Category: Toxicology
Keywords: propylene glycol, lorazepam, phenytoin (PubMed Search)
Posted: 10/4/2012 by Fermin Barrueto
(Updated: 2/3/2026)
Click here to contact Fermin Barrueto
Ever have that alcholic who requires lorazapam doses that start to approach 10mg? 20mg? or even higher. The next step is usually a lorazepam infusion and then send them to the ICU. In the ICU, the patient develops an unexplained anion gap lactic acidosis.
Check a Lactate - lorazepam has 80% propylene glycol (PG). PG is metabolized to lactate which can accumulate when a lorazepam infusion at an elevated dose is running constantly. Hypotension, bradycardia and even other EKG changes have been reported. Simply discontinue the infusion and assess your acid-base status.
Other IV meds that contain PG:
lorazepam - 80% PG
Phenytoin - 40% PG
Phenobarbital - 67.8%
Diazepam - 40% PG
Category: Toxicology
Keywords: Cannabinoid,hyperemesis, marijauna (PubMed Search)
Posted: 10/4/2012 by Ellen Lemkin, MD, PharmD
(Updated: 2/3/2026)
Click here to contact Ellen Lemkin, MD, PharmD
Michael Hiotis PharmD, CSPI. ToxTidbits. Maryland Poison Center Sep 2012
Category: Critical Care
Posted: 10/2/2012 by Mike Winters, MBA, MD
(Updated: 2/3/2026)
Click here to contact Mike Winters, MBA, MD
Thrombotic Thrombocytopenic Purpura (TTP)
Kessler CS, et al. Thrombotic thrombocytopenic purpura: A hematological emergency. J Emerg Med 2012; 43:538-44.
Category: Visual Diagnosis
Posted: 10/1/2012 by Haney Mallemat, MD
(Updated: 10/2/2012)
Click here to contact Haney Mallemat, MD
Do you place central-lines?
Do you suture your central-lines into place?
Do you ever get worried that you are going to stick yourself with that needle?
If you answered yes to any of these questions, then maybe this pearl is for you; click here
Follow me on Twitter (@criticalcarenow) or on Google+ (+haney mallemat)
Category: Cardiology
Keywords: Heyde s Syndrome, aortic stenosis, angiodysplasia (PubMed Search)
Posted: 9/30/2012 by Semhar Tewelde, MD
(Updated: 2/3/2026)
Click here to contact Semhar Tewelde, MD
Aortic valve (AV) stenosis associated with gastrointestinal angiodysplasia
Proteolysis of Von Willebrand (type 2A) as it passes through the stenotic valve is one culprit of bleeding
Hemostatic abnormalities e.g. GI bleed are often corrected after AV replacement
Valve replacement is only recommended for cardiac symptoms
Vincentelli A, Susen S, et al. Acquired von Willebrand Syndrome in Aortic Stenosis. N Engl J Med 2003; 349:343-349
Category: Orthopedics
Keywords: Fight, bite (PubMed Search)
Posted: 9/29/2012 by Michael Bond, MD
Click here to contact Michael Bond, MD
Fight Bites
Category: Pediatrics
Keywords: dysrhythmia, arrhythmia (PubMed Search)
Posted: 9/28/2012 by Mimi Lu, MD
Click here to contact Mimi Lu, MD
The incidence of pediatric syncope is common with 15%-25% of children and adolescents experiencing at least one episode of syncope before adulthood. Incidence peaks between the ages of 15 and 19 years for both sexes.
Although most causes of pediatric syncope are benign, an appropriate evaluation must be performed to exclude rare life-threatening disorders. In contrast to adults, vasodepressor syncope (also known as vasovagal) is the most frequent cause of pediatric syncope (61%–80%). Cardiac disorders only represent 2% to 6% of pediatric cases but account for 85% of sudden death in children and adolescent athletes. 17% of young athletes with sudden death have a history of syncope.
Key features on history and physical examination for identifying high-risk patients include exercise-related symptoms, a family history of sudden death, a history of cardiac disease, an abnormal cardiac examination, or an abnormal ECG.
Category: Critical Care
Posted: 9/25/2012 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
Intubated patients may occasionally meet certain criteria for extubation while in the Emergency Department. Extubation is not without its risk, however, as up to 30% of patients have respiratory distress secondary to laryngeal and upper airway edema, with some patients requiring re-intubation.
Prior to extubation, Intensivists use a brief “cuff-leak” test (deflation of the endotracheal balloon to assess the presence or absence of an air-leak around the tube) to indirectly screen for the presence of upper airway edema and ultimately the risk of re-intubation. The cuff-leak test is performed by deflating the endotracheal balloon followed by one or more of the following maneuvers:
Ochoa et al. performed a systematic review to determine the accuracy of the “cuff-leak” test to predict upper airway edema prior to extubation. The authors concluded that a positive cuff-leak test (i.e., absence of an air-leak) indicates an elevated risk of upper airway obstruction and re-intubation. A negative cuff-leak test (i.e., presence of an air-leak), however, does not reliably exclude the presence of upper airway edema or the need for subsequent re-intubation.
Bottom line: No test prior to extubation reliably predicts the absence of upper airway edema. Patients extubated in the Emergency Department require close observation with airway equipment located nearby.
Ochoa, ME et al. Cuff-leak test for the diagnosis of upper airway obstruction in adults: A systematic review and meta-analysis. Intensive Care Med (2009) 35:1171–1179
Follow me on Twitter @criticalcarenow or Google+ (+Haney Mallemat)
Category: Visual Diagnosis
Posted: 9/24/2012 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
Guide-wires can be challenging to dispose of after central-line insertion because they are difficult to keep on the field, hard to place in the sharps box, and can splash nearby observers.
Click here for this little guide-wire disposal trick.
Follow me on Twitter @criticalcarenow or Google+ (+haney mallemat)
Category: Cardiology
Keywords: Brugada syndrome (PubMed Search)
Posted: 9/23/2012 by Semhar Tewelde, MD
Click here to contact Semhar Tewelde, MD
Mizusawa Y, Wilde A. Brugada Syndrome. Circ Arrhythm Electrophysiol. 2012;5:606-616.
Category: Orthopedics
Keywords: Shoulder, biceps, cartilage tear (PubMed Search)
Posted: 9/22/2012 by Brian Corwell, MD
(Updated: 11/19/2013)
Click here to contact Brian Corwell, MD
SLAP tear/lesion – Superior labral tear anterior to posterior
Glenoid labrum – A rim of fibrocartilaginous tissue surrounding the glenoid rim, deepening the “socket” joint and is integral to shoulder stability
http://www.orthospecmd.com/images/shoulder_labral_tear_anat_02.jpg
Injury is most commonly seen in overhead throwing athletes
Or from a fall on the outstretched hand, a direct shoulder blow or a sudden pull to the shoulder
Sx’s: A dull throbbing pain, a “catching” feeling w/ activity. Some describe clicking or locking of the shoulder. May also include nighttime symptoms. Pain is located to the anterior, superior portion of the shoulder.
Athletes may describe a significant decrease in throwing velocity
http://sitemaker.umich.edu/fm_musculoskeletal_shoulder/o_brien_s_test
Category: Pediatrics
Keywords: premedication, RSI, ventilator, high flow nasal cannula (PubMed Search)
Posted: 9/21/2012 by Mimi Lu, MD
Click here to contact Mimi Lu, MD
Category: Toxicology
Keywords: arsenic, rice (PubMed Search)
Posted: 9/20/2012 by Fermin Barrueto
Click here to contact Fermin Barrueto
Just when you think buying organic protects you from chemicals and pesticide, along comes the studies detecting arsenic in rice products and specficially in organic foods with brown rice organic sweetener. An organic toddler milk formula reportedly had 6x EPA standards for safe drinking water limit.
The more toxic arsenic is the inorganic arsenic which can cause neuropathy but after chronic exposure can cause a classic arsenic keratosis - see attached pic. The inorganic is seen commonly in seafood and is more easily excreted by the body. Unfortunately, in the study referenced here, inorganic As was the predominant type.
Arsenic, organic foods, and brown rice syrup.
Jackson BP, Taylor VF, Karagas MR, Punshon T, Cottingham KL.
Environ Health Perspect. 2012 May;120(5):623-6. Epub 2012 Feb 13.
Category: Critical Care
Posted: 9/18/2012 by Mike Winters, MBA, MD
Click here to contact Mike Winters, MBA, MD
The Lung Transplant Patient in Your ED
Fuehner T, et al. The lung transplant patient in the ICU. Curr Opin Crit Care 2012; 18:472-8.
Category: Visual Diagnosis
Posted: 9/17/2012 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
27 year-old woman with AIDS presents complaining of a painful, puritic, and papular rash. What's the diagnosis?

Answer: Herpes zoster ophthalmicus
Herpes Zoster Ophthalmicus
Follow me on Twitter (@criticalcarenow) or on Google+ (+haney mallemat)
Category: Airway Management
Keywords: Pericarditis (PubMed Search)
Posted: 9/16/2012 by Semhar Tewelde, MD
Click here to contact Semhar Tewelde, MD
Pericarditis is based on clinical diagnosis; typically two of four criteria are found (pleuritic chest pain, pericardial rub, diffuse ST-segment elevation, and pericardial effusion).
Treatment of pericarditis should be targeted at the cause.
Most causes of pericarditis have a good prognosis and are self-limited.
Imazio M. Contemporary management of pericardial diseases. Current Opinion in Cardiology. 27(3):308-17, 2012 May.
Category: Misc
Keywords: CSF, lactate (PubMed Search)
Posted: 9/15/2012 by Michael Bond, MD
Click here to contact Michael Bond, MD
Lactate levels help to confirm septic arthritis but what about bacterial meningitis. As reported in the daily electronic ACEP newsletter a small study of 45 patients showed that all patients with a confirmed diagnosis of bacterial meningitis had a CSF lactate level > 3.5 mmol/L. Therefore, it might be true that viral meningitis will only have CSF lactate levels < 3.5 mmol/L.
With only 45 patients, this finding is clearly not ready for Prime Time but consider adding it to your next CSF study so more data can be collected on the utility of this test.
The story as seen in ACEP eNews on September 14th, 2012 is:
MedPage Today (9/14, Gever) reports, "Cerebrospinal fluid (CSF) levels of lactate were a perfect marker of viral versus bacterial meningitis in a small study, a researcher reported" at the Interscience Conference on Antimicrobial Agents and Chemotherapy. Researchers found that, "among 45 adults in whom the etiology of meningitis was microbiologically confirmed, all those with CSF lactate levels above 3.5 mmol/L had the bacterial form, whereas every patient with lower levels had viral meningitis."
Category: Pediatrics
Posted: 9/15/2012 by Rose Chasm, MD
(Updated: 2/3/2026)
Click here to contact Rose Chasm, MD
Category: Toxicology
Keywords: cyanide, smoke inhalation, enclosed-space fire, carbon monoxide (PubMed Search)
Posted: 9/7/2012 by Bryan Hayes, PharmD
(Updated: 9/13/2012)
Click here to contact Bryan Hayes, PharmD
Carbon monoxide (CO) and hydrogen cyanide (HCN) are two of the main gases causing injury and death from smoke inhalation in fire victims. During the first phase of a fire, and prior to depletion of oxygen reserves and subsequent production of CO, formation of HCN from the thermal breakdown of nitrogen-containing materials may be the primary cause of lethal poisoning in an enclosed-space fire.
A recent, retrospective, observational study from Poland assessed the prevalence of toxic HCN exposure in victims of enclosed-space fires.
Important findings:
Conclusion: The high prevalence of coincident HCN concentrations and COHb levels in victims of enclosed-space fires emphasises the need to suspect HCN as a co-toxin in all persons rescued from fire who show signs and symptoms of respiratory distress.
Grabowska T, et al. Prevalence of hydrogen cyanide and carboxyhaemoglobin in victims of smoke inhalation during enclosed-space fires: a combined toxicological risk. Clin Toxicol 2012;50:759-63.
Follow me on Twitter (@PharmERToxGuy)
Category: Critical Care
Posted: 9/11/2012 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
40 year-old male with severe uncontrolled hypertension presents with altered mental status (head CT below). The CXR is from the same patient. What's the connection?
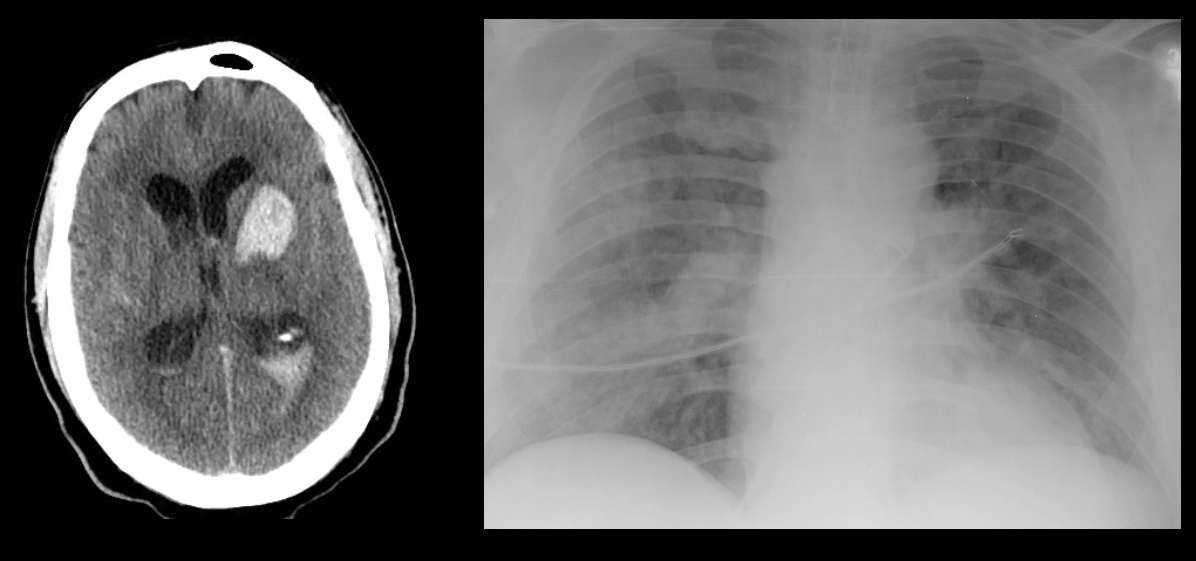
Answer: Neurogenic pulmonary edema (NPE)
NPE is defined as acute pulmonary edema following central nervous system (CNS) insult; NPE has been recognized for over 100 years, but its incidence is underreported due to a lack objective clinical criteria.
The pathophysiology of NPE is poorly understood but it is generally believed that both cardiogenic and non-cardiogenic pulmonary edema play a role. CXR (see above) demonstrates a pattern similar to acute respiratory distress syndrome (i.e., bilateral interstitial infiltrates).
CNS insults that are abrupt, rapidly progressive, and increase intracranial pressure (e.g., subarachnoid hemorrhage, intraparenchymal hemorrhage, traumatic brain injury, subdural, etc.) have the highest risk for NPE. Neural injury leads to sympathetic activation, the release of catecholamines, and one or all of the following:
Treatment of NPE includes:
Davidson, D. et al. Neurogenic pulmonary edema. Crit Care. 2012 Mar 20;16(2):212.
Follow me on Twitter (@criticalcarenow) and Google+ (+haneymallemat)
