Category: Critical Care
Posted: 7/24/2012 by Mike Winters, MBA, MD
(Updated: 2/3/2026)
Click here to contact Mike Winters, MBA, MD
Steroids and Septic Shock
Sherwin RL, Garcia AJ, Bilkovski R. Do low-dose corticosteroids improve mortality or shock reversal in patients with septic shock? A systematic review and position statement prepared for the American Academy of Emergency Medicine. JEM 2012;43:7-12.
Category: Visual Diagnosis
Posted: 7/23/2012 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
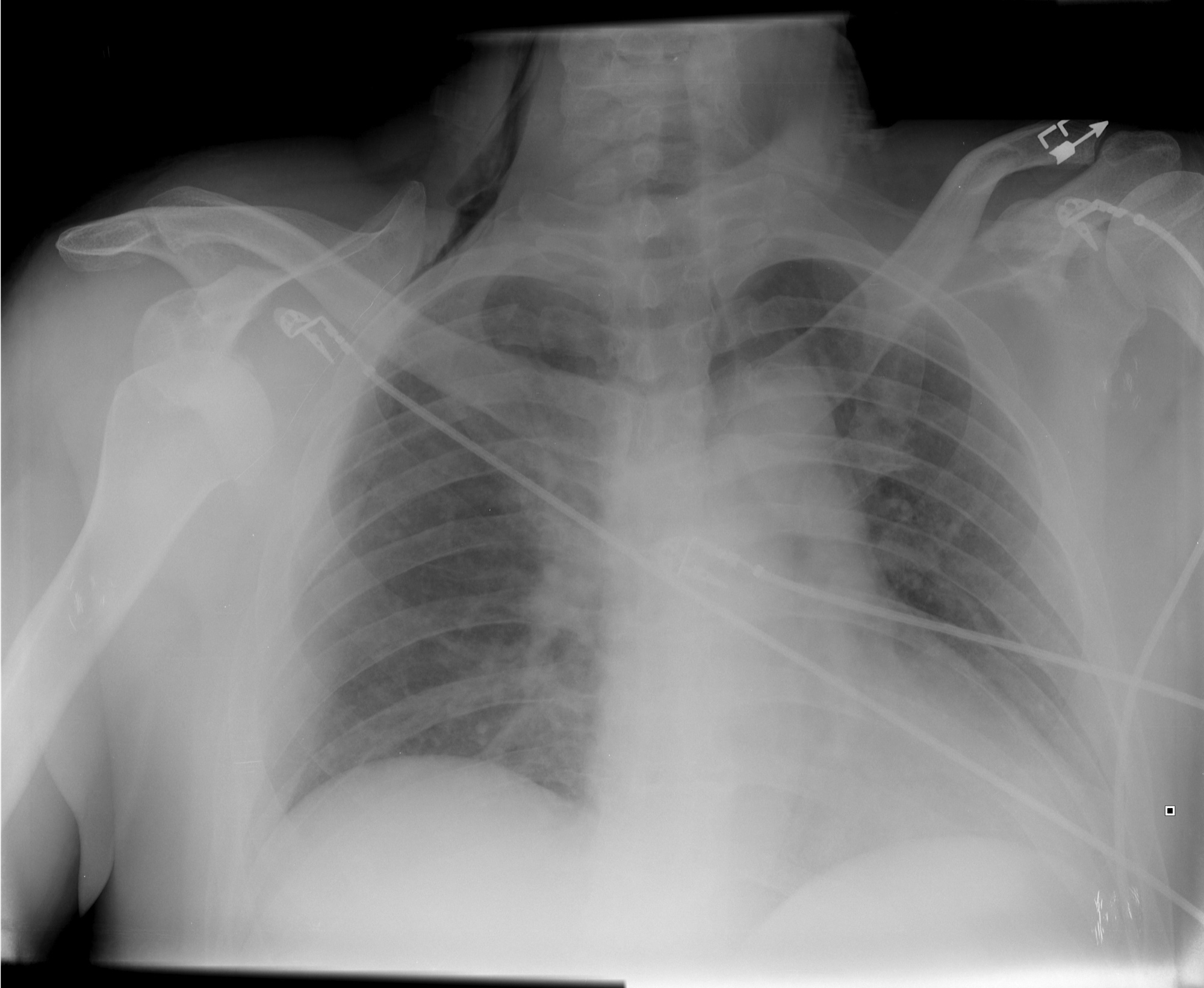
Find four abnormalities in the chest Xray below.
Follow me on Twitter (@criticalcarenow) or Google+ (+haney mallemat)
Category: Orthopedics
Keywords: Humerus Fractures (PubMed Search)
Posted: 7/21/2012 by Michael Bond, MD
(Updated: 8/28/2014)
Click here to contact Michael Bond, MD
Humerus Fractures, Proximal
Category: Pediatrics
Keywords: leukemia, back pain, cancer (PubMed Search)
Posted: 6/29/2012 by Mimi Lu, MD
(Updated: 7/20/2012)
Click here to contact Mimi Lu, MD
Category: Critical Care
Posted: 7/17/2012 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
Wernicke encephalopathy (WE) is a neurologic disorder secondary to prolonged thiamine deficiency; it is characterized by confusion, ataxia, and ocular abnormalities.
Traditional medical teaching advises against the administration of glucose (or glucose containing fluid) in thiamine deficient patients, without first giving thiamine, as this may precipitate WE.
This teaching is problematic, however, in hypoglycemic patients who require the immediate administration of glucose while simultaneously being suspected of thiamine deficiency (e.g., malnourished alcoholics). Delays in treating hypoglycemia may be more harmful (e.g., seizures, permanent neurologic deficits, etc.) than the risk of WE.
Schabelman et. al performed a literature search to unearth the origins of this teaching. Nineteen papers related to this topic were found consisting of case reports, animal studies, and expert opinion; there were no randomized trials, cohort studies, or case-control studies.
Bottom-line: The available evidence does not support withholding glucose treatment until thiamine can be administered and educators should consider abolishing this dogmatic teaching until better evidence is available.
Schabelman, et al. Glucose before thiamine for Wernicke encephalopathy: a literature review. J Emerg Med. 2012 Apr; 42(4): 488-94
Follow me on Twitter (@criticalcarenow) or Google+ (+haney mallemat)
Category: Visual Diagnosis
Posted: 7/15/2012 by Haney Mallemat, MD
(Updated: 7/16/2012)
Click here to contact Haney Mallemat, MD
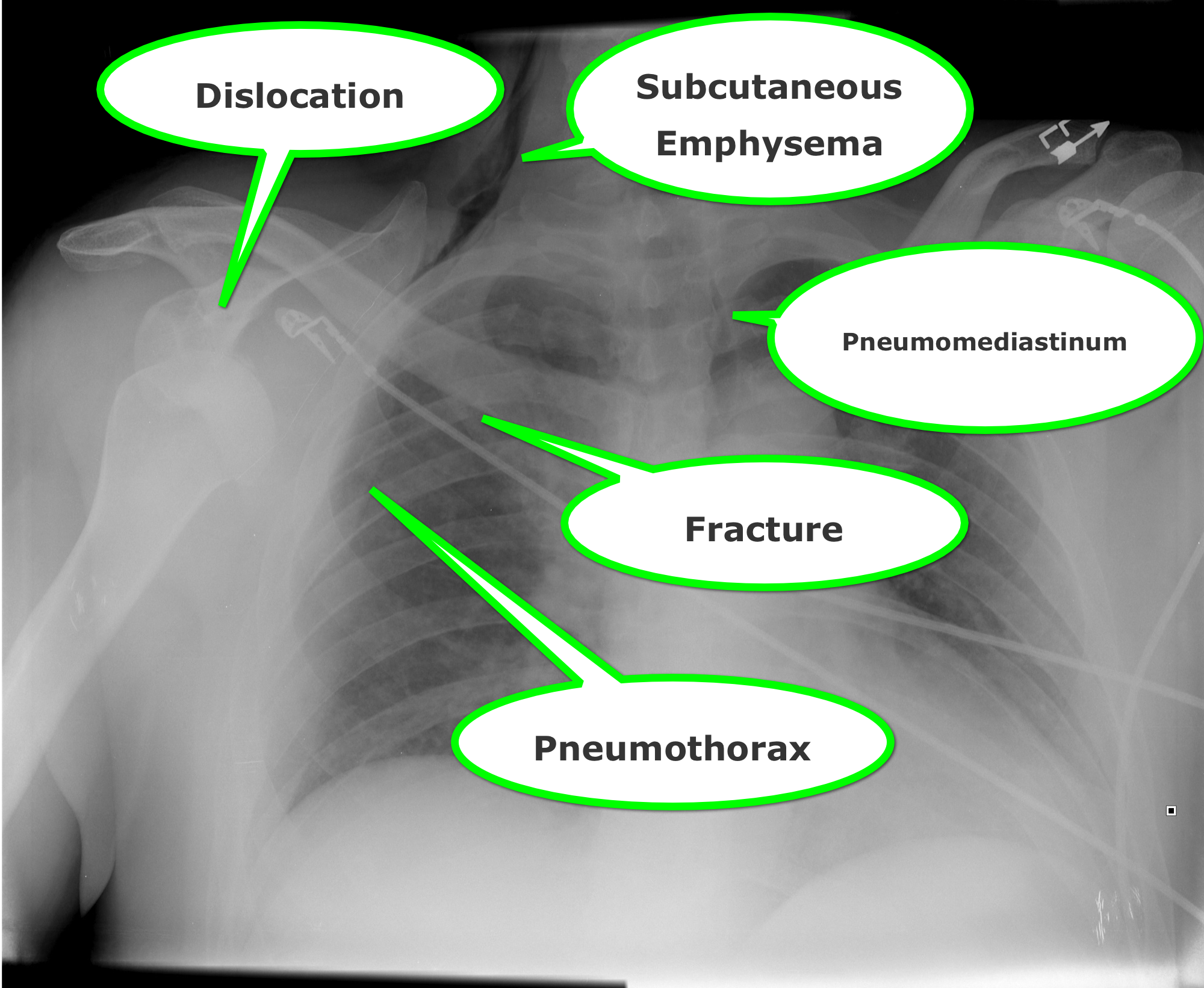
23 year-old female presents complaining of progressive right lower quadrant pain after doing "vigorous" pushups. CT abdomen/pelvis below. What’s the diagnosis? (Hint: it’s not appendicitis)

Answer: Rectus Sheath Hematoma
Rectus Sheath Hematoma (RSH)
Rectus muscle tear causing damage to the superior or inferior epigastric arteries with subsequent bleeding into the rectus sheath; uncommon cause of abdominal pain but mimics almost any abdominal condition.
May occur spontaneously, but suspect with these risk factors:
Typically a self-limiting condition, but hypovolemic shock may result from significant hematoma expansion.
Follow me on Twitter (@criticalcarenow) or Google+ (+haney mallemat)
Category: Cardiology
Keywords: Atrial fibrillation, a fib (PubMed Search)
Posted: 7/15/2012 by Semhar Tewelde, MD
(Updated: 2/3/2026)
Click here to contact Semhar Tewelde, MD
Atrial fibrillation is most commonly associated with cardiovascular disease
Non cardiac causes: pulmonary disease/PE, hyperthyroidism, sympathomimetics, drugs/ETOH
AFFIRM & RACE trials compared outcomes of a fib patients treated w/ rate vs. rhythm control
- No significant difference in survival between groups
Risk of thromboembolic CVA
- Rhythm control = Rate control + anticoagulation
New data challenges the need for strict heart rate control
- Resting heart rate should be <110 bpm
Use CHADS2 score to identify who requires anticoagulation based on %risk of emboli
- Chronic heart failure, HTN, Age>75, DM, Stroke/TIA
Atrial Fibrillation. Bontempo L, Goralnick E. Emerg Med Clin N Am 29 (2011)747-758.
Category: Orthopedics
Keywords: Ulnar nerve, compression, neuropathy, wrist (PubMed Search)
Posted: 7/14/2012 by Brian Corwell, MD
(Updated: 2/3/2026)
Click here to contact Brian Corwell, MD
The median nerve is not the only compression neuropathy of the wrist
The ulnar nerve can become compressed at the level of the wrist as it 1) enters Guyon's canal or 2) or as the deep branch curves around the hook of the hamate
Compression can occur due to carpal bone fractures, local inflammation, ganglias, lipomas, anatomic abnormalities, etc
In sports medicine, the most common mechanism is injury is seen in cyclists (cyclist/handlebar palsy)
http://www.hughston.com/hha/b_15_3_2a.jpg
Also seen in those who participate in racquet sports, baseball, and golf
Symptoms can be isolated motor (claw hand = rare), sensory or both
http://en.academic.ru/pictures/enwiki/85/Ulnar_claw.jpg
Can be associated w/ median nerve compression
Tx: Activity modification such as wearing padded gloves, padding the object, or changing hand position on the handlebars
If above fails, surgical decompression is very effective.
Category: Pediatrics
Posted: 7/13/2012 by Rose Chasm, MD
(Updated: 2/3/2026)
Click here to contact Rose Chasm, MD
NMS Pediatrics, 4th edition
Category: Toxicology
Keywords: cocaine, levamisole, leukoencephalopathy (PubMed Search)
Posted: 7/10/2012 by Bryan Hayes, PharmD
(Updated: 7/12/2012)
Click here to contact Bryan Hayes, PharmD
Levamisole is a pharmaceutical with anthelminthic and immunomodulatory properties that was previously used in both animals and humans to treat inflammatory conditions and cancer.
It has been identified as a cocaine adulterant in the U.S. since 2003, with the DEA estimating that by 2009 up to 70% of cocaine seized contained levamisole.
Leukopenia, agranulocytosis, and vasculitis are well known complications of levamisole use.
One important complication to keep in mind is the possibility of multifocal inflammatory leukoencephalopathy (MIL). Although no formal case of leukoencephalopathy in the setting of cocaine use has yet been reported, various neurological side effects were described with levamisole therapy, the most concerning complication being MIL.
Larocque A, Hoffman RS. Levamisole in cocaine: Unexpected news from an old acquaintance. Clin Toxicol. 2012;50:231-41.
Follow me on Twitter (@PharmERToxGuy)
Category: Critical Care
Posted: 7/10/2012 by Mike Winters, MBA, MD
(Updated: 2/3/2026)
Click here to contact Mike Winters, MBA, MD
Anaphylaxis
De Bisschop MB, Bellou A. Anaphylaxis. Curr Opin Crit Care 2012; 18:308-17.
Category: Visual Diagnosis
Posted: 7/8/2012 by Haney Mallemat, MD
(Updated: 7/9/2012)
Click here to contact Haney Mallemat, MD
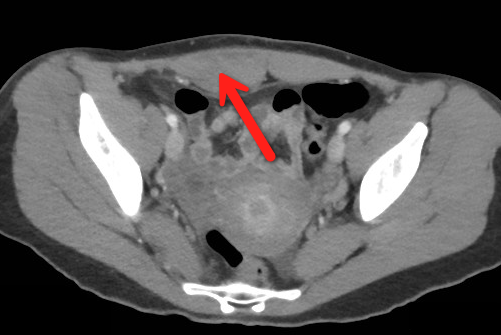
A previously healthy 3 year-old male presents with a one-day history of fever, drooling, and refusal to move his neck. The lateral neck x-ray is shown. What's the diagnosis?
Answer: Retropharyngeal abscess
Retropharyngeal Abscess (RPA)


Follow me on Twitter (@criticalcarenow) or Google+ (+haney mallemat)
Category: Pharmacology & Therapeutics
Keywords: alteplase, tPA, warfarin, INR, ischemic stroke (PubMed Search)
Posted: 7/2/2012 by Bryan Hayes, PharmD
(Updated: 7/7/2012)
Click here to contact Bryan Hayes, PharmD
Issue 1: Mean INR in study patients was only 1.22 (median 1.2). An INR of 1.2 represents very little actual anticoagulation.
Issue 2: In the small subgroup of patients with INR 1.5 to 1.7 (n = 269) there was a higher risk of ICH (7.8%), but did not reach statistical significance (it was significant in the unadjusted risk population).
Bottom line: Patients with INRs < 1.5 may be ok to receive tPA. Patients with INRs 1.5 or greater need further study.
Xian Y, Liang L, Smith EE, et al. Risk of Intracranial Hemorrhage Among Patients With Acute Ischemic Stroke Receiving Warfarin and Treated with Intravenous Tissue Plasminogen Activator. JAMA. 2012;307(24):2600-8.
Follow me on Twitter (@PharmERToxGuy)
Category: Toxicology
Keywords: envenomation,stings,jellyfish (PubMed Search)
Posted: 7/5/2012 by Ellen Lemkin, MD, PharmD
Click here to contact Ellen Lemkin, MD, PharmD
No one treatment has demonstrated consistency of pain relief from jellyfish stings over all species; conversely, a treatment for one species may worsen an envenomation from another.
Deionized water, seawater, meat tenderizer, and urea treatment do not appear to produce any improvement in pain sensation.
Ammonia, acetic acid, and ethanol may cause an increased stinging sensation, and in most species vinegar may cause nematocyst discharge.
Application of topical lidocaine reduced the local sensation of pain (10% and 15% produced immediate pain relief), and hot water results in pain relief in the majority of patients tested.
Ward NT, Darracq MA, Tomasewski C, Clark RF. Evidence-Based Treatment of Jellyfish Stings in North America and Hawaii. Article published online, Annals of Emergency Medicine June 8, 2012.
Category: Critical Care
Keywords: hydroxyethyl starch crystalloid, colloid, lactated ringers, normal saline, resuscitation, sepsis, hypotension (PubMed Search)
Posted: 7/3/2012 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
Septic patients with hemodynamic instability often require intravenous fluids as part of their resuscitation. Major debate has occurred whether the optimal resuscitation fluids are crystalloids (e.g., normal saline) or colloids (e.g., albumin).
In theory, colloids are more potent intravascular expanders than crystalloids because their oncotic pressure is higher and should increase intravascular volume similarly to larger amounts crystalloid (i.e., colloids require less volume during resuscitation).
Despite these theoretical benefits, the colloid hydroxyethyl starch (HES), has come under scrutiny after prior studies have linked its use with adverse outcomes.
A recent prospective randomized-control trial compared the use of HES to lactated acetate for resuscitating septic patients and found that HES significantly increased both the incidence of renal-replacement therapy and mortality at 90 days (both primary end-points in the study).
Bottom line: There is no convincing data that HES performs superiorly to crystalloid for resuscitation in sepsis and there is increased harm with its use. Furthermore, the increased cost of HES compared to crystalloids does not justify its routine use.
Perner A., et al. Hydroxyethyl Starch 130/0.4 versus Ringer's Acetate in Severe Sepsis. NEJM. 2012 Jun 27.
Follow me on Twitter (@criticalcarenow) or Google+ (+haney mallemat)
Category: Visual Diagnosis
Posted: 7/2/2012 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
Have you ever had to give a national presentation, but can't find that one ultrasound clip or image that you really need? You could "borrow" it from someone on the internet, but you are secretly afraid that the "owner" of the clip is lurking somewhere in the audience. Well, the guys at the Ultrasound Podcast (www.ultrasoundpodcast.com) have come to your rescue by creating SonoCloud, a free access ultrasound library. At Sonocloud, you will find several categories of ultrasound clips and images for you to view and share,...and again it's FREE. In fact, the only thing you are expected to do is upload some of your own ultrasounds to share.
Follow me on Twitter (@criticalcarenow) or Google+ (+haney mallemat)
Category: Cardiology
Keywords: cocaine (PubMed Search)
Posted: 7/1/2012 by Amal Mattu, MD
(Updated: 2/3/2026)
Click here to contact Amal Mattu, MD
[Pearls provided by Dr. Semhar Tewelde]
Cocaine...
1. causes systolic and diastolic dysfunction, arrhythmias, and atherosclerosis even in young users with relatively few cardiac risk factors, typically TIMI risk score <1
2. decreases myocardial contractility and ejection fraction by blocking sodium and potassium channels within the myocardium
3. prolongs the PR, QRS, and QT intervals on the ECG
4. users have a higher overall incidence of MI (odds ratio 3.8 to 6.9)
5. -induced chest pain is associated with acute MI in approx. 6% of cases
6. increases the risk of MI by 24-fold in the first hour after use
7. contributes to approx. 1 of every 4 MIs between 18 and 45 years of age
Cardiovascular Effects of Cocaine. Schwartz B, et al. Circulation. 2010;122:2558-2569.
Category: Orthopedics
Keywords: Bennett, Rolando, fracture (PubMed Search)
Posted: 6/30/2012 by Michael Bond, MD
(Updated: 2/3/2026)
Click here to contact Michael Bond, MD
First Metacarpal Fractures:
There are two types of fractures that commonly occur at the base of the 1st metacarpal. They are:
Bennett Fracture: This is an intraarticular fracture at the base of the 1st metacarpal that always involves some degree of subluxation or dislocation of the 1st carpometacarpal joint.

Image from Wikipedia Commons
Rolando Fracture: This is a communited intraarticular fracture at the base of the first metacarpal that typically has a T or Y shaped configuration with 3 fragments.

Image courtesy of WikiPedia Commons
Category: Pediatrics
Posted: 6/29/2012 by Rose Chasm, MD
(Updated: 2/3/2026)
Click here to contact Rose Chasm, MD
Submitted by Dr. Lauren Rice
The summertime can be full of lots of fun activities (beach, fireworks, cookouts, and campfires) that can put children at risk of burns.
Burn depth classification:
1. Superficial (first-degree): red and blanching with minor pain, resolves in 5-7 days
2. Partial thickness (second-degree): red and wet with blisters, very painful, resolves in 2-5 weeks
Treatment: clean with soap and water twice daily, and apply silvadene wrap with gauze, kerlex
3. Full thickness (third-degree): dry and leathery without pain, no resolution after 5-6 weeks, may require graft
Treatment: wound debridement and dressings as above
Parkland formula: 4ml/kg/%TBSA in 1st 24 hours with 50% of total volume in 1st 8 hours
Calculate burn surface area:
-SAGE: free computerized burn diagram available at www.sagediagram.com
-Rule of Nines > 14 years old
-Rule of Palm <10 years old
Burn Center Referral
-Extent: partial thickness of >30% TBSA or full thickness of >10-20%
-Site: hands, feet, face, perineum, major joints
-Type: electrical, chemical, inhalation
1. Cross, J.T. and Hannaman, R.A. MedStudy Pediatrics Board Review Core Curriculum, 5th edition, p. 3-11, 3-12.
2. Children’s National Medical Center, Department of Trauma and Burn Surgery. Trauma Cheat Sheet.
Category: Pediatrics
Posted: 6/23/2012 by Mimi Lu, MD
(Updated: 6/29/2012)
Click here to contact Mimi Lu, MD
Pathology at the umbilicus can manifest as inflammation, drainage, a palpable mass, or herniation.
Omphalitis - A cellulitis of the umbilicus. Mild cases often respond to local application of alcohol to clean the area, but due to the possibility of rapid progression and abdominal wall necrotizing fasciitis, admission for observation and IV antibiotics is usually warranted. Cover staph, strep, and GNRs.
Umbilical granuloma - As the umbilical ring closes and the cord sloughs off, granulation tissue formation is a normal part of umbilical epithelialization. There is sometimes an overgrowth of granulation tissue which can be treated once or twice with silver nitrate. Should the tissue not regress after a 1-2 treatments, the patient should be referred to pediatric surgery for excision and evaluation of other pathology (urachal or vitelline remnants).
Umbilical fistula - This is a patent vitelline duct and is characterized by persistent drainage that is bilious or purulent. A fistulogram using a small catheter and radio opaque dye can sometimes be helpful in determining the source of drainage (dye should be seen in the small bowel).
Umbilical polyp - Often confused with an umbilical granuloma with its glistening cherry red appearance, this is actually a vitelline duct remnant and contains small bowel mucosa. It does not regress with silver nitrate.
Vesicoumbilical fistula/sinus - The urachal versions of the umbilical fistula. This are a failure of complete closure of the urachus, resulting in persistent drainage of urine from the umbilicus, and infection (including recurrent UTIs). A fistulogram can be helpful for diagnosis.
