Category: Orthopedics
Keywords: foot, plantar fasciitis (PubMed Search)
Posted: 3/10/2012 by Brian Corwell, MD
(Updated: 2/3/2026)
Click here to contact Brian Corwell, MD
The plantar fascia arises from the medial tuberosity of the calcaneous and extends to the proximal phalanges of the toes.
Pkantar Fasciitis is the most common cause of heel pain in adults.
Etiology is thought to be from a degenerative tear at the fascial origin followed by a tendinosis type reaction and .
Affects women 2x> men
More common in overweight patients.
Onset is insidious and not related to trauma.
Hx: Pain and tenderness directly over the medial calcaneal tuberosity and 1-2cm distally along the plantar fascia.
Pain is worse with prolonged standing/walking. Pain is most intense however when rising from a resting position such as first thing in the morning.
PE: Pain is increased with passive dorsiflexion of the toes. Tenderness to palaption over the medial calcaneal tuberosity and 1-2cm distally along the plantar fascia.(At times, one may have to apply increased pressure to approximate weight bearing type stress)
XR: Usually not necessary with a good history and exam. Heel spurs are seen in up to 50% with the disease (and in up to 20% without it!)
DDx: Tarsal tunnel syndrome. Calcaneal stress fracture. Fat pad atrophy. traumatic rupture of planter fascia.
Category: Pediatrics
Posted: 3/9/2012 by Rose Chasm, MD
(Updated: 2/3/2026)
Click here to contact Rose Chasm, MD
American Academy of Pediatrics PREP Curriculum
Category: Toxicology
Keywords: crotalinae, snake, pressure immobilization, envenomation (PubMed Search)
Posted: 3/4/2012 by Bryan Hayes, PharmD
(Updated: 3/8/2012)
Click here to contact Bryan Hayes, PharmD
Pressure immobilization involves wrapping the entire extremity with a bandage and then immobilizing the extremity with a splint. It is a technique routinely employed in the pre-hospital management of neurotoxic snakes in Australia.
A position statement was recently published by several international toxicology societies regarding the utility of pressure immobilization after North American Crotalinae snake envenomation (e.g., Copperheads, Timber rattlesnakes, Cottonmouths).
"Available evidence fails to establish the efficacy of pressure immobilization in humans, but indicates the possibility of serious adverse events arising from its use. The use of pressure immobilization for the pre-hospital treatment of North American Crotalinae envenomation is NOT recommended."
Pressure immobilization after North American Crotalinae snake envenomation. Clin Toxicol;2011;49(10):881-2.
Follow me on Twitter @pharmacytoxguy
Category: Critical Care
Posted: 3/6/2012 by Mike Winters, MBA, MD
(Updated: 2/3/2026)
Click here to contact Mike Winters, MBA, MD
Preventing VAP in the Intubated ED Patient
Ramirez P, et al. Measures to prevent nosocomial infections during mechanical ventilation. Curr Opin Crit Care 2012;18:86-92.
Category: Pharmacology & Therapeutics
Keywords: egg, influenza, vaccine (PubMed Search)
Posted: 3/2/2012 by Bryan Hayes, PharmD
(Updated: 3/4/2012)
Click here to contact Bryan Hayes, PharmD
The seasonal influenza vaccine is produced in chicken eggs. Ovalbumin, an egg protein, is often listed as a component of the purified vaccine on most drug-package inserts. The concentration of ovalbumin indicates the potential egg-allergen content of a vaccine.
Earlier ACIP guidelines recommended against giving the influenza vaccine to people with egg allergy, including those with a history of mild symptoms. However, several studies showed that influenza vaccine containing inactivated, or killed, virus is safe to give to people with egg allergy, especially those with a history of mild allergic reactions.
Influenza vaccines are now made with much lower ovalbumin concentrations than in the past; therefore, the level of potential egg protein allergens in a single dose of vaccine is extremely low.
The following are ACIP recommendations for the 2011 to 2012 influenza season:
http://www.niaid.nih.gov/topics/vaccines/research/Pages/eggAllergy.aspx
Recommended Adult Immunization Schedule - United States, 2012. MMWR Weekly. February 3, 2-12 / 61(04);1-7.
Follow me on Twitter (@pharmacytoxguy)
Category: Toxicology
Keywords: Octreotide, sulfonylurea, glucose, insulin (PubMed Search)
Posted: 3/1/2012 by Ellen Lemkin, MD, PharmD
Click here to contact Ellen Lemkin, MD, PharmD
Dougherty PP, Klein-Schwartz W. J. Med Toxicol 2010;6:199-206.
Category: Critical Care
Keywords: VAD, ventricular assist device, hear failure, shock, hemodynamics (PubMed Search)
Posted: 2/28/2012 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
Ventricular assist devices (VAD) pump blood from the left, right or both ventricles for patients in severe ventricular failure.
VADs may be placed temporarily (as a bridge to transplant) or permanently in patients who are not transplant candidates (also known as Destination Therapy)
Certain types of VADs continuously pump blood in a non-pulsatile fashion. In these cases, a patient may be perfusing normally without a palpable pulse.
Familiarity with potential VAD complications is important as a patient with a VAD may be presenting to an ED near you. Complications include:
Follow me on Twitter (@criticalcarenow) or Google+ (+haney mallemat)
Category: Visual Diagnosis
Posted: 2/27/2012 by Haney Mallemat, MD
(Updated: 8/28/2014)
Click here to contact Haney Mallemat, MD
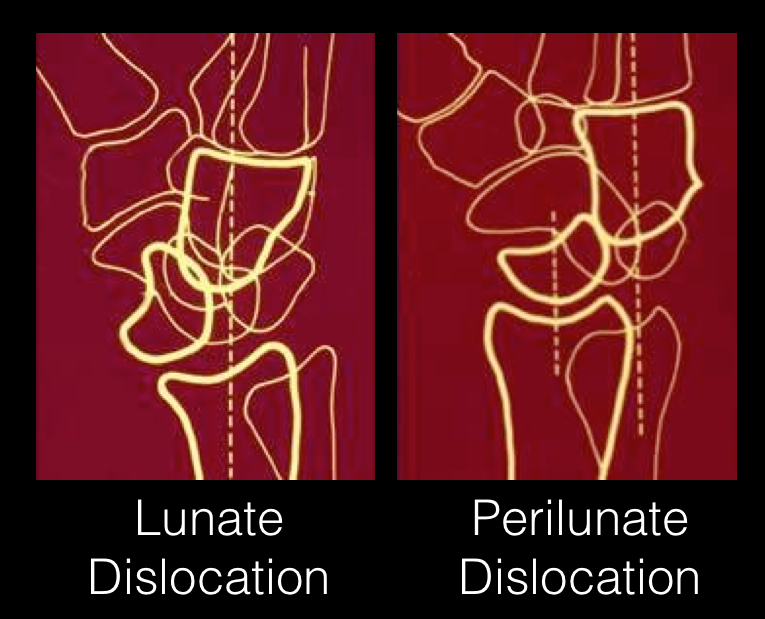
24 year-old male presents following fall from a scaffolding and complains of wrist pain. Diagnosis?

Answer: Perilunate dislocation
Perilunate dislocations usually occur following high-energy trauma (e.g., fall from a height); the mechanism is usually wrist hyperextension, ulnar deviation, and carpal supination.
Tenderness is palpated along the dorsum of the wrist; specifically distal to the lister tubercle along the scapholunate ligament; injuries may be associated with scaphoid fracture
Paresthesias may also occur along the median nerve distribution with up to 25% of cases developing carpal tunnel syndrome.
Treatment options include closed reduction and casting or open reduction and ligamentous repair with internal fixation.
The figure below illustrates the differences between lunate and perilunate dislocations.
References
Lunate and Perilunate Dislocations. Kannikeswaran, N & Sethuraman, U.
http://www.radiologyassistant.nl/en/42a29ec06b9e8 (diagram)
Follow me on Twitter (@criticalcarenow) or Google+ (+haney mallemat)
Category: Cardiology
Keywords: cardiogenic shock (PubMed Search)
Posted: 2/26/2012 by Amal Mattu, MD
(Updated: 2/3/2026)
Click here to contact Amal Mattu, MD
Quick pearls on cardiogenic shock
Post-MI cardiogenic shock is associated with a mortality of 50-70%. There are only a few interventions that have been demonstrated to improve outcomes: early use of intra-aortic balloon pump, stenting, and G2B3A inhibitors.
It is generally recommended to avoid clopidogrel since so many of these patients will require CABG.
Early use of mechanical ventilation decreases work of breathing and improves oxygenation.
Remember that age alone is not a contraindication to aggressive treatment.
Category: Orthopedics
Keywords: Heel, overuse injury, apophysis (PubMed Search)
Posted: 2/25/2012 by Brian Corwell, MD
(Updated: 2/3/2026)
Click here to contact Brian Corwell, MD
Severs disease
- Perhaps the most common overuse injury
-Pain is due to inflammation of the calcaneal apophysis growth plate
- Caused by repetitive microtrauma from the pull of the Achilles tendon on the apophysis.
- Occurs in young athletes ages 7-14
Sx’s bilateral in >50%
Hx – Gradual onset of posterior heel pain, worse with activity, better with rest.
PE – Tenderness at the insertion of the Achilles tendon onto the calcaneous. Swelling is mild.
This is a self limited condition because as the adolescent ages, the physis closes
Tx – Rest (no running or jumping), ice, NSAIDs, heel lifts/arch supports. Outpatient physical therapy for stretching and strengthening exercises.
Category: Pediatrics
Posted: 2/24/2012 by Mimi Lu, MD
Click here to contact Mimi Lu, MD
Category: Toxicology
Keywords: midazolam, lorazepam (PubMed Search)
Posted: 2/23/2012 by Fermin Barrueto
(Updated: 2/3/2026)
Click here to contact Fermin Barrueto
You have seen the study comparing diazepam to lorazepam IV for the cessation of seizures. Lorazepam one that one. Now, for prehospital status epilepticus midazolam IM went head to head with IV lorazepam to see which would stop seizure more quickly.
This study was more about the practicality of starting an IV than it was of the pharmacokinetics or onset of action of a particular benzodiazepine. It was a large enough study to warrant publication in New Engl J Med last month and is worth noting.
Subjects whose seizures ceased before ED arrival (median):
Time to active treatment: 1.2 min IM Midazolam group; 4.8 min IV Lorazepam group
Median times active treatment to cessation of SZ: 3.3 min IM Midazolam and 1.6 min IV Lorazepam
Safety was equal in both groups. This study validates EMS initiating therapy with IM midazolam for the cessation of seizures while intravenous access is being attempted.
Intramuscular versus intravenous therapy for prehospital status epilepticus.
Silbergleit R, Durkalski V, Lowenstein D, Conwit R, Pancioli A, Palesch Y, Barsan W; NETT Investigators.
N Engl J Med. 2012 Feb 16;366(7):591-600.
Category: Critical Care
Posted: 2/21/2012 by Mike Winters, MBA, MD
(Updated: 2/3/2026)
Click here to contact Mike Winters, MBA, MD
Ice-Cold Crystalloid for Therapeutic Hypothermia
Arulkumaran N, Ball SJ. Use of ice-cold crystalloid for inducing mild therapeutic hypothermia following out-of-hospital cardiac arrest. Resuscitation 2012;83:151-8.
Category: Medical Education
Keywords: Prezi, Power Point (PubMed Search)
Posted: 2/20/2012 by Rob Rogers, MD
(Updated: 2/3/2026)
Click here to contact Rob Rogers, MD
Getting tired of the same old Power Point presentations? Getting bored with Apple's Keynote? Looking for something new to excite learners?
Well, you might want to consider using a newer presentation tool, a tool designed to eliminate those boring bullet points...
Say hello to Prezi...
This really cool presentation tool allows you place all of your content (words, pictures, video, etc) on one canvas and then manipulate the sequence you want to show it in.
Check out the website and give it a try: www.prezi.com
Simply click on some of the sample Prezi presentations on the site. It's very cool and quite addictive.
ww.prezi.com
Category: Orthopedics
Keywords: Morton, neuroma (PubMed Search)
Posted: 2/18/2012 by Michael Bond, MD
(Updated: 2/3/2026)
Click here to contact Michael Bond, MD
Morton's Neuroma
Thomas JL, et al. Diagnosis and treatment of forefoot disorders: Morton's intermetatarsal neuroma. Journal of Foot and Ankle Surgery. 2009;48:251.
Category: Pediatrics
Posted: 2/17/2012 by Mimi Lu, MD
Click here to contact Mimi Lu, MD
Children & Appendicitis
Category: Critical Care
Keywords: pericardial tampaonde, shock, tamponade, fluids, hypoperfusion (PubMed Search)
Posted: 2/13/2012 by Haney Mallemat, MD
(Updated: 2/15/2012)
Click here to contact Haney Mallemat, MD
A fluid bolus is often the first-line therapy for patients with pericardial tamponade. A fluid bolus, however, may not always improve hemodynamics.
The cardiac index of forty-nine patients with cardiac tamponade was assessed before and after a 500 cc normal saline bolus:
Bottom-line: A fluid bolus may a reasonable first choice in a hypotensive patient with tamponade, but remember that fluid boluses may not always work. Attempts at fluid resuscitation should never delay definitive treatment with pericardiocentesis.
Sagrista-Sauleda, et al. Hemodynamic effects of volume expansion in patients with cardiac tamponade. Circulation 2008; 117:1545
Follow me on Twitter (@criticalcarenow) or Google+ (+haney mallemat)
Category: Visual Diagnosis
Posted: 2/13/2012 by Haney Mallemat, MD
(Updated: 8/28/2014)
Click here to contact Haney Mallemat, MD
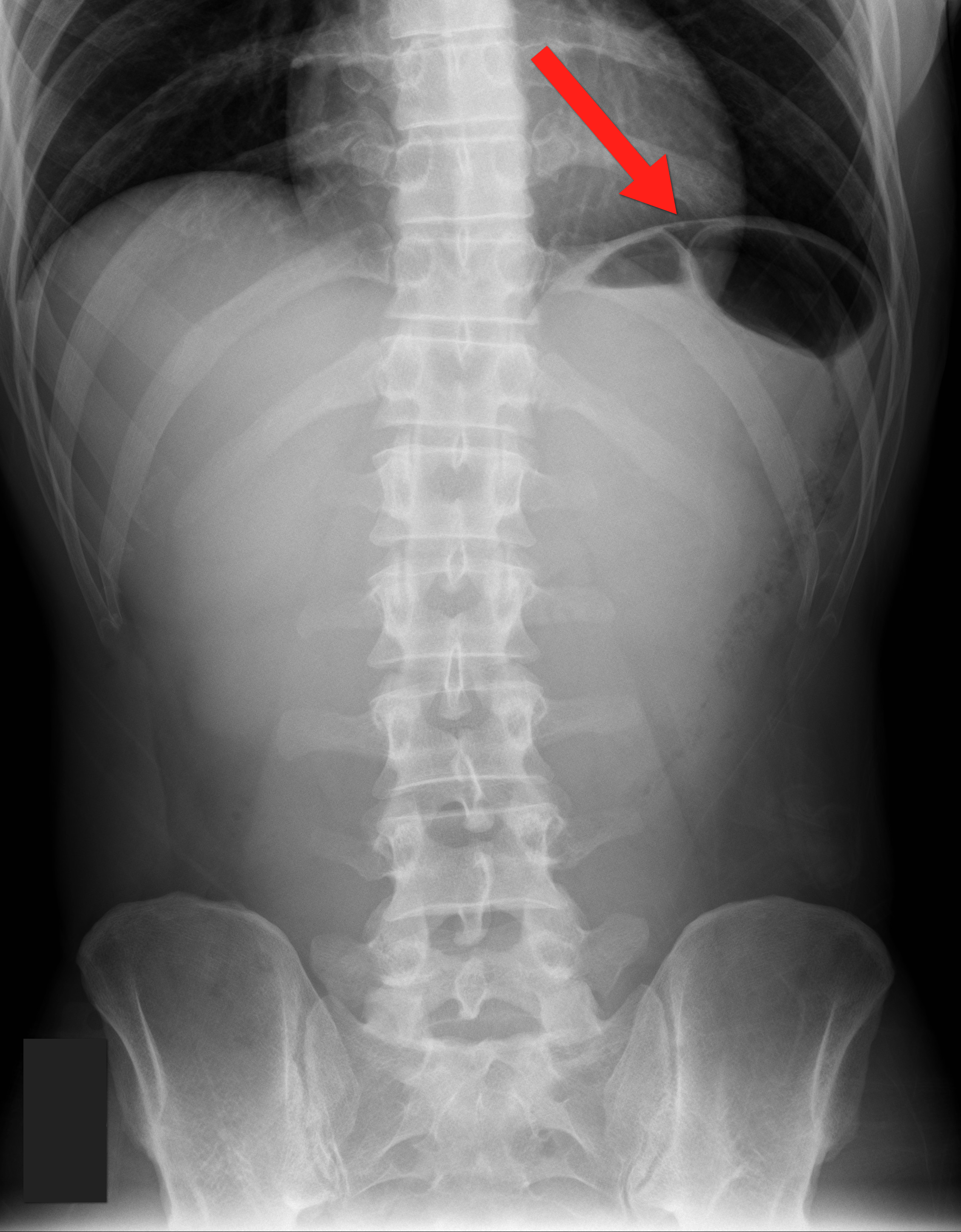
35 year old male with sudden onset of abdominal pain. Diagnosis?

Answer: Pneumoperitoneum
Follow me on Twitter (@criticalcarenow) or Google+ (+haney mallemat)
Category: Cardiology
Keywords: ACS, MI, painless, CAD, acute coronary syndrome (PubMed Search)
Posted: 2/12/2012 by Amal Mattu, MD
(Updated: 2/3/2026)
Click here to contact Amal Mattu, MD
You might think that patients with painless MIs might have a better prognosis than patients with pain. Unfortunately, this is just not true. A recent study (1) supported prior literature indicating that the lack of pain is not a predictor of a more benign course, and in fact patients with painless MIs have a higher in-hospital and 1-year mortality. There are several other factors that may associate lack of pain with worse outcomes (e.g. painless MIs occur more often in older patients), but regardless it's important to remember that (1) many patients with MI will present without pain, and (2) the lack of "typical" symptoms should not be reassuring.
Cho JY, et a. Comparison of outcomes of patients with painless versus painful ST-segment elevation myocardial infarction undergoing percutaneous coronary intervention. Am J Cardiol 2012;109:337-343.
Category: Orthopedics
Keywords: herbal, supplements, complementary medicine (PubMed Search)
Posted: 2/11/2012 by Brian Corwell, MD
Click here to contact Brian Corwell, MD
Common herbs and supplements used to treat pain
1) Turmeric root - used for arthritis pain. Little evidence to support its use. May slow blood clotting/enhance anticoagulant/antiplatelet effects.
2) Boswellia - used for OA and RA pain. Little evidence to support its use.May interfere with anticoagulant drugs and leukotreine inhibitors.
3) St. John's Wort - used for HA, migraine, neuralgia, muscle pain, sciatica, fibromyalgia. Little to no evidence to support its use.May interfere with numerous medications including anticoagulants, digoxin and SZ medications.
4) Glucosamine and Chondroitin - used for OA, knee pain, back pain. The glucosamine/chondroitin arthritis intervention trial found that "the dietary supplements Glucosamine and Chondroitin, taken alone or in combination are generally ineffective for OA pain of the knee." May increase the effect of Warfarin.
5) KavaKava - used for HA, muscle pain. Insufficient evidence demonstrating effectiveness for treatment of painful conditions. May cause severe liver damage and potentiate drowsiness side effects of other medications.
6) Echinacea - used for pain, migraines, arthritis. Little evidence to support its use. May exacerbate symptoms of autoimmune disorders.
7) Valerian root – used for joint and muscle pain. Insufficient evidence to support its use. May potentiate sedative side effects of barbiturates and benzos.
8) Chinese Thunder God Vine – used for arthritis. There is some evidence to suggest that this agent has anti-inflammatory properties. Long term this agent may decrease bone mineral density in women, decrease fertility in men, and may produce GI side effects.
9) Feverfew – used for muscle pain, arthritis. Some evidence to suggest that may reduce frequency of migraine headaches. No evidence for benefit in RA. May enhance effects of anticoagulants and some drugs that undergo hepatic metabolism.
10) Cat’s claw – used for herpes zoster, bone pain, arthritis. Possible benefit for OA and RA in small studies in humans but no large study has shown benefit. May interact with clotting agents, BP meds and cyclosporine.
11) Black Cohosh – used for muscle pain and arthritis. Insufficient evidence demonstrating benefit. May be associated with severe liver side effects.
12) Bromelain – used for muscle pain, arthritis, knee pain. The NIH reports that bromelain may be effective for arthritis when used in combination with trypsin and rutin. May interact with amoxicillin and other antibiotics, anticoagulants and antiplatelet drugs.
13) Devil’s claw – used for muscle pain, back pain, arthritis, migraine. The NIH reports that “taking devil’s claw alone or with NSAIDs seems to help decrease OA related pain.” May increase effects of warfarin.
