Category: Pharmacology & Therapeutics
Keywords: Intranasal administration,fentanyl,ketorolac,sumatriptin,glucagon,desmopressin,midazolam (PubMed Search)
Posted: 10/6/2011 by Ellen Lemkin, MD, PharmD
Click here to contact Ellen Lemkin, MD, PharmD
There are an increasing number of intranasal medications commercially available for use, which is opportune as more and more intravenous medications become scarce.
These now include:
| Generic name | Brand Name | Usage |
| Fentanyl | Instanyl | Opiate analgesic |
| Ketorolac | Sprix | NSAID analgesic |
| Desmopressin (DDAVP) | Stimate | Bleeding |
| Vitamin B12 | Nasobal | Anti-migraine (yes!) |
| Sumatriptan | Imitrex | Anti-migraine |
| Zolmitripran | Zomig | Anti-migraine |
*******In addition, you can administer glucagon, midazolam and narcan intranasally as well.
Veldhorst-Jassen, NM, Fiddelers AA, Paul-Hugo M et all. A review of the clinical pharmacokinetics of opioids, benzodiazepines, and antimigraine drugs delivered intranasally. Clinical Therapeutics Nov 12, 20009;31(12):2954-87.
Wolfe TR, Braude DA. Intranasal Medication Delivery for Children: A Brief Review and Update. Pediatrics 2010;126;532:532-7.
Category: Neurology
Keywords: pontine stroke, pontine hemorrhage, corneal reflex, miosis, opiate abuse, opiate overdose (PubMed Search)
Posted: 10/5/2011 by Aisha Liferidge, MD
Click here to contact Aisha Liferidge, MD
Category: Neurology
Keywords: pontine stroke, pontine hemorrhage, corneal reflex, miosis, opiate abuse, opiate overdose (PubMed Search)
Posted: 10/5/2011 by Aisha Liferidge, MD
Click here to contact Aisha Liferidge, MD
Category: Critical Care
Posted: 10/4/2011 by Mike Winters, MBA, MD
(Updated: 2/3/2026)
Click here to contact Mike Winters, MBA, MD
Fever and ICH
Flower O, Smith M. The acute management of intracerebral hemorrhage. Curr Opin Crit Care 2011; 17:106-14.
Category: Visual Diagnosis
Posted: 10/3/2011 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
Question: 50-year-old diabetic female s/p foot burn several weeks ago, now presenting with pain and discharge from a poorly healing wound. Diagnosis?

Answer: Osteomyelitis
Osteomyelitis
· Acute or chronic bone infection
· Risk factors: Immunosuppression (diabetes, chronic steroid use, AIDS, and sickle-cell dz.)
· Secondary to direct trauma, contiguous spread from local infection, or hematogenous spread (in children)
· Common bacteria: S. Aureus, Pseudomonas, Salmonellae (classically in Sickle cell dz.)
· X-ray (limited sensitivity):
- 3-5 days post-infection: Soft-tissue swelling
- 14-21 days: Some patients demonstrate bony changes (e.g., periosteal elevation, bone lucencies, etc.)
- >28 days: >90% with Xray findings
· MRI is the imaging gold standard
· Two of the following needed for diagnosis:
- Purulent aspiration
- Positive blood or tissue culture
- Positive imaging
- Tenderness + erythema / edema
· Antibiotic coverage based on culture results. When immediate empiric therapy required (sepsis), cover most likely pathogen plus MRSA.
References
Carek PJ, Dickerson LM, Sack JL. Diagnosis and management of osteomyelitis. Am Fam Physician. 2001 Jun 15;63(12):2413-20.
Pruthi S, Thapa MM. Infectious and inflammatory disorders. Radiol Clin North Am. Nov 2009;47(6):911-26.
Zink BJ, Raukar NP. Bone and Joint Infections. In: Marx JA, Hockberger RS, Walls RM, Adams JG, Barsan WG, Biros MH, Danzl DF, Gausche-Hill M, Ling LJ, Newton EJ, eds. 7th ed. Emergency Medicine: Concepts and Clinical Practice.Volume 2. Philadelphia, PA: Mosby; 2010:1821-1830.
Follow me on Twitter (@criticalcarenow) or Google+ (+haney mallemat)
Category: Cardiology
Keywords: hostility, cardiovascular disease, acute myocardial infarction, acute coronary syndrome, coronary artery disease (PubMed Search)
Posted: 10/2/2011 by Amal Mattu, MD
(Updated: 2/3/2026)
Click here to contact Amal Mattu, MD
Hostile behavior appears to be a predictor of ischemic heart disease and myocardial infarction. Prior studies have demonstrated this association, and now one more study has supported this. In short, researchers from Nova Scotia demonstrated that observed hostility was a predictor of ischemic heart disease and myocardial infarction (2-fold), independent of age, sex, Framingham Risk Score, and other psychosocial risk factors.
The key takeaway point of this fun, but validated concept, is that in addition to exercising and eating right, we all just need to relax a bit more. And the next time you have to deal with an angry consultant, just tell him to chill out or he'll die!
Newman JD, et al. Observed hostility and the risk of incident ischemic heart disease. J Am Coll Cardiol 2011;58:1222-1228.
Category: Pharmacology & Therapeutics
Keywords: warfarin, creatinine, nephropathy (PubMed Search)
Posted: 9/27/2011 by Bryan Hayes, PharmD
(Updated: 10/1/2011)
Click here to contact Bryan Hayes, PharmD
An acute increase in the INR over 3 in patients with chronic kidney disease (CKD) is often associated with an unexplained acute increase in serum creatinine and an accelerated progression of CKD.
Kidney biopsy in a subset of these patients showed obstruction of the renal tubule by red blood cell casts, and this appears to be the dominant mechanism of the acute kidney injury. This has been termed warfarin-related nephropathy (WRN).
In 15,258 patients who initiated warfarin therapy during a 5-year period, 4006 had an INR over 3 and creatinine measured at the same time. A presumptive diagnosis of WRN was made if the creatinine increased by over 0.3 mg/dl within 1 week after the INR exceeded 3 with no record of hemorrhage. WRN occurred in 20.5% of the entire cohort, 33.0% of the CKD cohort, and 16.5% of the no-CKD cohort. Other risk factors included age, diabetes mellitus, hypertension, and cardiovascular disease. The 1-year mortality was 31.1% in patients with WRN compared with 18.9% in those without WRN, an increased risk of 65%.
Take home message: Although the mechanisms are not clear, be very wary of even a small creatinine bump in patients presenting with an INR > 3 on warfarin therapy. Yet another reason to fear warfarin...
Brodsky SV, et al. Warfarin-related nephropathy occurs in patients with and without chronic kidney disease and is associated with an increased mortality rate. Kidney Int 2011;80(2):181-9.
Category: Pediatrics
Keywords: Concussion, sports injury, TBI, return to play (PubMed Search)
Posted: 9/30/2011 by Mimi Lu, MD
Click here to contact Mimi Lu, MD
You are seeing a high school football player following a head injury. After your exam or head CT, you determine the child to have had a mild traumatic brain injury (aka concussion). You are ready to discharge him home when the parents or coach ask you when he can return to playing football.
A concussion is a form of functional, rather than structural, brain injury that displays no evidence of injury on structural neuroimaging. Symptoms include transient loss of consciousness, amnesia, vomiting, headache, poor school work, sleep changes, and emotional lability. Remember that children’s brains (even adolescents) are still developing, and are more prone to prolonged recovery following injury.
Recovery of symptoms usually follows a sequential course. Current guidelines recommend a stepwise return to play (aka concussion rehabilitation) involving both physical and cognitive rest (e.g. no texting, video games, limited school work). Once asymptomatic, the patient goes through each stage with at least 24 hours between stages. If symptoms return during a stage, then the patient is expected to return to the previous stage for 24 hours before attempting the higher stage again.
Return to Play Guidelines:
| Rehabilitation stage | Functional Exercise |
| Complete physical and cognitive rest |
| Walking, swimming, stationary cycling at 70% maximal heart rate, no resistance exercise |
| Specific sport related drills but no head impact |
| More complex drills, may start light resistance training |
| After medical clearance, participate in normal training |
| Normal game play |
References:
Category: Toxicology
Keywords: toxicology, pharmacist (PubMed Search)
Posted: 9/29/2011 by Fermin Barrueto
(Updated: 2/3/2026)
Click here to contact Fermin Barrueto
A growing trend in EDs is to have a dedicated ED Pharmacist present to assist with the evaluation of a patient's medication list, appropriate and safe drug administration and to improve drug delivery times. To date, it has been difficult for hospitals to determine if this was a cost-effective measure. There has been increasing research that has shown the proven benefits that physicians feel when they have an ED Pharmacist. With the aging population, increasing polypharmacy, core measure and national patient safety goals all rising to the top of hospital initiatives, the ED pharmacist will be proven to be a valuable cog of the ED - as UofMd already knows
1) Improved safety - this study showed an ED pharmacist caught 2.9 errors/100 medications, very important considering the cost of just one severe reaction can cause a hospitalization or even litigation(1)
2) Improved time to delivery of medication - this study showed improved time of delivery of medications not found in a Pyxis from 61 min with no pharmacist decreased to 47 min with ED pharmacist.(2)
Further studies will be needed to determine the true cost:benefit however with core measures like 6hr time to administration of antibiotics and the safe/timely adminstration of tPA combined with patient safety/quality goals - the value of an ED pharmacist will only be accentuated.
1 - Rothschild JM, Churchill W, Erickson A, et al. Medication errors recovered by emerency department pharmacists. Ann Emerg Med. 2010 Jun;55(6):513-21. Epub 2009 Dec 11.
2 - Owen KP. The role of the emergency department pharmacist in the timing of medication delivery. Clin Tox 2011. 49(6): 591.
Category: Neurology
Keywords: marcus gunn pupil, afferent pupillary defect, swinging flashlight test (PubMed Search)
Posted: 9/28/2011 by Aisha Liferidge, MD
Click here to contact Aisha Liferidge, MD
Category: Critical Care
Keywords: Epinephrine, adrenaline, cardiac arrest, return of spontaneous circulation, ROSC, critical care, ICU, saline (PubMed Search)
Posted: 9/27/2011 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
· The use of epinephrine in cardiac arrest is currently standard of care.
· Several observational and non-randomized trials have demonstrated the efficacy of epinephrine in cardiac arrest, but there has never been a randomized double-blind placebo-controlled trial in humans.
· A recently published Australian trial randomized cardiac patients (of any type) to receive either 1 mg of epinephrine (n=272) or 0.9% normal saline (n=262); the primary end-point was survival to hospital discharge. Secondary end-points were pre-hospital return of spontaneous circulation (ROSC) and neurological outcomes at hospital discharge.
· Significantly more patients had pre-hospital ROSC in the epinephrine group (regardless of the underlying rhythm), however, there was no statistically significant difference in survival to discharge (the primary outcome) between groups.
· This randomized double-blinded placebo-controlled trial raises many new and interesting questions about epinephrine, but more study is needed before changing current practice.
Jacobs IG, et al. Effect of adrenaline on survival in out-of-hospital cardiac arrest: A randomized double-blind placebo-controlled trial. Resuscitation 2011;82:1138-1143.
Follow me on Twitter (@criticalcarenow) or Google+ (+haney mallemat)
Category: Geriatrics
Keywords: fever, infections, elderly, geriatric (PubMed Search)
Posted: 9/25/2011 by Amal Mattu, MD
(Updated: 2/3/2026)
Click here to contact Amal Mattu, MD
Elderly patients in general have a lower baseline body temperature than younger patients. Consequently, it makes sense to redefine the definition of what constitutes a "fever" in the elderly. Rather than using the typical oral temperature cutoff of 38o C (100.4o F) for defining a fever, instead consider using 37.2o C (99o F). Redefining fever in this way increases the sensitivity for detecting bacterial infections from 40% to 83% while retaining an 89% specificity.
Caterino JM. Evaluation and management of geriatric infections in the emergency department. Emerg Med Clin N Am 2008;26:319-343.
Category: Orthopedics
Keywords: radial nerve, mononeuropathy (PubMed Search)
Posted: 9/24/2011 by Brian Corwell, MD
(Updated: 2/3/2026)
Click here to contact Brian Corwell, MD
Saturday night palsy - radial nerve mononeuropathy due to improper arm positioning associated with inebriated sleep.
Physical examination - Wrist and finger drop.
Patients may have findings suggestive of ulnar nerve co-involvement (interossei testing) which may falsely lead the examiner to consider a more proximal location for the lesion such as the brachial plexus.
The finger drop caused by the radial nerve lesion places the hand at a mechanical disadvantage. Adjust for this by examining the hand on a flat surface (stretcher, counter top). With the fingers now supported in extension at the MCP joint (no longer "dropped"), the interossei can now be tested in isolation and will be normal.
Category: Pediatrics
Keywords: ultrasound, intra-abdominal injury, free fluid, blunt trauma (PubMed Search)
Posted: 9/23/2011 by Mimi Lu, MD
Click here to contact Mimi Lu, MD
Category: Neurology
Keywords: glascow coma scale, GCS (PubMed Search)
Posted: 9/21/2011 by Aisha Liferidge, MD
(Updated: 2/3/2026)
Click here to contact Aisha Liferidge, MD
EYE OPENING
4 = spontaneous
3 = to voice
2 = to pain
1 = none
VERBAL RESPONSE
5 = orientated
4 = confused
3 = inappropriate
2 = incomprehensible
1 = none
MOTOR RESPONSE
6 = obeys command
5 = localizes pain
4 = withdraw to pain
3 = decorticate
2 = decerebrate
1 = none
Category: Critical Care
Posted: 9/20/2011 by Mike Winters, MBA, MD
Click here to contact Mike Winters, MBA, MD
Spontaneous Bacterial Peritonitis
Al-Khafaji A, Huang DT. Critical care management of patients with end-stage liver disease. Crit Care Med 2011; 39:1157-66.
Category: Visual Diagnosis
Posted: 9/19/2011 by Haney Mallemat, MD
(Updated: 8/28/2014)
Click here to contact Haney Mallemat, MD
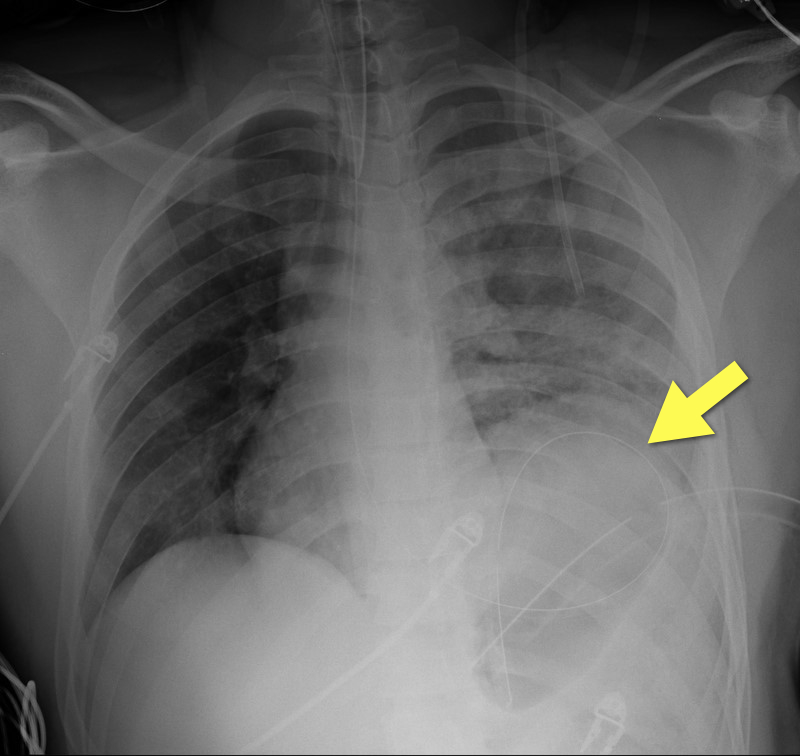
19 year-old male s/p high-speed MVC with hypotension and diminished breath sounds on left. Diagnosis?
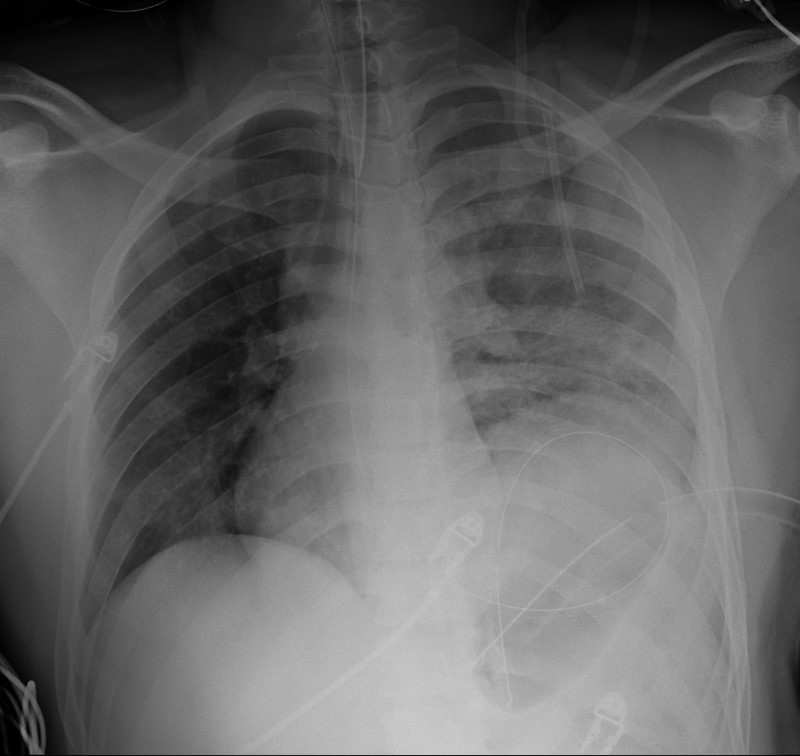
Answer: Diaphragmatic rupture (Note position of NG tube on image below).
·Uncommon; less than 1% of all traumatic injuries
·Diagnosis may be obvious on CXR (as in example) or subtle (e.g., diaphragmatic elevation, basilar atelectasis, etc.)
·Requires a high-index of suspicion because delayed diagnosis increases the risk of abdominal organ herniation or strangulation.
·Mortality depends on the mechanism and presence of associated injuries; mortality is highest for blunt injuries.
Bhavnagri S, et al. When and how to image a suspected broken rib. Cleveland Clinic J Med. 2009;76(5):309.
Williams M, et al. Predictors of mortality in patients with traumatic diaphragmatic rupture and associated thoracic and/or abdominal injuries. Am Surg. 2004;70(2):157.
National Trauma Data Base. American College of Surgeons 2000-2004.
Follow me on Twitter (@criticalcarenow) or Google+ (+haney mallemat)
Category: Cardiology
Keywords: acute MI, MI, myocardial infarction, acute coronary syndrome (PubMed Search)
Posted: 9/18/2011 by Amal Mattu, MD
(Updated: 2/3/2026)
Click here to contact Amal Mattu, MD
A patient presents to the ED in pulmonary edema, hypotensive, and has JVD. There's a new systolic murmur. The patient had an acute MI 7-10 days ago and had appropriate treatment and uncomplicated course, then discharge. What's the diagnosis and what do you do?
Step 1: Sign out immediately.
Step 2: If it's not time to sign out (just kidding about step 1), listen carefully to the murmur. If it's heard best at the lower sternal border, it's probably a ruptured papillary muscle with acute MR. If it's a "machinery" type murmur heard throughout the precordium loudly, it's probably an acute VSD.
Step 3: VSD patient is likely to die, but with either one, you've got to move quickly. IMMEDIATELY call cardiology AND cardiac surgery. The patient is in need of a balloon pump and OR.
All you can do is buy time until the patient goes upstairs....pressors for BP, IV NTG as tolerated for preload reduction, and be judicious with diuretics. Vasodilators might help unload the heart also. This patient may end up on 2-3 drips, and make sure ALL meds are titrateable. And just keep your fingers crossed!
Category: Orthopedics
Keywords: Posterolateral Corner, knee (PubMed Search)
Posted: 9/17/2011 by Michael Bond, MD
(Updated: 2/3/2026)
Click here to contact Michael Bond, MD
Posterolateral Corner Injuries
The posterolateral corner “PLC” of the knee is becoming increasingly recognized as an extremely important structure to maintain the stability of the knee joint.
PLC injuries occur with hyperextension, varus load and tibial external rotation. So the most common mechanism is a posterolaterally directed blow to the anteromedial tibia when the knee is hyperextended. PLC injuries are commonly associated with injury to other ligaments (ACL, PCL, LCL) and occur in isolation in <5% of cases. If suspected make sure to check for other ligamentous injuries.
Since this injury can be missed and is associated with significant disability it is important to test for it. This YouTube video, http://youtu.be/bnXaTdvZZ6o, demonstrates several examination techniques that can identify the injury.
Wheeless Online Ortho Reference http://www.wheelessonline.com/ortho/posterolateral_rotary_instability_of_the_knee
Category: Neurology
Keywords: bell palsy, bell's palsy, cranial nerve seven palsy, facial paralysis (PubMed Search)
Posted: 9/14/2011 by Aisha Liferidge, MD
(Updated: 2/3/2026)
Click here to contact Aisha Liferidge, MD
