Category: Visual Diagnosis
Posted: 12/10/2012 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
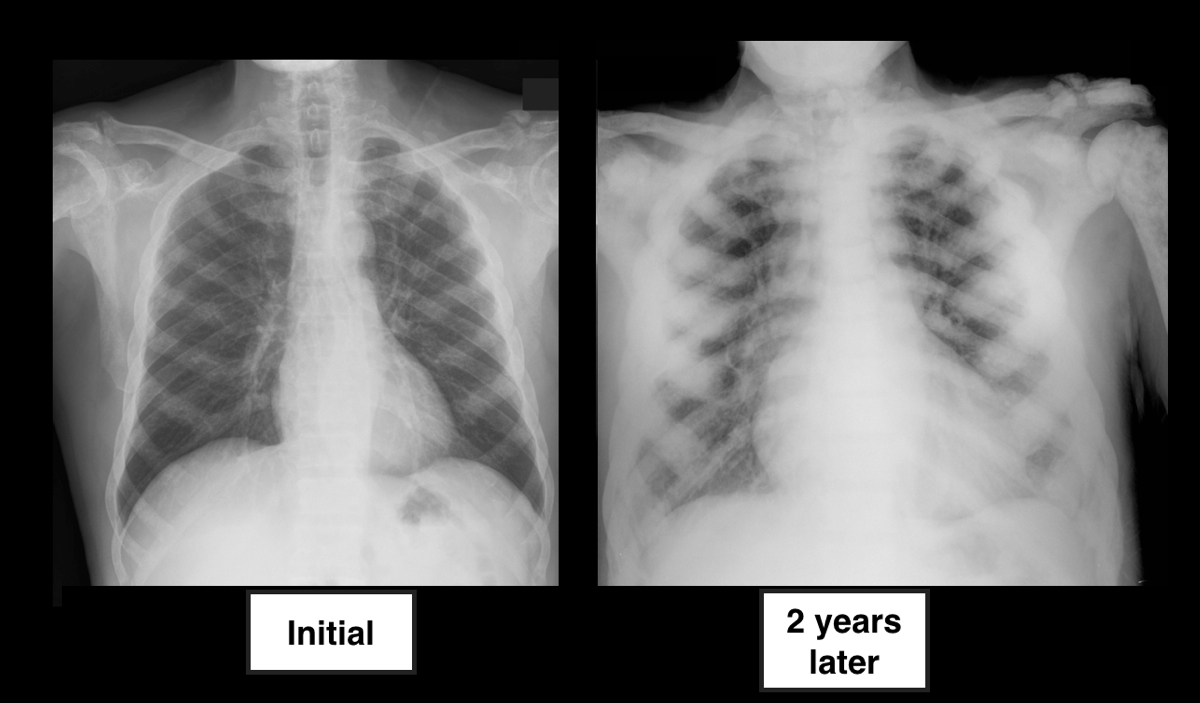
64 year-old male with no past medical history presents complaining of chronic weight-loss and diffuse chest pain; CXR is shown below. What's the diagnosis, and what other disease(s) may present this way?

Answer: Sclerotic bone (osteoblastic) metastasis secondary to prostate cancer. The patient's CXR from 2 years prior is shown below for comparison.
Other malignancies associated with osteoblastic metastasis:
Follow me on Twitter (@criticalcarenow) or on Google+ (+haney mallemat)
Category: Cardiology
Posted: 12/8/2012 by Semhar Tewelde, MD
Click here to contact Semhar Tewelde, MD
Hijazi K. Coarctation of the aorta: From fetal life to adulthood. Cardiology Journal. 18(5):487-95, 2011
Category: Orthopedics
Keywords: pneumonia, rib fracture, blunt chest trauma (PubMed Search)
Posted: 12/7/2012 by Brian Corwell, MD
Click here to contact Brian Corwell, MD
Are discharged patients who suffer minor thoracic injury at risk of developing delayed pneumonia?
Prospective study of 1,057 patients age 16 and older with minor thoracic injury who were discharged from the ED.
32.8% had at least one rib fracture
8.2% had asthma
3.4% had COPD
Only 6 patients developed pneumonia!!
Sex, smoking, atelectasis on CXR, and alcohol intoxication were not significantly associated with delayed pneumonia.
However, for patients with preexistent pulmonary disease (asthma or COPD) AND rib fracture, the relative risk of delayed pneumonia was 8.6. Patients without either of these conditions are at extremely low risk of future development of pneumonia.
Patients with rib fractures do not develop delayed pneumonia: a prospective, multicenter cohort study of minor thoracic injury. Chauny JM, Emond M, Plourde M, Guimont C, Le Sage N, Vanier L, Bergeron E, Dufresne M, Allain-Boulé N, Fratu R. Ann Emerg Med. 2012 Dec;60(6):726-31.
Category: Pediatrics
Posted: 12/7/2012 by Jenny Guyther, MD
Click here to contact Jenny Guyther, MD
Epidemiology:
Trampoline injuries doubled between 1991 and 1996, increasing from 39,000 injuries per year to more then 83,000 injuries per year. Injury rates and trampoline sales peaked in 2004 and have been decreasing since; however, hospitalization rates are still between 3% and 14%.
Risk Factors:
¾ of injuries occur when multiple people are on the trampoline at once
Smaller participants were 14x more likely to be injured then their heavier playmates
Falls account for 27-39% of all injuries
Springs and frames account for 20% of injuries
Up to ½ of injuries occur despite adult supervision
Injury types:
Lower extremity injuries are more common than upper extremity
Head and neck injuries accounted for 10-17% of trampoline injuries
Unique Injuries:
Proximal tibial fractures
Manubriosternal dislocations and sternal injuries
Vertebral artery dissection
Atlanto-axial subluxation
Trampoline Saftey in Childhood and Adolescence. Pediatrics 2012; 130; 774-779.
Category: Critical Care
Keywords: anaphylaxis, tryptase, diagnosis (PubMed Search)
Posted: 12/6/2012 by Ellen Lemkin, MD, PharmD
(Updated: 2/3/2026)
Click here to contact Ellen Lemkin, MD, PharmD
Simons EF, Ardusso LE, Bilo MB, et al. 2012 Update: World Allergy Organization Guidelines for the assessment and management of anaphylaxis.
Category: Airway Management
Posted: 12/5/2012 by Walid Hammad, MD, MBChB
(Updated: 2/3/2026)
Click here to contact Walid Hammad, MD, MBChB
40 yo previously healthy male in China who presents with prolonged “seizure” after receiving a cut on his foot while fishing 5 days ago.
Dx: Tetanus
Clinical features:
· Incubation period 4-14 days
· 3 clinical forms:
1. Local spasm
2. Cephalic (rare) - cranial nerve involvement
3. Generalized (most common) - Descending spasm: facial sneer (risus sardonicus), “locked jaw” trismus, neck stiffness, laryngeal spasm, abdominal muscle spasm.
· Spasms continue to 3-4 weeks and can take months to fully recover
Complications: apnea, rhabodymyolysis, fracture/dislocations
Treatment: supportive, benzodiazepines, RSI, Tetanus IG (3000-5000 units IM), wound debridement
University of Maryland Section for Global Emergency Health
Author: Veronica Pei, MD
Category: Visual Diagnosis
Posted: 12/4/2012 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
An 86 year-old nursing home resident presents to the ED with a urinary tract infection, four days after discharge from the inpatient service for the same diagnosis. She was discharged from the inpatient service with a prescription for ciprofloxacin to be given through her gastric feeding tube (she does not take anything orally). Could her tube feeds be playing a role in the relapse of her urinary tract infection?
Answer: Ciprofloxacin was not being properly absorbed secondary to enteral tube feeding.
Fluoroquinolones administered via enteral feeding tubes may have reduced efficacy and patient outcomes when given to patients simultaneously receiving tube feeds (e.g., PEG tube feeding).
The reduction in antimicrobial efficacy may be due to improper peak drug concentrations and variability in time to peak serum levels. Studies have demonstrated the bioavailability of Ciprofloxacin varies from 31-82% in patients receiving continuous enteral feeds.
The exact mechanism(s) responsible for the altered pharmokinetics are not completely understood but may involve the binding of divalent cations in the enteral feeds by fluoroquinolones, reducing its absorption and efficacy.
Clinicians should properly educate people who will be administering fluoroquinolones to the patient (e.g., nursing home staff, family, etc.). It is recommended that fluoroquinolones be given:
Perhaps easiest of all, is to consider discharging patients with a prescription for parenterally administered antibiotics for the duration of the infection.
Beckwith MF, Feddema SS, Barton RG, Graves C. A guide to drug therapy in patients with enteral feeding tubes: Dosage form selection and administration methods. Hosp Pharm. 2004;39:225–37
Follow me on Twitter (@criticalcarenow) or Google+ (+haney mallemat)
Category: Visual Diagnosis
Posted: 12/2/2012 by Haney Mallemat, MD
(Updated: 12/3/2012)
Click here to contact Haney Mallemat, MD
11 year-old boy presents with right knee pain and swelling after falling off of his bicycle. What's the diagnosis?
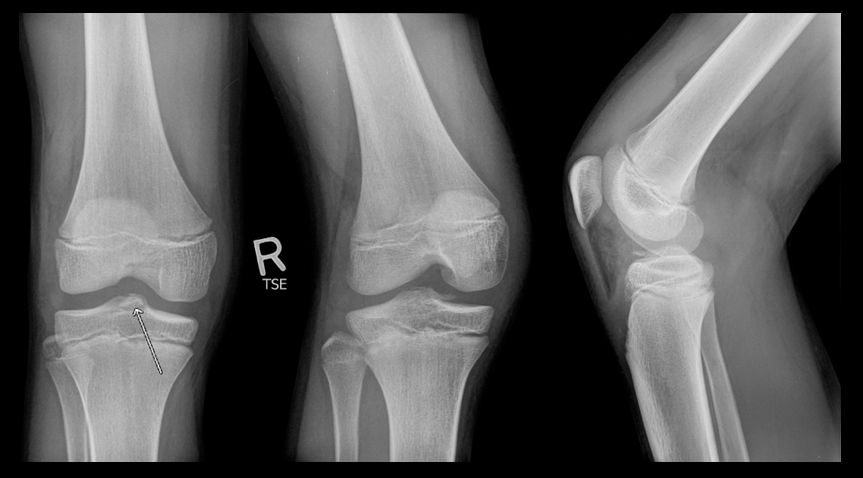
Answer: Fracture of the intercondylar eminence of the tibia; Meyers & McKeever Grade II (grading system described below)
Intercondylar Eminence Fracture
Reference: Tudisco, C., et al Intercondylar eminence avulsion fracture in children: long-term follow-up of 14 cases at the end of skeletal growth, J Pediatr Orthop B 19:403–408 c 2010
Follow me on Twitter (@criticalcarenow) or Google+ (+haney mallemat)
Category: Cardiology
Keywords: Kawasaki Disease, Mucocutaneous lymph node syndrome (PubMed Search)
Posted: 12/2/2012 by Semhar Tewelde, MD
(Updated: 2/3/2026)
Click here to contact Semhar Tewelde, MD
Scuccimarri R. Kawasaki Disease. Pediatric Clin N Am 59(2012)425-445
Category: Pharmacology & Therapeutics
Keywords: doxycycline, PID, pelvic inflammatory disease, STD, azithromycin (PubMed Search)
Posted: 11/28/2012 by Bryan Hayes, PharmD
(Updated: 12/1/2012)
Click here to contact Bryan Hayes, PharmD
In the rare circumstance you need to treat a patient with suspected PID and an allergy to doxycycline, what is the alternative?
For oral regimens, azithromycin is an option in place of doxycycline.
Suggested regimen for PID with doxycycline allergy:
Bevan CD, Ridgway GL, Rothermel CD. Efficacy and safety of azithromycin as monotherapy or combined with metronidazole compared with two standard multidrug regimens for the treatment of acute pelvic inflammatory disease. J Int Med Res 2003;31:45–54.
Savaris RF, Teixeira LM, Torres TG, et al. Comparing ceftriaxone plus azithromycin or doxycycline for pelvic inflammatory disease: a randomized controlled trial. Obstet Gynecol 2007;110:53–60.
Follow me on Twitter (@PharmERToxGuy)
Category: Toxicology
Keywords: CT, carbon monoxide, cyanide (PubMed Search)
Posted: 11/29/2012 by Fermin Barrueto
(Updated: 2/3/2026)
Click here to contact Fermin Barrueto
It is not often that a CT will be able to give you a hint to a toxicologic diagnosis. The following are CT findings that are either suggestive and even sometimes almost diagnostic for a given to toxin:
1) Intraparenchymal or Subarachnoid Hemorrhage: sympathomimetics or mycotic anuerysm rupture secondary to IV drug abuse
2) Basal Ganglia bilateral focal necrosis: characteristic of carbon monoxide, cyanide, hydrogen sulfide and even methanol
3) Severe advanced atrophy out of proportion for age: alcoholism, toluene
Adapted from Goldfranks Textbook of Toxicologic Emergencies 8th edition, p.82 Table 6-5.
Category: International EM
Keywords: water, international, cryptopsporidium, chlorine, iodine, boiling (PubMed Search)
Posted: 11/28/2012 by Andrea Tenner, MD
Click here to contact Andrea Tenner, MD
General Information:
• Millions of people around the world (including our patients who travel and victims of disasters like Hurricane Sandy) are exposed to non-potable water.
• How to treat contaminated water:
♦ Filter cloudy water through a clean cloth or allow to settle prior to treatment
♦ The safest method is boiling water vigorously for 1 minute (or, at least 3 minutes at altitudes >6,000ft)
♦ Chemical disinfection is not as effective but, if boiling is not possible, use either:
• 2 drops of unscented bleach (5.52% Cl) per quart/liter of water. (Unknown strength? Add 10 drops per quart/liter.)
-Or-
• 5 drops of tincture of 2% iodine per quart/liter.
- If the water is cloudy or cold, double the chlorine or iodine.
- Notes: Pregnant women or people with thyroid conditions should not use iodine
♦ UV decontamination can be accomplished by leaving clear bottles of water in direct sun for >6 hours or special equipment, but requires clear water
• Boiling, Chlorine/Iodine, and UV will kill viruses, bacteria, and Giardia
• Only Boiling kills Cryptosporidium
Bottom Line:
• If bottled water is available, use it.
• If not, boil your water.
• In order to treat for a wide variety of pathogens, it is best to combine available methods.
University of Maryland Section for Global Emergency Health
Author: Andi Tenner
United States Environmental Protection Agency. Water Health Series: Filtration Facts. 2005. http://water.epa.gov/drink/info/upload/2005_11_17_faq_fs_healthseries_filtration.pdf
United States Environmental Protection Agenecy. Emergency Disinfection of Drinking Water. 2006. http://water.epa.gov/drink/emerprep/emergencydisinfection.cfm .
United States Center for Disease Control. Water Treatment Methods. 2011. http://wwwnc.cdc.gov/travel/page/water-treatment.htm.
Category: Critical Care
Posted: 11/27/2012 by Mike Winters, MBA, MD
(Updated: 2/3/2026)
Click here to contact Mike Winters, MBA, MD
Managing Critically Ill Patients with AKI
Brienza N, et al. Protocoled resuscitation and the prevention of acute kidney injury. Curr Opin Crit Care 2012; 18:613-622.
Kidney Disease: Improving Global Outcomes (KDIGO) Acute Kidney Injury Work Group. KDIGO Clinical Practice Guideline for Acute Kidney Injury. Kidney Int 2012; 2(S):1-138.
Category: Visual Diagnosis
Posted: 11/25/2012 by Haney Mallemat, MD
(Updated: 11/26/2012)
Click here to contact Haney Mallemat, MD
2 year-old male with past medical history of asthma presents with fever and respiratory distress. CXR is shown below. What’s the diagnosis? (Hint: ...look beyond the obvious)

Answer #1: Multifocal opacities predominantly in left lower lobe representing pneumonia
Answer #2 Healing left-sided rib fractures involving the lateral aspects of ribs 8 through 10th suspicious for non-accidental trauma (see X-ray below)
Pediatric CXR pearls
Bottom line: Screen patients for the above risk factors when rib fractures have been identified, but always think of abuse and the child’s safety first….and don’t forget to thoroughly examine radiology despite finding one abnormal finding.

Reference: Cosway et al. Diagnostic indicators for NAI in children with rib fractures: A retrospective study. Arch Dis Child 2011; 96 (supplement)
Follow me on Twitter (@criticalcarenow) or Google+ (+Haney Mallemat)
Category: Cardiology
Keywords: Rheumatic fever, rheumatic heart disease (PubMed Search)
Posted: 11/25/2012 by Semhar Tewelde, MD
(Updated: 2/3/2026)
Click here to contact Semhar Tewelde, MD
Marijon E. Mirabel M. Celermajer DS. Jouven X. Rheumatic heart disease. Lancet. 379(9819):953-64, 2012 Mar 10.
Category: Orthopedics
Keywords: hematoma blocks, fracture analgesia (PubMed Search)
Posted: 11/24/2012 by Brian Corwell, MD
Click here to contact Brian Corwell, MD
Hematoma blocks for distal radius fractures
Hematoma blocks provide safe, effective analgesia without an increased risk of post procedural infections when compared with other regional blocks
Provide equal reduction quality AND pain control as procedural sedation with Propofol.
However, mean time to reduction (0.9 vs. 2.6 hours) and time to discharge post procedure (0.74 vs. 1.17 hours) were reduced with hematoma blocks.
Consider this option next time the department is busy or the patient is not an ideal procedural sedation candidate.
Emiley P, Schreier S and Pryor P. Hematoma Blocks for Reduction of Distal Radius Fractures. Emergency Physicians Monthly. September 2012. 16-17.
Category: International EM
Keywords: malaria, Plasmodium, falciparum, quinine, international, fever (PubMed Search)
Posted: 11/21/2012 by Andrea Tenner, MD
(Updated: 2/3/2026)
Click here to contact Andrea Tenner, MD
University of Maryland Section for Global Emergency Health
Author: Emilie J.B. Calvello, MD, MPH
Center for Disease Control. (2012). Malaria. Retrieved November 9, 2012, from http://www.cdc.gov/MALARIA/
Wattal, C. et al. Infectious disease emergencies in returning travelers: special referece to malaria, dengue and chikungunya. Med Clin North Am. 2012 Nov; 96(6): 1225 – 55.
Category: Critical Care
Posted: 11/20/2012 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
A low-tidal volume (or protective) strategy of mechanical ventilation (i.e., tidal volume of 6-8cc/kg of ideal body weight) has previously been demonstrated to be beneficial in patients with acute respiratory distress syndrome (ARDS).
A meta-analysis was recently performed to determine whether this strategy of mechanical ventilation is also beneficial for patients without lung injury prior to initiation of mechanical ventilation.
Dr. Neto, et al. performed a meta-analysis of 20 studies (total of 2,822 mechanically ventilated patients) comparing a conventional ventilation strategy (average tidal volume was 10.6 cc/kg) to a protective ventilation strategy (average tidal volume was 6.4 cc/kg) of mechanical ventilation.
The authors concluded that patients ventilated with a protective lung-strategy had reductions in:
Bottom-line: This meta-analysis supports the notion that a strategy of low-tidal volume ventilation may have benefits for patients without ARDS, however prospective studies are needed.
Neto, S. et al. Association between use of lung-protective ventilation with lower tidal volumes and clinical outcomes among patients without acute respiratory distress syndrome. JAMA, Oct. 24/31; 308;16.
Follow me on Twitter (@criticalcarenow) or Google+ (+haney mallemat)
Category: Visual Diagnosis
Posted: 11/19/2012 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
Do you like placing ultrasound-guided IV catheters? Check out this trick for covering the probe during the procedure.
http://ultrarounds.com/Ultrarounds/The_Vascular_Probe_Protector.html
or
https://www.youtube.com/watch?v=ZuOq6Ea_FbA&feature=plcp
Follow me on Twitter (@criticalcarenow) or Google+ (+haney mallemat)
Category: Cardiology
Keywords: Torsades de pointes, prolonged QT syndrome (PubMed Search)
Posted: 11/18/2012 by Semhar Tewelde, MD
Click here to contact Semhar Tewelde, MD
Congenital and Acquired Long QT Syndrome.Cardiology in Review. 12(4):222-34, 2004 Jul-Aug.
