Category: Critical Care
Posted: 1/22/2013 by Mike Winters, MBA, MD
Click here to contact Mike Winters, MBA, MD
Postintubation Hypotension
Heffner AC, Swords D, Kline JA, et al. The frequency and significance of postintubation hypotension during emergency airway management. J Crit Care 2012; 27:417e9-417e13.
Heffner AC, Swords D, Nussbaum ML, et al. Predictors of the complication of postintubation hypotension during emergency airway management. J Crit Care 2012; 27:587-593.
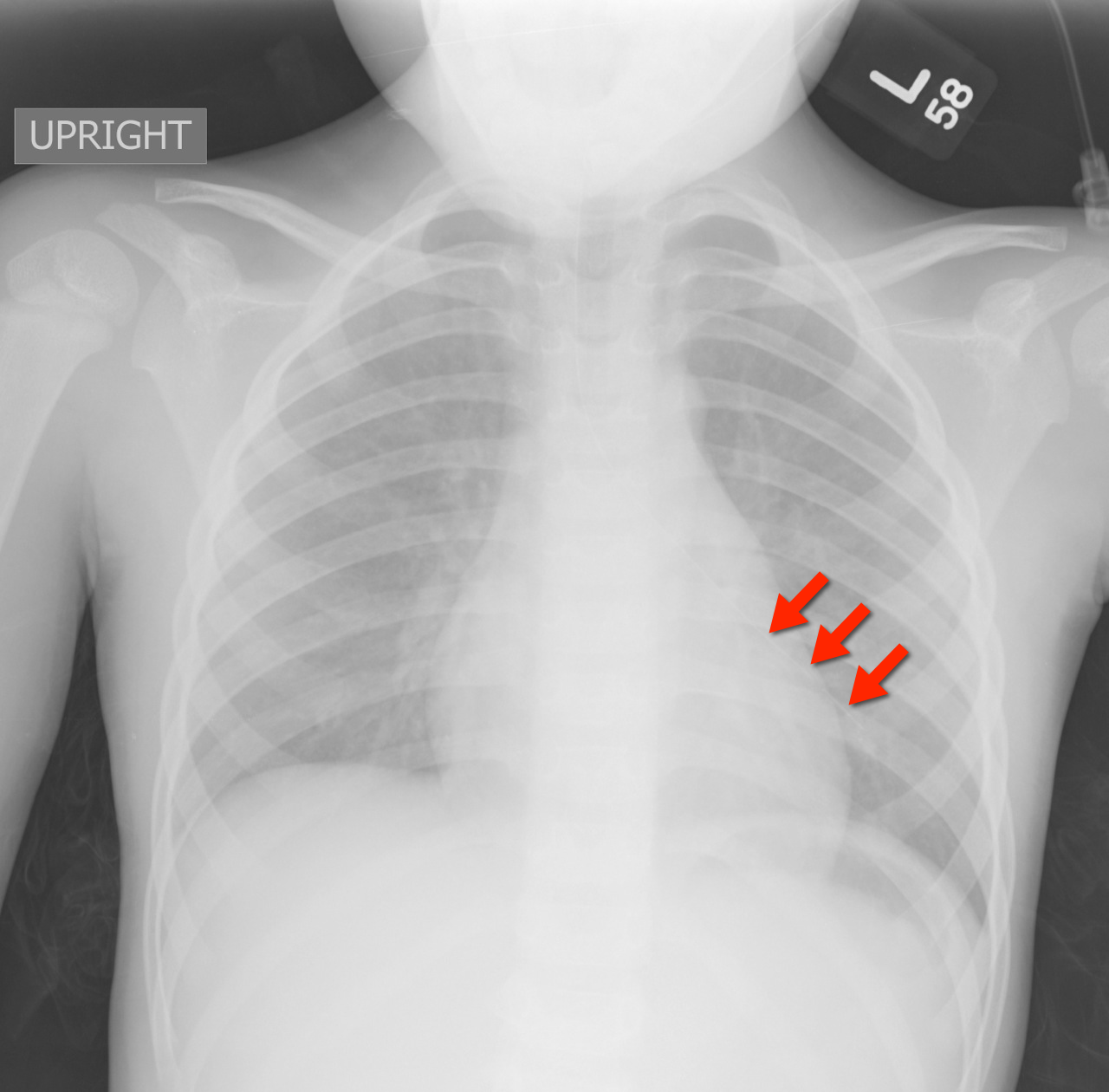
Category: Visual Diagnosis
Posted: 1/21/2013 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
45 year-old male complains of chest pain and cough. He also tells you, "...oh, and by the way doc, I just smoked something." What's the diagnosis?
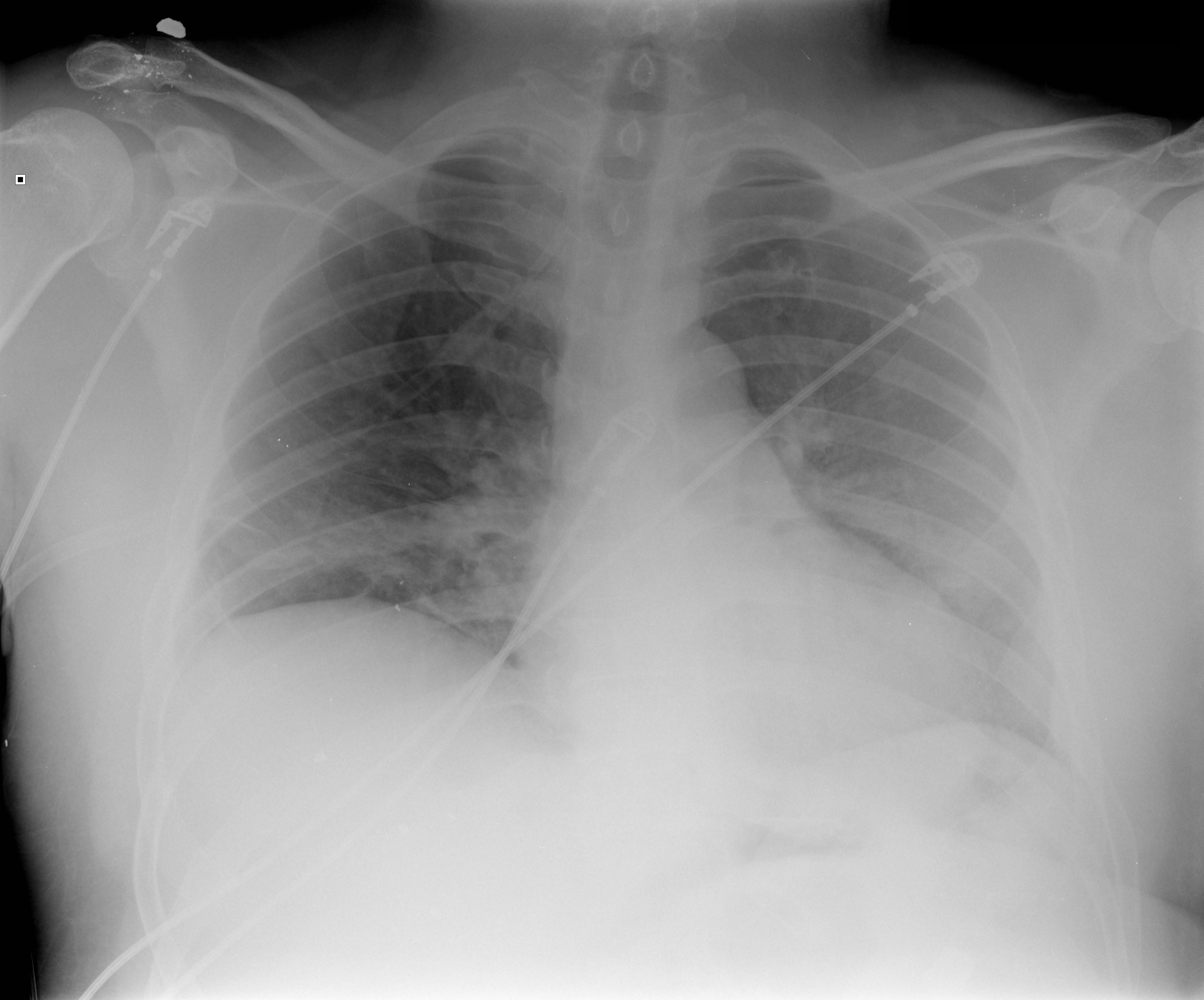
Visual pearls is two years old!!! I want to take this time to thank you all for your support....and now, your answer.
Restrepo, C. et al. Pulmonary complications from cocaine and cocaine-based substances: imaging manifestations. Radiographics. Jul-Aug 2007; 27(4): 941-56
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Cardiology
Posted: 1/20/2013 by Semhar Tewelde, MD
(Updated: 2/3/2026)
Click here to contact Semhar Tewelde, MD
· Cyanosis in the newborn is defined as an arterial saturation <90% and a PO2 <60 torr
· To help differentiate between cardiogenic and non-cardiogenic causes initially obtain an arterial saturation on room air and obtain a subsequent measurements on 100% oxygen
· Infants w/neurogenic or pulmonary causes of cyanosis will demonstrate increases in arterial blood saturation on 100% oxygen while infants with congenital heart disease show minimal elevation
· There are 3 general sources of arterial desaturation in neonates with structural heart disease:
1.) Lesions with decreased pulmonary blood flow (tetralogy of Fallot, severe pulmonary stenosis/atresia, and tricuspid atresia)
2) Admixture lesions, in which desaturated systemic venous blood mixes with intracardiac blood, and then enters the aorta (transposition of great vessels, partial anomalous pulmonary venous drainage)
3) Lesions with increased pulmonary blood flow and pulmonary edema, in which diffusion barriers and intrapulmonary shunting prevent proper oxygenation (truncus arteriosus)
Flanagan MF, Taylor DC, "Cardiac Disease". In Avery GB, Fletcher MA, MacDonald MC, eds. Neonatology. Philadelphia: J.B. Lippincott. 1994:519.
Turley K. Intermediate results from the period of the Congenital Heart Surgeons Society Transposition Study 1985-1989. Ann Thorac Surg. 1995;60:505-510.
Category: Pediatrics
Keywords: magnets, bowel perforation, ischemic necrosis, ingestion (PubMed Search)
Posted: 11/30/2012 by Mimi Lu, MD
(Updated: 1/18/2013)
Click here to contact Mimi Lu, MD
Patient: A 10 year old female is brought to the ED after swallowing 2 beads (see image). Based on the findings, what are your concerns and what is the disposition?
Answer: Multiple Magnet Ingestion
The mother was eventually able to produce the magnetic beads ingested at home 2 hours prior to presentation
The ingestion of multiple magnets is a medical emergency. If the 2 magnets separate and reconnect it can lead to:
- pressure necrosis
- bowel perforation
- fistula formation
- and/or bowel obstruction secondary to kinking, inflammatory reaction, and/or internal herniation
Patients with a multiple magnet ingestion should be taken emergently to the OR for endoscopic evaluation.
If the magnets have passed the pylorus, conservative management with laxatives and serial X-rays may be performed, however if their position becomes fixed on serial imaging then an emergent laparotomy may need to be performed for the removal of the FBs before the symptoms and signs occur.
Bottom line: Patients presenting with a multiple magnet ingestion need to be admitted regardless of the FB location. Consult GI and pediatric surgery early, since prompt removal can prevent devastating outcomes. Single magnet ingestions can be managed conservatively with serial exams and imaging.
Reference:
Alzaham AM et al, Ingested magnets and gastrointestinal complications. Journal of Paediatrics and Child Health; 43 (2007) 497–498.
Category: Toxicology
Keywords: Ssri, Hyponatremia (PubMed Search)
Posted: 1/17/2013 by Fermin Barrueto
(Updated: 2/3/2026)
Click here to contact Fermin Barrueto
SSRIs and SNRIs like venlafaxine and sertraline are well known to cause hyponatremia. Usually considered safe, this adverse drug event can lead to weakness, confusion, seizure and even cerebral edema. Elderly are more susceptible to this adverse effect.
ADH is regulated by serotonin and thus the mechanism for the Hyponatremia is SIADH.
Tolvaptan, a vasopressin receptor antagonist, has been a new treatment that has been used anecdotally in Europe. Waiting for the first US case report.
Meyer I, Frank D, Janssens U.
Dtsch Med Wochenschr. 2012 May;137(21):1096-9. doi: 10.1055/s-0032-1305012. Epub 2012 May 15. German.
[Tolvaptan in antidiuretic hormone secretion syndrome secondary to treatment with citalopram].
Pinal-Fernández I, Segura-García A.
Rev Clin Esp. 2011 Oct;211(9):491-2. doi: 10.1016/j.rce.2011.02.012. Epub 2011 Apr 30. Spanish. No abstract available.
Category: International EM
Posted: 1/16/2013 by Walid Hammad, MD, MBChB
Click here to contact Walid Hammad, MD, MBChB
More than 1.2 billion people are infected with at least one species.
Most helminth infections are contracted by ingesting the eggs, except strongyloides and hookworm whose larvae penetrate bare skin when it is contact with the soil.
The roundworm (Ascaris lumbricoides) life cycle involves migration through the lung tissue which can cause pneumonitis. Patients can present with interstitial infiltrates, wheeze, and blood tinged sputum. Ascaris than migrates to the intestines where it can cause partial small bowel obstruction. In pediatric patients, the appendix may be invaded causing gangrene with symptoms indistinguishable from appendicitis. In adults, the worms can invade the biliary tract and cause biliary disease or pancreatitis. Fever causes this helminth to migrate and it can emerge from the nasopharynx or the anus.
Whipworms (Trichuris trichiura) present as colitis or symptoms similar to inflammatory bowel disease. Chronic illness can involve anemia and clubbing. In severe cases, trichuris can cause dysentery and rectal prolapse.
Hookworms (Necator americanus or Ancylostoma duodenale) also have a pulmonary phase, but with milder symptoms than Ascaris. Eventually hookworms cause iron deficiency anemia and malnutrition. They can be a primary cause of anemia in pregnancy in endemic areas.
Threadworm (Strongyloides stercoralis) can cause a wide spectrum of disease presentations. The infection can start with a rash, larva currens. The infection may be subclinical or may invade the lung, intestinal wall, or the nervous system. Eventually hyperinfection may develop which is a very large increase in worm burden and then the infection becomes disseminated.
Toxocara canis or toxocara cati have affected approximately 14% of the US population. These helminthes reproduce in dogs or cats, and human infection is not part of the normal life cycle. Most infections are subclinical but it can produce a mild pneumonitis that is very similar to asthma. There can be pain and inflammation as the helminthes travel through organs such as the liver or lung and is called visceral larva migrans. The helminth may also move through the eye and optic never causing an ocular form of the disease, ocular larva migrans.
Pinworms (Enterobius vermicularis) are the cause of most common helminth infection in US and can present with anal pruritus leading to trouble sleeping. When an infection is identified, everyone in the household should be treated, regardless of symptoms.
University of Maryland Section of Global Emergency Health
Author: Jenny Reifel Saltzberg, MD, MPH
J Bethony, S Brooker, M Albonico, S M Geiger, A Loukas, D Diemert, P J Hotez. Soil-transmitted helminth infections: ascariasis, trichuriasis, and hookworm. Lancet: 2006; 367: 1521–32.
S Knopp, P Steinmann, J Keiser, J Utzinger. Nematode Infections: Soil-Transmitted Helminths and Trichinella Infect Dis Clin N Am: 2012; 26:341–358.
Category: Critical Care
Posted: 1/15/2013 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
Intra-aortic balloon pumps (IABP) are devices that provide hemodynamic support during cardiogenic shock; the balloon inflates during diastole (improving coronary artery perfusion) and deflates during systole (reducing afterload and improving systemic perfusion). Click here to see a 41 second video illustrating how it works.
Several guidelines recommend placement of an IABP for patients in cardiogenic shock secondary to acute myocardial infarction (AMI), if early revascularization (e.g., CABG) is planned (Class I recommendation). Data behind this recommendation, however, is limited.
The IABP-SHOCK II trial was a randomized, multi-center, open-label study that enrolled 600 patients (598 in the analysis) with cardiogenic shock secondary to AMI (STEMI or NSTEMI). Patients were randomized to the control group (receiving standard therapy; N=298) or the experimental group (receiving IABP; N=300).
No significant difference was found between groups with respect to 30-day mortality (primary end-point), secondary end-points (e.g., time to hemodynamic stabilization, renal function, lactate levels, etc.), or complications (e.g., major bleeding, peripheral ischemic complications, etc.).
Bottom line: Perhaps it is time to reassess the approach to cardiogenic shock secondary to AMI when early revascularization is planned. At this time consultation with local expertise is recommended.
Category: Cardiology
Keywords: VAD (PubMed Search)
Posted: 1/13/2013 by Semhar Tewelde, MD
Click here to contact Semhar Tewelde, MD
Klein T, Jacob M. Management of Implantable Assisted Circulation Devices. Cardiology Clinics. 2012;30(4):673-682.
Category: Orthopedics
Keywords: head injury, concussion, return to play (PubMed Search)
Posted: 1/12/2013 by Brian Corwell, MD
(Updated: 2/3/2026)
Click here to contact Brian Corwell, MD
"When can my child get back out on the field doc?"
Return to play
▸ Concussion symptoms should be resolved before returning to exercise.
▸ A RTP progression involves a gradual, step-wise increase in physical
demands, sports-specific activities and the risk for contact.
▸ If symptoms occur with activity, the progression should be halted and
restarted at the preceding symptom-free step.
▸ RTP after concussion should occur only with medical clearance from a
licenced healthcare provider trained in the evaluation and management
of concussions.
Short-term risks of premature RTP
▸ The primary concern with early RTP is decreased reaction time leading
to an increased risk of a repeat concussion or other injury and
prolongation of symptoms.
Long-term effects
▸ There is an increasing concern that head impact exposure and
recurrent concussions contribute to long-term neurological sequelae.
▸ Some studies have suggested an association between prior concussions
and chronic cognitive dysfunction. Large-scale epidemiological studies are
needed to more clearly define risk factors and causation of any long-term
neurological impairment.
American Medical Society for Sports Medicine
position statement: concussion in sport, 2013
Category: Pediatrics
Posted: 1/11/2013 by Rose Chasm, MD
(Updated: 2/3/2026)
Click here to contact Rose Chasm, MD
CDC MMWR 1/2011
FDA 12/2012
Category: Toxicology
Keywords: tapentadol, methadone, false positive, urine toxicology (PubMed Search)
Posted: 1/7/2013 by Bryan Hayes, PharmD
(Updated: 1/10/2013)
Click here to contact Bryan Hayes, PharmD
Several medications can produce a false-positive result for methadone on the urine drug screen: diphenhydramine, doxylamine, clomipramine, chlorpromazine, quetiapine, thioridazine, and verapamil.
Add a new one to the list. Tapentadol, a relatively new opioid analgesic similar to tramadol, can also produce a false-positive result for methadone on certain immunoassays.
A separate study concluded that tapentadol does not affect the amphetamine screen.
Brahm NC, Yeager LL, Fox MD, et al. Commonly prescribed medications and potential false-positive urine drug screens. Am J Health Syst Pharm 2010;67(16):1344-50. [PMID 20689123]
Collins AA, Merritt AP, Bourland JA. Cross-reactivity of tapentadol specimens with DRI methadone enzyme immunoassay. J Anal Toxicol 2012;36(8):582-7. [PMID 22879537]
Tang S, Mullins ME, Braun BM, et al. Can tapentadol cause a false-positive urine drug screen for amphetamine? Clin Toxicol 2012;50(10):1174-5. [PMID 23088194]
Follow me on Twitter (@PharmERToxGuy)
Category: Visual Diagnosis
Keywords: spinal, international, tuberculosis, scoliosis, kyphosis, pulmonary, neurologic (PubMed Search)
Posted: 1/9/2013 by Andrea Tenner, MD
Click here to contact Andrea Tenner, MD
These two Ethiopian boys present with “back problems”. What are the diagnoses and what do you need to worry about with each of them?
The boy on the left has spinal tuberculosis (Pott's Disease) while the one on the right has severe scoliosis.
Pott's Disease:
Severe Scoliosis:
Bottom Line:
Spinal tuberculosis most commonly causes anterioposterior (AP) deformity and can cause severe neurologic deficits. Anti-TB medication is needed for treatment.
Severe scoliosis involves lateral as well as AP deformity and can cause severe pulmonary dysfunction.
University of Maryland Section of Global Emergency Health
Author: Andi Tenner, MD, MPH
Center for Disease Control and Prevention. Guidelines for Preventing the Transmission of Mycobacerium tuberculosis in Health-Care Settings. MMWR 2005;54(No. RR-17):1-144.
Koumbourlis AC. Scoliosis and the respiratory System. Paediatric Respiratory Reviews 2006;7:152-160.
Turgut M. Spinal tuberculosis (Pott’s disease): its clinical presentation, surgical management, and outcome. A survey study on 694 patients. Neurosurg Rev 2001;24:8-13.
Category: Critical Care
Posted: 1/8/2013 by Mike Winters, MBA, MD
Click here to contact Mike Winters, MBA, MD
The Crashing Cardiac Transplant Patient
Chacko P, Philip S. Emergency department presentation of heart transplant recipients with acute heart failure. Heart Failure Clinics 2009; 5:129-143.
Costanzo MR, et al. The International Society of Heart and Lung Transplantation Guidelines for the care of heart transplant recipients. J Heart Lung Transplant 2010; 29:914.956.
Category: Visual Diagnosis
Posted: 1/7/2013 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
4 year-old female with the post-procedural CXR shown below. What's the diagnosis? (Hint: use the zoom...this one is tricky)
Answer: Nasogastric tube in the left mainstem bronchus. Patient was asymptomatic but ironically bubbling was heard when air was injected into the NG tube.
Nasogastric tube (NGT) pearls
The risk of NGT misplacement is 4% in adults, but is 21-43% in children.
Risk factors for misplacement are:
The ability to aspirate gastric contents, pH testing of the aspirated fluid, and the auscultation of “bubbling” over the epigastrium have all been suggested as reliable methods to confirm proper placement; unfortunately, they are often unreliable.
Visualization of the NGT by X-ray is the only way to be 100% certain of placement.
The risks of misplacement include pneumonia and pneumothorax.
Farrington et al. Nasogastric tube placement verification in pediatric and neonatal patients. Pediatric Nursing. Jan-Feb 2009. Vol 35. Issue 1.
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Cardiology
Posted: 1/6/2013 by Semhar Tewelde, MD
(Updated: 2/3/2026)
Click here to contact Semhar Tewelde, MD
Bock J, Benitez M. Blunt Cardiac Injury. Cardiology Clinics. 2012;30(4):545-55.
Category: Pharmacology & Therapeutics
Keywords: Tdap, tetanus, immunization, vaccine, pertussis (PubMed Search)
Posted: 1/3/2013 by Bryan Hayes, PharmD
(Updated: 1/5/2013)
Click here to contact Bryan Hayes, PharmD
The two available Tetanus/reduced diphtheria toxoid/acellular pertussis (Tdap) vaccine products in the U.S. are Boostrix and Adacel. Neither were originally approved in older adults age 65 and older. Boostrix received FDA-approval for use in this age group in July 2011, but Adacel never has.
However, in June 2012 ACIP issued new guidance recommending Tdap for all adults age 65 years and older.
"When feasible, Boostrix should be used for adults aged 65 years and older; however, ACIP concluded that either vaccine administered to a person 65 years or older is immunogenic and would provide protection. A dose of either vaccine may be considered valid."
Bottom line: Regardless of which Tdap product is stocked at your institution, both are considered safe to use in adults 65 years and older.
Centers for Disease Control and Prevention (CDC), “Updated Recommendations for Use of Tetanus Toxoid, Reduced Diphtheria Toxoid, and Acellular Pertussis (Tdap) Vaccine in Adults Aged 65 Years and Older - Advisory Committee on Immunization Practices (ACIP)," MMWR Morb Mortal Wkly Rep, 2012, 61(25):468-70. [PMID 22739778]
Follow me on Twitter (@PharmERToxGuy)
Category: Pediatrics
Posted: 1/4/2013 by Lauren Rice, MD
(Updated: 2/3/2026)
Click here to contact Lauren Rice, MD
Rotavirus is the leading cause of gastroenteritis worldwide and a leading cause of infant death in the developing world.
95% of U.S. children have had a rotavirus infection by the age of 5 years.
Most cases occur in late winter and early spring.
Route of transmission is mostly fecal-oral but may be airborne in cooler months.
Most common presenting signs and symptoms include fever (1/3 of cases), vomiting (in the first 1-2 days), and diarrhea (copious, watery, lasting 5-21 days).
Diagnosis is largely based on clinical manifestations, but antigen assays are available and may be useful in patients with extraintestinal complications, such as hepatitis, pneumonitis, or encephalopathy.
Treatment is largely supportive with efforts to maintain hydration.
Prevention is key to disease control and accomplished with good hand hygiene and widespread vaccination.
Newly implemented vaccine programs worldwide have proven to be effective in decreasing hospitalizations and deaths in developing countries.
Cox, Elaine and Christenson, John. Rotavirus. Pediatrics in Review. 2012; 33 (10): 439 - 447.
Category: Toxicology
Keywords: creatine, supplement, weight lifting (PubMed Search)
Posted: 1/3/2013 by Ellen Lemkin, MD, PharmD
(Updated: 2/3/2026)
Click here to contact Ellen Lemkin, MD, PharmD
Creatine
Adverse effects: weight gain, edema, GI cramping, fatigue and diarrhea
Dandoy C, Gereige RS. Performance-Enhancing Drugs. Pediatrics in Review June 2012;33(6):265-72.
Category: International EM
Keywords: Leptospirosis, Baltimore, jaundice, thrombocytopenia, international, tropical (PubMed Search)
Posted: 1/2/2013 by Andrea Tenner, MD
Click here to contact Andrea Tenner, MD
General Information:
-Leptospirosis is a tropical infectious disease that is also endemic in the US. (Estimated 16% seroprevalence in inner city Baltimore!)
-The spirochete is spread through animal urine and can survive in water or soil for weeks.
-Risk factors: rural exposure to animal urine (farming, adventure sports) or urban exposure to rat urine.
-Infection is acquired through breaks in the skin or mucus membranes
-Outbreaks are often seen following rain or floods.
Clinical Presentation:
-Non-specific febrile illness (usually not diagnosed in these cases)
-If untreated, 5-10% progress to jaundice, renal failure, thrombocytopenia, hemorrhage, and respiratory failure.
Diagnosis:
- Primarily based on clinical presentation and history
- Paired serum sent to CDC (the acute serum sample should be drawn in the ED)
Treatment:
- Doxycycline, Ceftriaxone and Penicillin are all effective
Bottom Line:
Consider and treat for Leptospirosis in patients with possible exposure animal urine (especially after a flood) who present in extremis with renal failure, jaundice, and thrombocytopenia.
University of Maryland Section of Global Emergency Health
Author: Andi Tenner, MD, MPH
Center for Disease Control. (2012) Leptospirosis. Retrieved January 1, 2013 from http://www.cdc.gov/leptospirosis/infection/index.html.
Childs JE, Schwartz BS, Ksiazek TG, et al. Risk Factors Associated with Antibodies to Leptospires in Inner-city Residents of Baltimore: A Protective Role for Cats. Am J Public Health. 1992;82:597-599.
Leung J, Schiffer J. Feverish, Jaundiced. Am J Med. 2009;122:129-131.
Category: Critical Care
Posted: 1/1/2013 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
DRESS (Drug Reaction with Eosinophilia and Systemic Symptoms) or DIHS (Drug-Induced Hypersensitivity Syndrome) is a potentially life-threatening adverse drug-reaction.
Incidence is 1/1,000 to 1/10,00 drug exposures. It occurs 2-6 weeks after the drug is first introduced, distinguishing it from other adverse drug-reactions which typically occur sooner.
The syndrome classically includes:
The most commonly implicated drugs are anticonvulsants (e.g., carbamazepine, phenobarbital, and phenytoin), sulfonamides, and allopurinol.
Recovery is typically complete after discontinuing the offending drug; systemic steroids may promote resolution of the illness.
Cacoub P. et al. The DRESS syndrome: a literature review. Am J Med 2011 Jul;124(7):588-97. http://www.ncbi.nlm.nih.gov/pubmed/21592453
Follow me on Twitter (@criticalcarenow) or on Google+ (+criticalcarenow)
