Category: Cardiology
Posted: 3/30/2013 by Semhar Tewelde, MD
(Updated: 2/3/2026)
Click here to contact Semhar Tewelde, MD
Category: Orthopedics
Keywords: Ottawa, Knee, Pittsburgh (PubMed Search)
Posted: 3/30/2013 by Michael Bond, MD
Click here to contact Michael Bond, MD
Knee Pain Injuries are Radiographs needed?
Many people know that the folks in Ottawa have come up with a rule to determine whether radiographs are needed in patients complaining of knee pain. The Ottawa Knee rules that that radiographs are only required for knee injuries with any of the following:
• Age 55 years or older
• isolated tenderness of patella
• tenderness at head of fibula
• inability to flex to 90'
• inability to bear weight both immediately and in the emergency department (4 steps)
Well another group in Pittsburgh have their own set of rules that were recently shown to be more specific with equal sensitivity. The Pittsburgh decision rules state that radiographs are only needed if
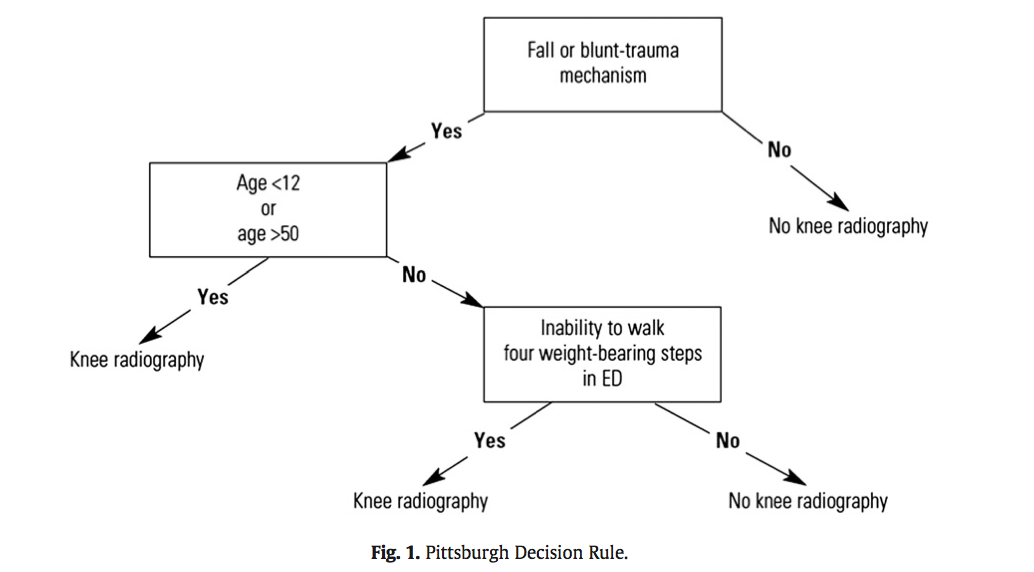
So consider using the Pittsburgh or Ottawa Knee rules the next time you have a patient with knee pain to determine if those radiographs are really needed.
The full article can be found at http://www.ajemjournal.com/article/S0735-6757%2812%2900566-9/abstract
Cheung TC, Tank Y, Breederveld RS, Tuinebreijer WE, de Lange-de Klerk ESM, MD RJD. Diagnostic accuracy and reproducibility of the Ottawa Knee Rule vs the Pittsburgh Decision Rule. Am J Emerg Med. Elsevier Inc; 2013 Feb 1;:1–5.
Category: Pediatrics
Posted: 3/29/2013 by Mimi Lu, MD
Click here to contact Mimi Lu, MD
You have diagnosed an infant or child with pneumonia. How do you decide if they need admission?
The Pediatric Infectious Disease Society and the British Thoracic Society each have guidelines from 2011 to help with this decision.
Category: International EM
Posted: 3/28/2013 by Walid Hammad, MD, MBChB
(Updated: 2/3/2026)
Click here to contact Walid Hammad, MD, MBChB
Background Information:
Combination antiretroviral therapy (cART) reduces HIV-associated morbidities and mortalities but cannot cure infection. Recent literature has suggested that early initiation of cART with primary infection can lead to “functional cure” for HIV infected patients with suppressed viremia and delayed progression to clinical symptoms.
Pertinent Study Design and Conclusions:
- Researchers studied 14 patients whose treatment with combination antiretrovirals began soon after exposure to HIV. The patients' viral loads became undetectable within roughly 3 months, and treatment was interrupted after about 3 years.
- The patients were found to have very low viral loads and stable CD4-cell counts after several years without therapy. The researchers estimate that about 15% of those treated early could achieve similar results.
Bottom Line:
Have a high suspicion of acute anti-retroviral syndrome in the ED (fever, rash, pharyngitis, lymphadenopathy) and test properly (viral load NOT ELISA) to identify patients who may benefit from early, rapid initiation of cART.
University of Maryland Section of Global Emergency Health
Author: Emilie J. B. Calvello, MD, MPH
Sáez-Cirión A, Bacchus C, Hocqueloux L, Avettand-Fenoel V, Girault I, et al. (2013) Post-Treatment HIV-1 Controllers with a Long-Term Virological Remission after the Interruption of Early Initiated Antiretroviral Therapy ANRS VISCONTI Study. PLoS Pathog 9(3): e1003211.
Category: Critical Care
Posted: 3/26/2013 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
There are several reasons why a mechanically ventilated patient may decompensate post-intubation. Immediate action is often needed to reverse the problem, but it can be difficult to remember where to start as the vent alarm is sounding and the patient is decompensating.
Consider using the mnemonic “D.O.P.E.S. like D.O.T.T.S.” to assist you in first diagnosing the problem (D.O.P.E.S.) and then fixing the problem (D.O.T.T.S.). You can view an entire lecture on the Crashing Ventilated Patient here.
Step 1: Could this decompensation be secondary to D.O.P.E.S.?
Step 2: Fix the problem with D.O.T.T.S.
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Visual Diagnosis
Posted: 3/25/2013 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
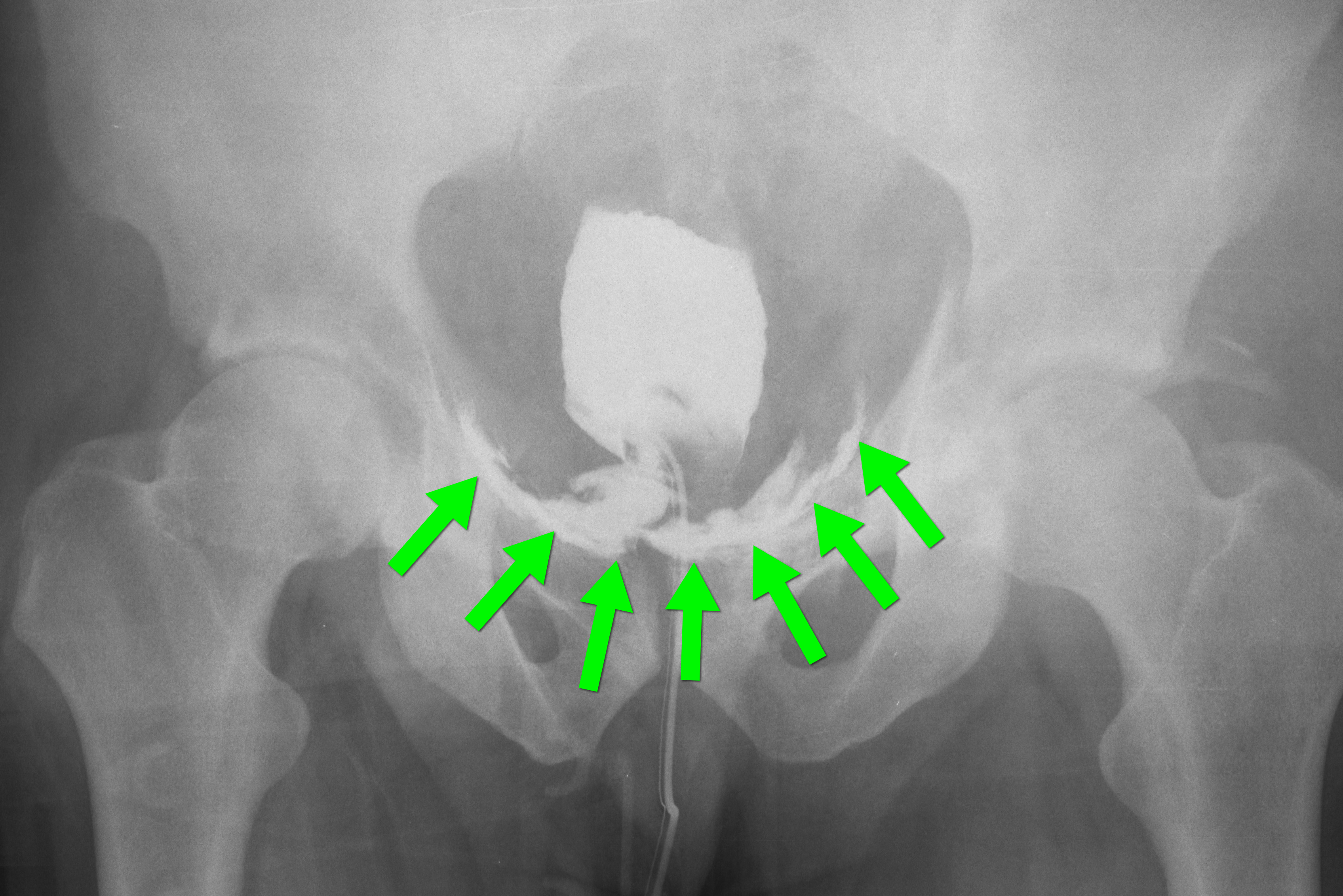
35 year-old male presents after a motor vehicle crash. No blood seen at the meatus of the penis and a Foley catheter is placed (see photo below). What's the next diagnostic step?

Answer: Retrograde cystogram
Traumatic bladder rupture
Gross or microscopic hematuria (>50 RBCs per high-power field) following blunt trauma requires a retrograde cystogram to evaluate for bladder injury. If blood is present at the meatus, however, urethral injury (not discussed) should be suspected and retrograde urethrogram should be performed before passing a Foley catheter.
A retrograde cystogram is performed by infusing diluted contrast into the bladder (200-400 mL) to gently distend the bladder and allow visualization of potential rupture(s). A CT scan of the abdomen and pelvis is then performed to determine if any contrast has leaked from the bladder; alternatively an AP pelvis can also be used, but is not as sensitive as CT.
Traumatic bladder ruptures are categorized as either intra-peritoneal or extra-peritoneal (note: X-ray below demonstrates extra-peritoneal rupture).
Treatment for bladder rupture:
Prognosis is typically good for either injury.

Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Cardiology
Keywords: LVH (PubMed Search)
Posted: 3/25/2013 by Semhar Tewelde, MD
Click here to contact Semhar Tewelde, MD
Okin PM, Roman MJ, Devereux RB, Kligfield P. Electrocardiographic identification of increased left ventricular mass by simple voltage-duration products. J Am Coll Cardiol. 1995 Feb; 25(2):417-23.
Category: Pediatrics
Posted: 3/23/2013 by Mimi Lu, MD
Click here to contact Mimi Lu, MD
In children, it is important to consider the maximum doses of local anesthetics when performing a laceration repair or painful procedure like abscess drainage. If there are multiple lacerations, or large lacerations, it may be possible to exceed those doses if one is not careful.
Max doses of common anesthetics
For example, in a 20 kg child (an average 5-6 year old), the maximum doses would be:
Pearls:
Category: Toxicology
Keywords: dexmedetomidine, cocaine (PubMed Search)
Posted: 3/21/2013 by Fermin Barrueto
(Updated: 2/3/2026)
Click here to contact Fermin Barrueto
Cocaine toxicity is characterized by the sympathomimetic toxidrome: tachycardia, hypertension, hyperpyrexia, diaphoresis as well as sodium channel blocking effects that can cause local anesthesia topically, QRS widening and even seizure.
Usual treatment for a cocaine toxic patient is benzodiazepines and cooling. Be wary of end organ damage, trauma and seizures.
There was a recent study that looked at dexmedetomidine to treat the sympathomimetic effects. Placebo-controlled trial used cocaine-addicted volunteer and applied intranasal cocaine. Measuring skin sympathetic nerve activity and skin vascular resistance, this study, unfortunately, showed as the dose increased MAP did not fall further and increased paradoxically in 4 of 12 subjects.
This highlights the incredible physiologic mechanism of catecholamine release from the CNS with cocaine. This mechanism overlaps some with the centrally acting alpha agonist - dexmedetomidine and was shown in the study by Kontak et al.
Kontak AC, Victor RG, Vongpatanasin W.
Hypertension. 2013 Feb;61(2):388-94
Category: International EM
Keywords: novel, coronavirus, International, infectious, SARS, pulmonary (PubMed Search)
Posted: 3/19/2013 by Andrea Tenner, MD
(Updated: 3/25/2013)
Click here to contact Andrea Tenner, MD
General Information:
14 cases of lower respiratory infection caused by a new coronavirus (not the original SARS virus, but with a similar picture) occurred in the past year. Mortality rate of this virus is >50%.
Area of the world affected:
Relevance to the US physician:
Bottom Line:
Consider this infection in patients with a lower respiratory tract infection who have traveled to or had contact with someone who traveled to the above regions in the past 10 days.
ASK ABOUT RECENT TRAVELS IN PATIENTS PRESENTING WITH SYMPTOMS OF SEVERE LOWER RESPIRATORY TRACT INFECTION!
University of Maryland Section of Global Emergency Health
Author: Veronica Pei MD, MPH
cdc.gov/mmwr/preview/mmwrhtml/mm6210a4.htm?s_cid=mm6210a4_w
Category: Critical Care
Posted: 3/19/2013 by Mike Winters, MBA, MD
(Updated: 2/3/2026)
Click here to contact Mike Winters, MBA, MD
Extubating in the ED
McConville JF, Kress JP. Weaning patients from the ventilator. NEJM 2012; 367:2233-9.
Category: Visual Diagnosis
Posted: 3/18/2013 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
A 56-year-old woman with a history of psoriasis presents with fever, nausea, and painful pin-point pustules on an erythematous base. Her dermatologist recently reduced her prednisone dose. What's the diagnosis?

Answer: Pustular psoriasis
Pustular psoriasis
Occurs in patients with psoriasis, classically occurring after a decrease in dose or cessation of systemic steroids
Symptoms include:
These lesions can eventually drain and desquamate, leaving large patches of exposed dermis.
Complications include:
Patients may be admitted for supportive care and treatment with disease-modifying antirheumatic drugs (DMARDs) such as cyclophosphamide or methotrexate.
REFERENCE
L Naldi, D Gambini, The clinical spectrum of psoriasis, Clinics in Dermatology, Volume 25, Issue 6, November–December 2007, Pages 510-518
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Cardiology
Posted: 3/17/2013 by Semhar Tewelde, MD
Click here to contact Semhar Tewelde, MD
Zanuttini D, Armellini I, et al. Impact of Emergency Coronary Angiography on In-Hospital Outcome of Unconscious Survivors After Out-of-Hospital Cardiac Arrest Original. J Am Coll Cardiol 2012; 110:12 pages 1723-1728
Category: Orthopedics
Keywords: scapular, fracture (PubMed Search)
Posted: 3/16/2013 by Michael Bond, MD
(Updated: 2/3/2026)
Click here to contact Michael Bond, MD
Scapular fractures
Carol Rivers Written Board Review Book 7th edition, Ohio Acep
Category: Toxicology
Keywords: gastric lavage, GI decontamination (PubMed Search)
Posted: 3/9/2013 by Bryan Hayes, PharmD
(Updated: 3/14/2013)
Click here to contact Bryan Hayes, PharmD
In 2013, the American Academy of Clinical Toxicology and European Association of Poisons Centres and Clinical Toxicologists published a second update to their position statement on gastric lavage for GI decontamination (original 1997, 1st update 2004).
Bottom line: Gastric lavage generally causes more harm than good. It should not be thought of as a viable GI decontamination method.
Bonus: Dr. Leon Gussow (@poisonreview) reviews the position paper on his blog, The Poison Review, here: http://www.thepoisonreview.com/2013/02/23/gastric-lavage-fuggedaboutit/
Benson BE, et al. Position paper update: gastric lavage for gastrointestinal decontamination. Clin Toxicol 2013 Feb 18. [Epub ahead of print]
Follow me on Twitter (@PharmERToxGuy)
Category: International EM
Posted: 3/13/2013 by Walid Hammad, MD, MBChB
Click here to contact Walid Hammad, MD, MBChB
Case Presentation: A 31 yo Hispanic male presents to your emergency department with extensive facial abrasions and contusions from an assault 7-8 days ago, c/o difficulty swallowing for 1-2 days. He was seen at that time in a nearby emergency department for his abrasions and contusions.
Upon examination, you find him to be irritable and restless, diaphoretic, tachycardic, and with mild neck stiffness. Over the course of his stay in the ED, he develops generalized muscle rigidity, severe neck stiffness and opisthotonic posturing.
Clinical Question: What is the diagnosis? And what went wrong?
Answer: This is an early presentation of generalized tetanus.
Unfortunately, little evidence exists to support any particular therapeutic intervention in tetanus. There are only nine randomized trials reported in the literature over the past 30 years. The goals of treatment include:
. At risk populations:
o Elderly patients are substantially less likely than young individuals to have adequate immunity against tetanus.
o Immigrants from Mexico had a 67% non-protective anti-tetanus antibody (ATA) level.
o In a pilot study 86% of Korean immigrants did not have protective ATA levels
o Emergency physicians were less likely to adhere to the tetanus guidelines when admitting patients to the hospital.
· Halting the toxin production: wound management and antimicrobial therapy
o Metronidazole 500mg IV q 6-8 hrs or Penicillin-G 2-4M units IV q4-6 hrs for 7-10 days
· Neutralization of the unbound toxin
o Human Tetanus Immunoglobulin (HTIG): A dose of 3000 to 6000 units intramuscularly should be given ASAP
o Since tetanus is one of the few bacterial diseases that does NOT confer immunity following recovery from acute illness, all patients with tetanus should receive FULL active immunization immediately upon diagnosis
· Treatment of generalized tetanus: this is best performed in the ICU and includes:
o Early and aggressive airway management
o Control of muscle spasms
o Management of dysautonomia
o General supportive management
Bottom Line:
o EP’s consistently under-immunize for tetanus, especially in elderly and immigrant populations, who have a much higher risk of under-immunization.
o Better awareness of tetanus prophylaxis recommendations is necessary, and future tetanus prophylaxis recommendations may be more effective if they are also based on demographic risk factors.
o Emergency physicians must comply with immunization guidelines for injured patients to assure adequate protection from both tetanus and diphtheria.
University of Maryland Section of Global Emergency Health
Author: Terry Mulligan DO, MPH
Alagappan K, Rennie W, Kwiatkowski T, Falck J, Silverstone F, and Silverman R. Seroprevalence of tetanus antibody titers in adults over 65 years of age. Annals of Emergency Medicine. 1996; 28:18-21.
Alagappan K, Rennie W, Kwiatkowski T, and Narang V. Antibody protection to diphtheria in the elderly. Annals of Emergency Medicine. 1997; 30:455-58.
Alagappan K, Rennie W, Narang V and Auerbach C. Immunologic response to tetanus toxoid in the elderly. Annals of Emergency Medicine. 1997; 30:459-462.
Alagappan K, Rennie W, Lin D, Auerbach C. Immunologic response to tetanus toxoid in the elderly:one year follow-up. Annals of Emergency Medicine. 1998; 32:155-60.
Talan D, Abrahamian F, Moran G, Mower W, Alagappan K, Tiffany B, Pollack C, Steele M, Dunbar L, Bajani M, Weyant R, Ostroff S. Tetanus immunity and physician compliance with tetanus prophlyaxis practices among emergency department patients presenting with wounds. Annals of Emergency Medicine. 2004, 43: 305-314
Alagappan K, Pulido G, Caldwell J, Abrahamian FM. Tetanus immunoprophylaxis in the emergency department: physician compliance in admitted versus discharged patients. Southern Medical Journal. Volume 99, No 3, 2006
Alagappan K, McGowan J, DeClaro D, Ng D, Silverman RA, Tetanus antibody protection among HIV-infected US-born patients and immigrants. International Journal of Emergency Medicine, Vol 2 : 123-126, June 2008
Alagappan K, Park R, Kuo T, Naderi S, Silverman R. Seroprevalence of tetanus antibody titers among Korean Americans in the New York City area -a pilot study, J Immigrant Minority Health. 11:105-107, 2009.
World Health Organization. Immunization surveillance, assessment and monitoring. Maternal and Neonatal Tetanus (MNT) elimination. http://www.who.int/immunization_monitoring/diseases/MNTE_initiative/en/index.html (Accessed on March 14, 2011).
Category: Critical Care
Posted: 3/12/2013 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
Mechanically ventilated patients can develop a condition in which air becomes trapped within the alveoli at end-expiration; this is called auto-PEEP.
Auto-peep has several adverse effects:
Auto-PEEP classically occurs in intubated patients with asthma or emphysema, but it may also occur in the absence of such disease. The risk of auto-PEEP is increased in patients with:
Auto-PEEP may be treated by:
Patients may need to be heavily sedated to accomplish the above ventilator maneuvers.
Follow me on Twtitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Visual Diagnosis
Posted: 3/11/2013 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
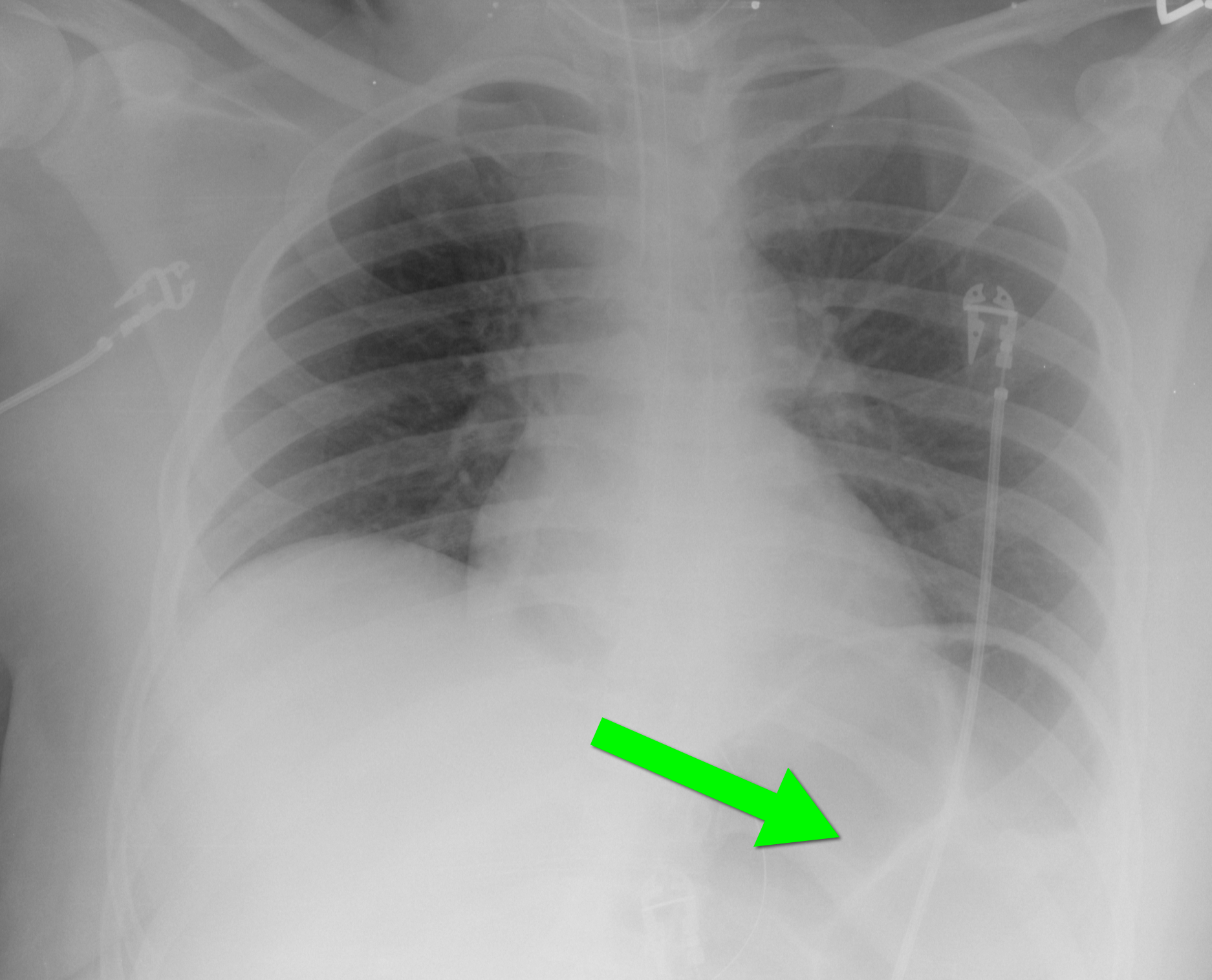
40 year-old female requiring intubation for altered mental status. CXR is below with something under the left diaphragm. What’s the diagnosis?
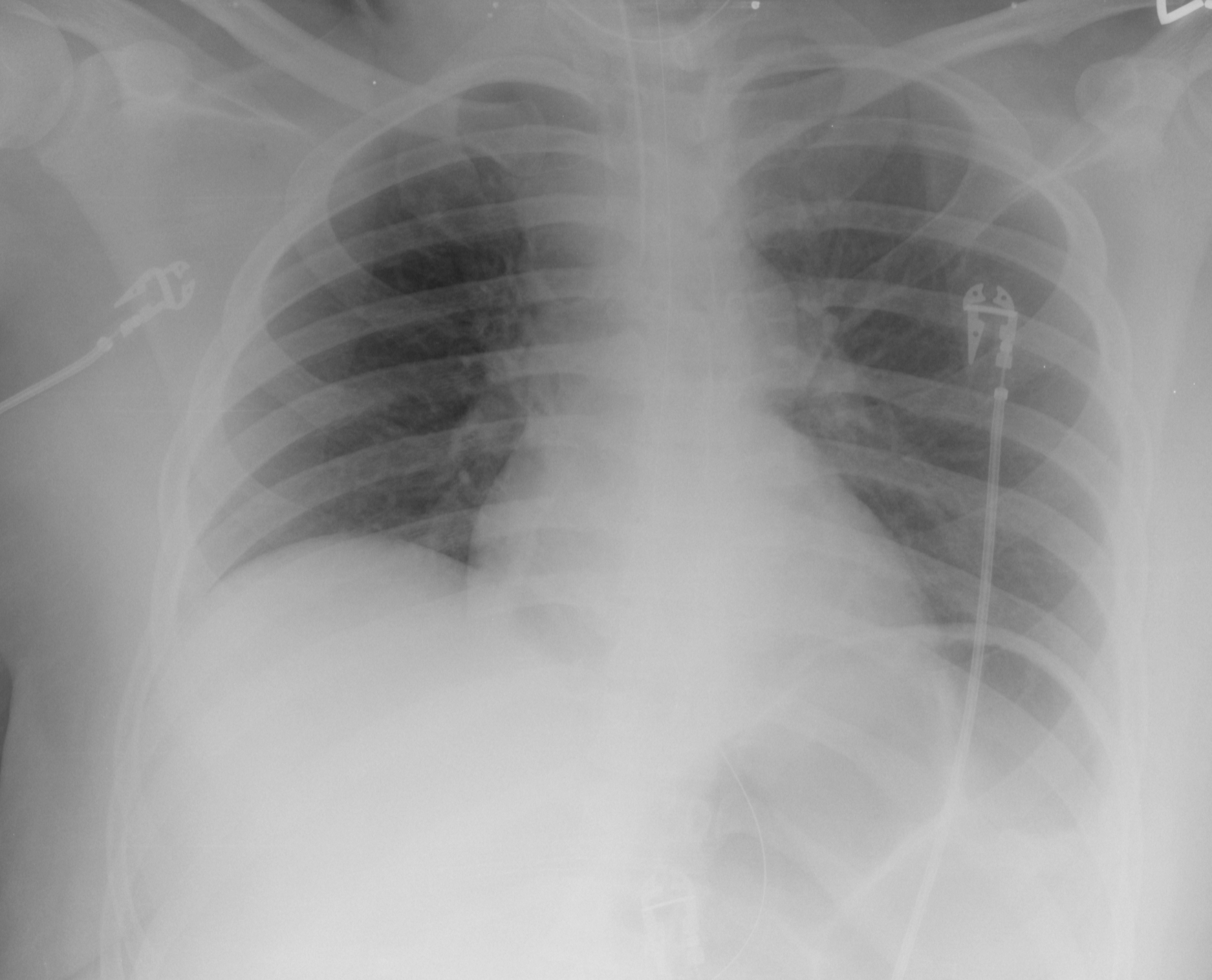
Answer: Loop of colon.
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Cardiology
Posted: 3/10/2013 by Semhar Tewelde, MD
Click here to contact Semhar Tewelde, MD
Boccara F, et al. HIV and Coronary Heart Disease. J Am Coll Cardiol 2013;61:511–23
Category: Orthopedics
Keywords: Concussion, closed head injury, return to play (PubMed Search)
Posted: 3/9/2013 by Brian Corwell, MD
Click here to contact Brian Corwell, MD
Key components in the determination of return to play following concussion include assessment of 1) brain function, 2) reaction time and 3) balance testing
Balance testing has become increasingly utilized in the diagnosis and management of sports related concussion. Studies have identified temporary or permanent deficits in static and/or dynamic balance in individuals with mild-to-moderate traumatic brain injury and sports related concussion. An example of this is the Balance Error Scoring System (BESS). Three stances are testing (narrow double-leg stance, single leg stance and a tandem stance) with the hands on the hips and eyes closed for 20 seconds. The FNL Sideline Concussion Assessment Tool utilizes a modified BESS. Example video below:
http://www.youtube.com/watch?v=xtJgv-D7IdU
