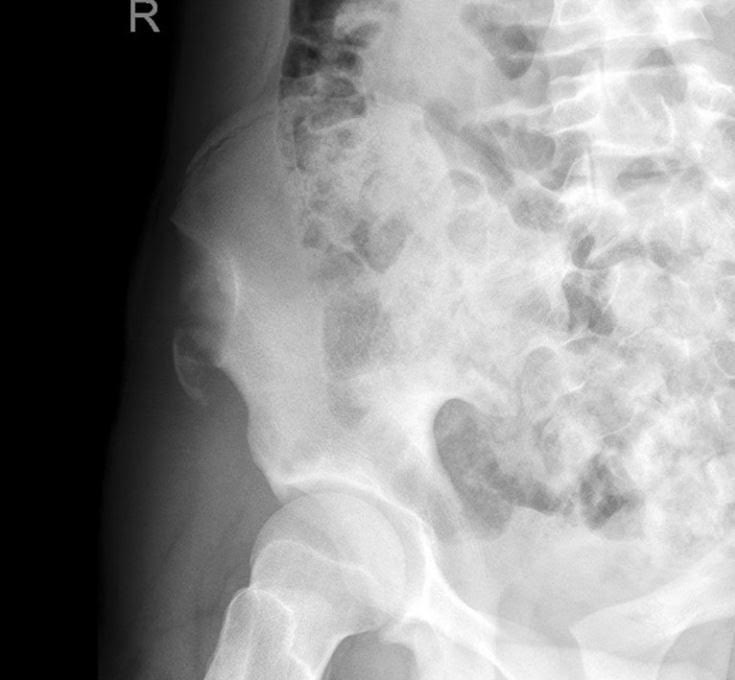
Answer: Avulsion fracture of the anterior superior iliac spine.
Injury:
An avulsion fracture of the anterior superior iliac spine is an uncommon injury seen almost exclusively in adolescent athletes.
They mostly result from a sudden, forceful, and/or unbalanced contraction of the attached musculotendinous unit (sartorius muscle or tensor fascia lata) during the starting phase of running, jumping, kicking, etc.
The most implicated sports include soccer, running, and ice hockey.
History/Exam:
The patient may report sudden shooting pain referred to the involved tuberosity.
Physical exam may include localized edema and tenderness to palpation and pain on passive ROM at the hip.
Anatomy:
The iliac crest is the weakest component of the pelvic ring during adolescence.
The avulsed fragment is usually displaced distally and laterally.
Treatment:
Conservative therapy includes 2-3 weeks of limited activity and walking with partial weight bearing restrictions and crutches. May also include bed rest with the affected lower extremity positioned with the hip and knee in flexion to ensure minimal tension of the muscles attaching to the ASIS. This is considered for minimally displaced fractures in younger children.
Surgical management generally consists of ORIF with a lag screw, and is generally recommended for patients with fracture fragments > 3cm or severely displaced fragments that cause compression of the lateral cutaneous nerve resulting in meralgia parasthetica.
Rossi F, Dragoni S. Acute avulsion fractures of the pelvis in adolescent competitive athletes: prevalence, location and sports distribution of 203 cases collected. Skeletal Radiol. 2001;30(3):127-31.
Kautzner J, Trc T, Havlas V. Comparison of conservative against surgical treatment of anterior-superior iliac spine avulsion fractures in children and adolescents. Int Orthop. 2014;38(7):1495-8.
Category: Toxicology
Keywords: mortality, predictors, MALA, pH, lactate (PubMed Search)
Posted: 2/12/2020 by Hong Kim, MD
Click here to contact Hong Kim, MD
Metformin associated lactic acidosis (MALA) has a high rate of mortality, ranging from 25% to 50%. Lactate level and acidemia are frequently associated with poor clinical outcome in many disease/medical conditions (e.g. sepsis).
A study investigated, via meta-analysis, if lactate level and pH were predictive of mortality in MALA.
Results
44 studies were identified from PubMed, EMBASE and Web of Science.
170 cases of MALA were included
pH and lactate were poor predictors of mortality based upon ROC curve
Conclusion
Category: Neurology
Keywords: spinal cord injury, cauda equina, urinary retention, incontinence (PubMed Search)
Posted: 2/12/2020 by WanTsu Wendy Chang, MD
Click here to contact WanTsu Wendy Chang, MD
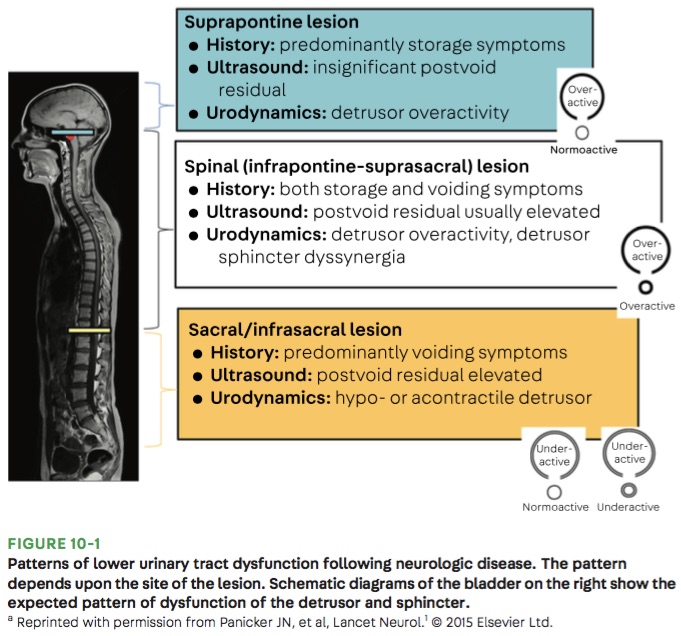
Bottom Line: Urinary retention can be seen with neurological injury involving the lower brainstem, spinal cord, cauda equina, and peripheral nerves.
Panicker JN, Sakakibara R. Lower urinary tract and bowel dysfunction in neurologic disease. Continuum (Minneap Minn). 2020;26(1):178-199.
Follow me on Twitter @EM_NCC
Category: Critical Care
Keywords: cerebral fat embolism, trauma, long bone fracture (PubMed Search)
Posted: 2/10/2020 by Mark Sutherland, MD
(Updated: 2/2/2026)
Click here to contact Mark Sutherland, MD
Don't forget cerebral fat embolism syndrome (FES) on the differential for altered trauma patients. FES is typically associated with long bone fractures, but has been reported with other fractures, orthopedic reaming (i.e. aggressive orthopedic procedures), and in rare cases even with non-fracture (soft-tissue) trauma. Typically symptoms occur between 24 and 72 hours after injury, but there have been cases both earlier and later. Diagnosis is clinical, but MRI may be helpful, and will often show multiple cerebral white matter lesions. It is debated whether FES is truly an embolic phenomena (i.e fat molecules traveling to and blocking blood supply of organs), or rather an inflammatory response to free fatty acids in the blood stream (i.e. more of a vasculitis type pathology). Management is supportive care, but give these patients time as there can be favorable outcomes, even after prolonged coma.
Morales-vidal SG. Neurologic Complications of Fat Embolism Syndrome. Curr Neurol Neurosci Rep. 2019;19(3):14.
From the diagnosis to the therapeutic management: cerebral fat embolism, a clinical challenge
https://www-ncbi-nlm-nih-gov.proxy-hs.researchport.umd.edu/pmc/articles/PMC6324602/
Category: Orthopedics
Keywords: Back pain (PubMed Search)
Posted: 2/8/2020 by Brian Corwell, MD
(Updated: 2/2/2026)
Click here to contact Brian Corwell, MD
Taking an accurate history to diagnose Cauda Equina Syndrome (CES)
Classic teaching is to inquire specifically about bowel and bladder function, sexual dysfunction, and/or loss of sensation in the groin.
Rather than asking about urinary incontinence, clinicians should ask specifically about difficulty passing urine, new leakage and retention.
Discussing issues related to sexual dysfunction are difficult for both clinicians and patients.
Rather than asking if there are any issues with sexual function, a more direct and informative way would be to ask if the patient has a “change in ability to achieve an erection or ejaculate” or “loss of sensation in genitals during sexual intercourse.”
Saddle anesthesia has the highest predictive value in diagnosing MRI-proven CES. Loss of sensation may be incomplete and patchy. Ask about change in sensation with wiping after a bowel movement.
Greenhalgh S, Truman C, Webster V, Selfe J. Development of a toolkit for early identification of cauda equina syndrome. Prim Health Care Res Dev. 2016;17(6):559-567.
Category: Pulmonary
Keywords: CAP, Pneumonia (PubMed Search)
Posted: 2/1/2020 by Ashley Martinelli
(Updated: 2/2/2026)
Click here to contact Ashley Martinelli
The new IDSA and American Thoracic Society guidelines for community acquired pneumonia were recently released. Major updates to the guidelines include but are not limited to:
1. It is not recommended to obtain sputum cultures in routine care. Consider only in patients who are intubated or empirically being treated for hospital associated pathogens such as MRSA or P. aeruginosa.
2. Blood cultures are only recommended for severe CAP managed in the hospital or those empirically being treated for MRSA or P. aeruginosa, or prior infection with those pathogens, or hospitalized and received parenteral antibiotics in the last 90 days.
3. Test for influenza during time periods when influenza is prominent (as in our current 2020 influenza outbreak).
4. Healthy patients can receive either amoxicillin 1g TID, doxycycline 100mg BID, or azithromycin 500mg followed by 250mg daily x 4 doses.
5. Patients with comorbidities such as chronic heart, lung, liver, or renal disease, diabetes, alcoholism, malignancy, or asplenia should receive combination therapy with a beta-lactam (amoxicillin/clavulanate, cefdinir, or cefpodoxime) + azithromycin or doxycycline. If allergies preclude the use of a beta-lactam, a fluoroquinolone (levofloxacin or moxifloxacin) can be used.
6. Patient admitted for non-severe CAP can receive combination beta-lactam (ampicillin/sulbactam, or ceftriaxone) and azithromycin therapy. Patients with severe beta-lactam allergies can receive either levofloxacin or moxifloxacin).
7. It is no longer recommended to add anaerobic coverage for suspected aspiration pneumonia unless the patient is suspected to have a lung abscess or empyema. It is most likely a chemical pneumonitis and should resolve within 24-48 hours with supportive therapy.
Metlay JP, Waterer GW, Long AC, et al. Diagnosis and treatment of adults with community-acquired pneumonia. An official clinical practice guideline of the American Thoracic Society and Infectious Diseases Society of America. Am J Resp Crit Care. 2019;200(7):e45-e67.
