Category: Visual Diagnosis
Posted: 7/1/2013 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
65 year-old male presents with nausea and diffuse abdominal pain, 3 days after knee replacement surgery. What's the diagnosis?
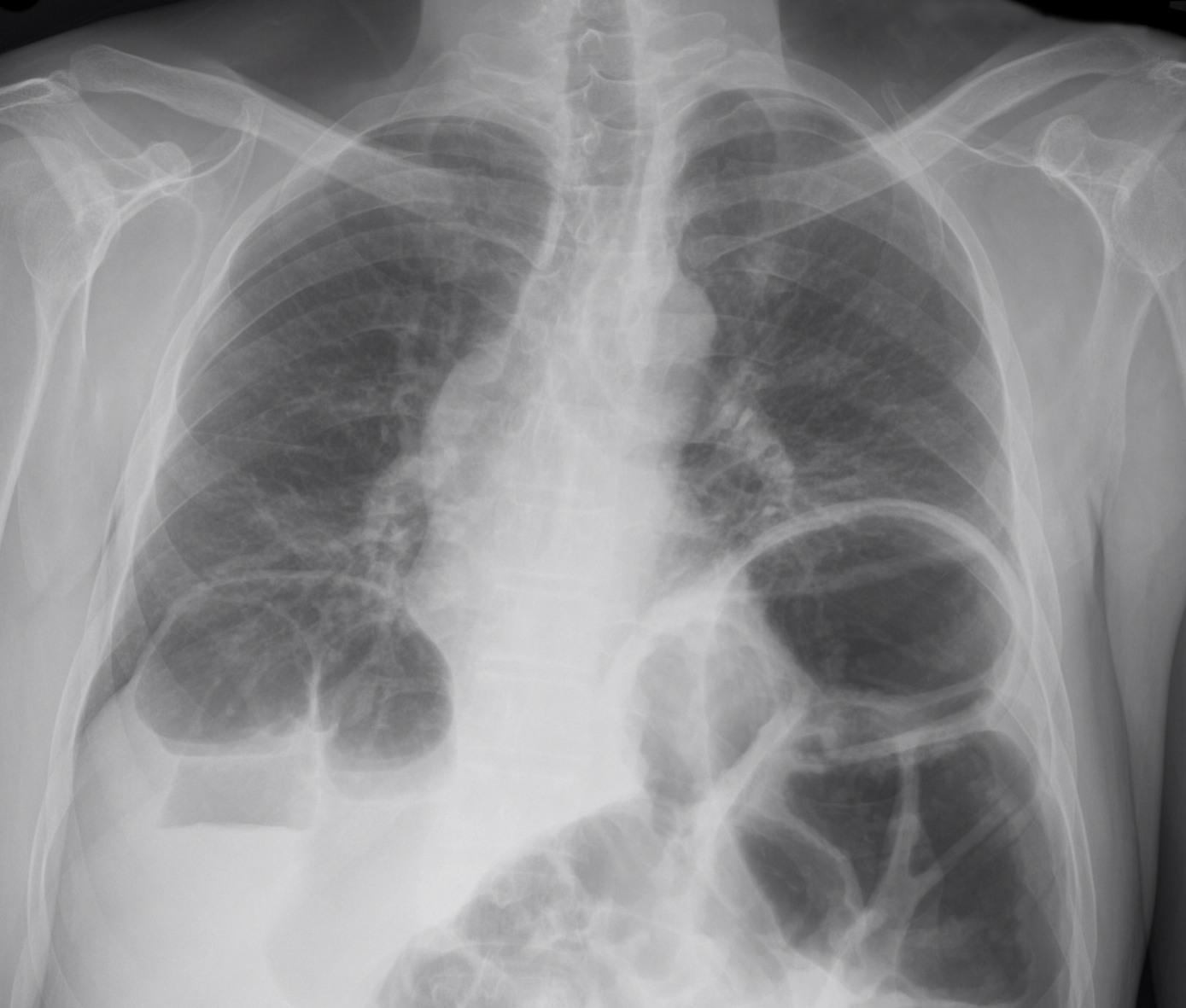
Adynamic ileus
Risk factors include
Imaging reveals distention of both large and small bowel without a transition zone, which differs from a small or large bowel obstruction. Such cases can be difficult to differentiate clinically from one another, so physicians often rely on imaging, specifically CT scanning to define a discrete obstruction versus an ileus.
References
1. Hayden and Sprouse, Bowel Obstruction and Hernia, Med Clin N Amer 29 (2011) 319-345
2. American College of Radiology, Suspected Small Bowel Obstruction, ACR Appropriateness Guidelines, rev. 2010
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Cardiology
Posted: 6/30/2013 by Semhar Tewelde, MD
(Updated: 2/3/2026)
Click here to contact Semhar Tewelde, MD
Kini A, Baber U, et al. Changes in Plaque Lipid Content After Short-Term Intensive Versus Standard Statin Therapy. JACC. Vol. 62, No. 1, 2013
Category: Orthopedics
Posted: 6/29/2013 by Michael Bond, MD
(Updated: 2/3/2026)
Click here to contact Michael Bond, MD
Sternal fractures
Brookes JG, Dunn RJ, Rogers IR. Sternal fractures: a retrospective analysis of 272 cases. J Trauma. Jul 1993;35(1):46-54. PMID 8331712
Category: Pediatrics
Keywords: NIV, intubation (PubMed Search)
Posted: 6/28/2013 by Mimi Lu, MD
Click here to contact Mimi Lu, MD
Category: Toxicology
Keywords: sotalol, torsade de pointes (PubMed Search)
Posted: 6/27/2013 by Fermin Barrueto
(Updated: 2/3/2026)
Click here to contact Fermin Barrueto
When reviewing a patient's medication list, there are always some that should catch your eye. Digoxin is one since we can measure it, has a low therapeutic index and elimination is effected when renal function is diminished. Another drug that should catch your eye is SOTALOL. Renally cleared and affected by even a minimally lower than normal magnesium. The toxic effect even at therapeutic levels is torsades de pointes.
One study, in a 736 bed hospital, showed 89% of patients prescribed sotalol were on an inappropriate dose due to renal function and an odds ratio of 3.7 increased re-admission rate at 6 months for the patients on the inappropriate dose of sotalol.
We can catch this in the ED. Involve your pharmacist, ED pharmacist or local toxicologist for dosing calculations.
Assessment of sotalol prescribing in a community hospital: opportunities for clinical pharmacist involvement. Finks SW, Rogers KC, Manguso AH. Int J Pharm Pract. 2011 Aug;19(4):281-6.
Category: International EM
Keywords: Pediatric, IFEM, guidelines, international (PubMed Search)
Posted: 6/26/2013 by Andrea Tenner, MD
(Updated: 2/3/2026)
Click here to contact Andrea Tenner, MD
General Information:
An estimated 70 children in the world die every 5 minutes-- 99% of these deaths are from developing countries, half in Sub-Saharan Africa , and two-thirds from preventable or easily treatable causes.
Area of the world affected:
One study examining the quality of hospital emergency care of 131 children in 21 hospitals in 7 developing countries found:
· 66% of hospitals did not have adequate triage; 41% of patients had inadequate initial assessment;
· 44% received inappropriate treatment and 30% had insuf cient monitoring.
· Frequent essential drugs, laboratory and radiology services supply outages
· Staffing and knowledge shortages for medical and nursing personnel
Relevance to the US physician:
The International Federation of Emergency Medicine (IFEM) used a consensus approach to develop the International Standards for Emergency Care of Children in Emergency Departments, published in July 2012.
· The standards covering initial assessment, stabilization and treatment, staf ng and training
· Guidelines for coordinating, monitoring and improving the pediatric emergency care are addressed
Bottom Line:
The IFEM International Standards for Emergency Care of Children provide an excellent resource for both clinicians and hospital managers in developing countries.
University of Maryland Section of Global Emergency Health
Author:Terrence Mulligan DO, MPH,FIFEM, FACEP, FAAEM, FACOEP, FNVSHA
--thanks and acknowledgments to Baljit Cheema, University of Cape Town and Stellenbosch University, South Africa
Lozano R, Wang H, Foreman KJ, Rajaratnam JK, Naghavi M, Marcus JR, et al. Progress towards Millennium Development Goals 4 and 5 on maternal and child mortality: an updated systematic analysis. Lancet 2011;378(9797):1139–65.
[1] You D, Jones G, Hill K, Wardlaw T, Chopra M. Levels and trends in child mortality, 1990-2009. Lancet 2010;376(9745):931–3.
[1] Cheema B. International standards of care for children in emergency centres – do they apply to Africa? African Journal of Emergency Medicine (2013) 3, 50–51
[1] Nolan T, Angos P, Cunha AJ, Muhe L, Qazi S, Simoes EA, Tamburlini G, Weber M, Pierce NF. Quality of hospital care for seriously ill children in less-developed countries. Lancet 2001 Jan 13;357(9250):106–10.
[1] International Standards for Emergency Care of Children in Emergency Departments. Full Document Available from: http://www.ifem.cc/Resources/PoliciesandGuidelines.aspx
Category: Critical Care
Posted: 6/25/2013 by Mike Winters, MBA, MD
(Updated: 2/3/2026)
Click here to contact Mike Winters, MBA, MD
CVP and Fluid Responsiveness
Marik PE, Cavallazzi R. Does the central venous pressure predict fluid responsiveness? An updated meta-analysis and a plea for some common sense. Crit Care Med 2013:41:1774-1781.
Category: Visual Diagnosis
Posted: 6/23/2013 by Haney Mallemat, MD
(Updated: 6/24/2013)
Click here to contact Haney Mallemat, MD
Name three differential diagnoses based on the CXR below.
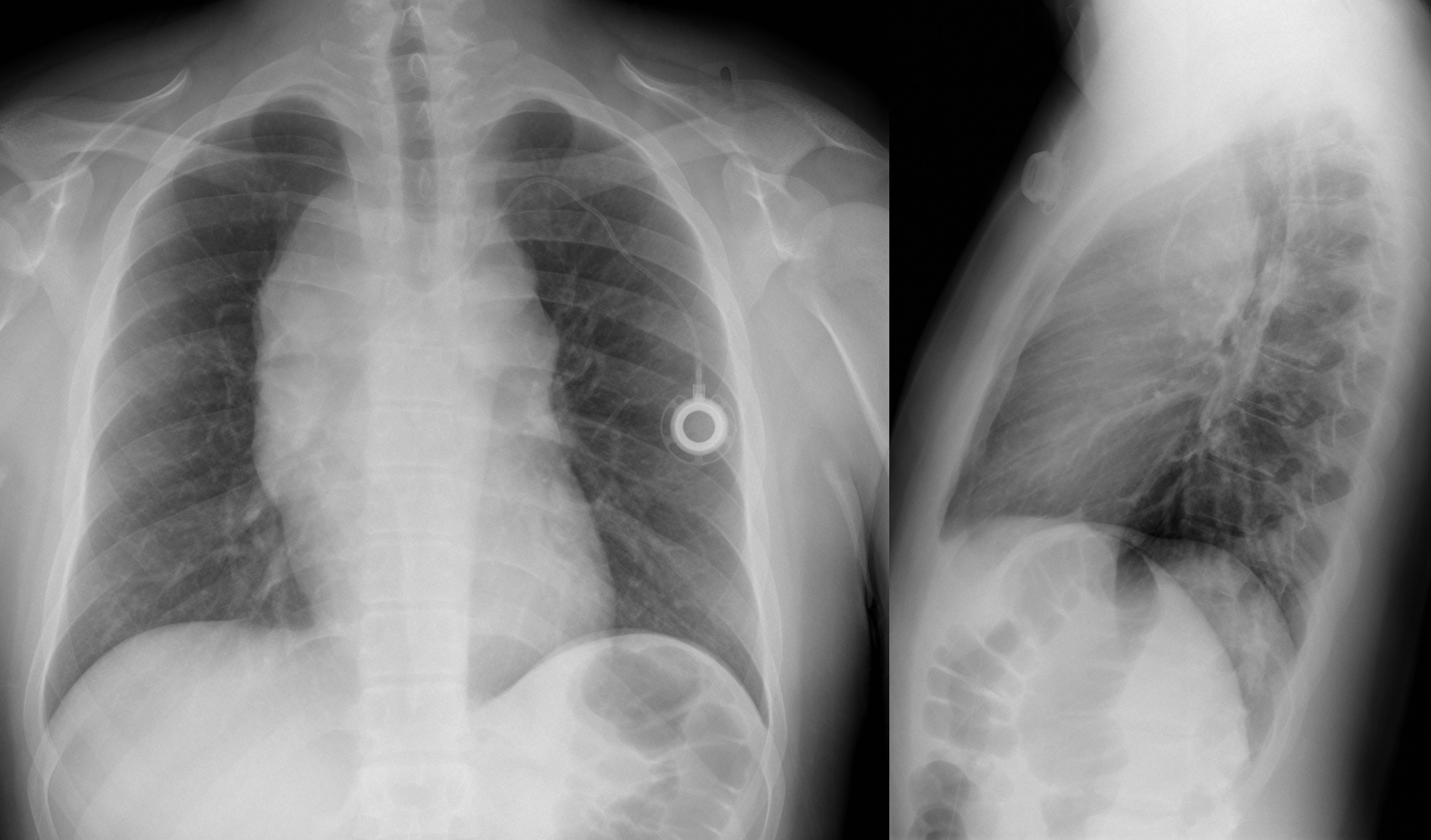
The diagnosis in this case is Non-Hodgkin lymphoma, but read below for more differentials.
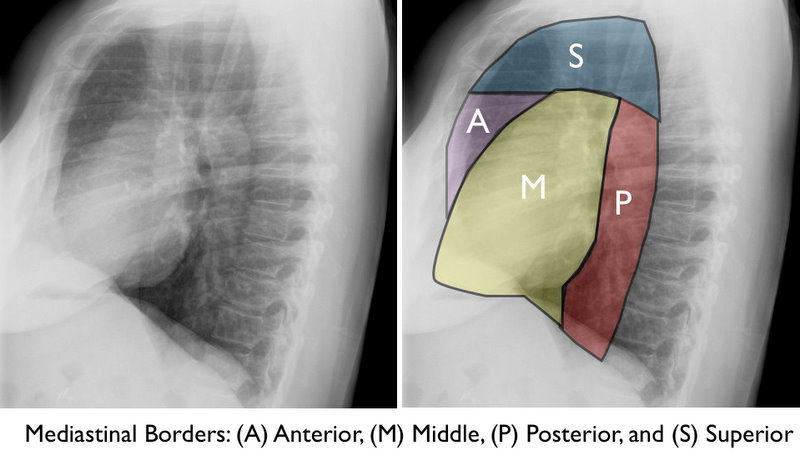
Mediastinal Masses
The mediastinum is subdivided into the regions shown below. Here are some differential diagnoses based on region.
Anterior / Superior Mediastinum
Middle Mediastinum
Posterior Mediastinum
Congratulations to all the graduating residents, especially our own at the University of Maryland. I wish you all the best as you start your phenomenal careers!
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Cardiology
Posted: 6/23/2013 by Semhar Tewelde, MD
Click here to contact Semhar Tewelde, MD
Bifascicular block
Incomplete Trifascicular block
Complete Trifascicular block
Category: Orthopedics
Keywords: Tennis Elbow, ECRB tendon (PubMed Search)
Posted: 6/22/2013 by Brian Corwell, MD
Click here to contact Brian Corwell, MD
Tennis Elbow
The tendon usually involved in tennis elbow is called the Extensor Carpi Radialis Brevis (ECRB).
The ECRB muscle helps stabilize the wrist when the elbow is straight.
Ask the patient to straighten the arm at the elbow and then perform resisted long finger extension. This will stress the ECRB and reproduce the pain. One can also ask the patient to lift the top of a chair in the air with the elbow extended.
Category: International EM
Keywords: hepatitis A, international, food-borne illness (PubMed Search)
Posted: 6/19/2013 by Andrea Tenner, MD
(Updated: 6/26/2013)
Click here to contact Andrea Tenner, MD
General Information:
Hepatitis A is a food-borne illness that is prevalent in developing countries. Currently in the US we are experiencing an outbreak in 8 states related to a frozen blend of organic berries. (Linked to Townson Farms brand sold at Costco and Harris Teeter)
Clinical Presentation:
- Case definition: sudden onset of S/S + jaundice or elevated liver enzyme levels
- S/S: nausea, anorexia, fever, malaise, abdominal pain
Diagnosis:
- Hepatitis A IgM
Treatment:
- Exposed patients should be given the Hep A vaccine within 2 weeks of exposure
- Exposed patients >40 yrs old, <1 yr old, immunocompromised, or with chronic liver disease: give immunoglobulin instead (risk of more severe disease)
- Supportive care
Bottom Line:
Patients potentially exposed to Hepatitis A in the past 2 weeks should be given either the vaccination or immunoglobulin, depending on comorbid conditions. Treatment of active infection is supportive.
University of Maryland Section of Global Emergency Health
Author: Andi Tenner, MD, MPH
http://www.cdc.gov/hepatitis/HAV/HAVfaq.htm#general
http://www.cdc.gov/hepatitis/Outbreaks/2013/A1b-03-31/index.html
Category: Critical Care
Posted: 6/18/2013 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
Keep Immune Thrombocytopenic Purpura (ITP) in your differential for patients with thrombocytopenia and evidence of bleeding. Although ITP has classically been described in children, it can occur in adults; especially between 3rd- 4th decade.
Thrombocytopenia leads to the extravasation of blood from capillaries, leading to skin bruising, mucus membrane petechial bleeding, and intracranial hemorrhage.
ITP occurs from production of auto-antibodies which bind to circulating platelets. This leads to irreversible uptake by macrophages in the spleen. Causes of antibody production include:
Suspect ITP in patients with isolated thrombocytopenia on a CBC without other blood-line abnormalities. Abnormality in other blood-line warrants consideration of another diagnosis (e.g., leukemia).
ITP cannot be cured; treatments include:
Category: Cardiology
Posted: 6/16/2013 by Semhar Tewelde, MD
Click here to contact Semhar Tewelde, MD
Stanford type A (proximal) aortic dissection accounts for ~60% of all aortic dissections
Classic treatment includes direct surgical replacement of the ascending aorta w/prosthetic graft (+/- AV aortic repair/replacement)
~20-30% of these patients (*institutional dependent) are considered poor candidates for surgery and receive only medical management, which innately results in substandard outcomes
In this study those who were considered poor candidates for surgical repair underwent novel endovascular treatment
Endovascular repair in this study was considered both appropriate and improved traditional medical outcomes in patients who were considered poor candidates
Lu Q, Feng J, et al. Endovascular Repair of Ascending Aortic Dissection A Novel Treatment Option for Patients Judged Un t for Direct Surgical Repair. J Am Coll Cardiol 2013;61:1917–24
Category: Orthopedics
Keywords: Trapezium, Fracture (PubMed Search)
Posted: 6/15/2013 by Michael Bond, MD
Click here to contact Michael Bond, MD
Trapezium Fractures
Suspect the Diagnosis when you note
If you are suspected the diagnosis oblique radiographs or a CT scan of the wrist will note the fracture the best.
Treatment consists of placing the patient in a thumb spica splint.
Category: Pediatrics
Posted: 6/14/2013 by Rose Chasm, MD
(Updated: 2/3/2026)
Click here to contact Rose Chasm, MD
Pediatrics Text 19th edition, Nelson
Category: Toxicology
Keywords: acetylcysteine, NAC, INR, PT, prothrombin time (PubMed Search)
Posted: 6/12/2013 by Bryan Hayes, PharmD
(Updated: 6/13/2013)
Click here to contact Bryan Hayes, PharmD
In the treatment of acetaminophen poisoning with N-acetylcysteine (NAC), the PT/INR can be slightly elevated even in the absence of hepatotoxicity. Considering Prothombin Time (PT) is one of the criteria used to assess severity of liver damage in this setting, it is important to know how much the PT/INR can be affected by NAC and if it has an actual effect on coagulation factor levels.
Clinical Practice Pearls
1. Pizon AF, et al. The in vitro effect of n-acetylcysteine on prothrombin time in plasma samples from healthy subjects. Acad Emerg Med 2011;18:351-4. [PMID 21496136]
2. Jang DH, et al. In vitro study of n-acetylcysteine on coagulation factors in plasma samples from healthy subjects. J Med Tox 2013;9:49-53. [PMID 22733602]
Follow me on Twitter (@PharmERToxGuy)
Category: International EM
Keywords: Listeria, cheese, infectious disease, fever, gastroenteritis, pregnant (PubMed Search)
Posted: 6/12/2013 by Andrea Tenner, MD
Click here to contact Andrea Tenner, MD
General Information:
-Listeria can cause serious infections in vulnerable groups: adults >65 years old, pregnant women, newborns, immunocompromised
-In a recent CDC report, infection with Listeria was associated with a 20% mortality rate.
Clinical Presentation:
- History of cantaloupe, soft cheese, or raw produce ingestion
- Non-specific symptoms: fever, myalgias, occasionally preceded by GI symptoms
-Can have headache, stiff neck, confusion, AMS, miscarriage or stillbirth in pregnant women
Diagnosis:
- Blood, CSF, or amniotic fluid culture showing Listeria monocytogenes
- Listeria is a reportable disease
Treatment:
- Ampicillin and Penicillin G are the drugs of choice
- Add gentamycin in CSF infection, endocarditis, the immunocompromised, and neonates.
Bottom Line:
Listeria infections have a high mortality rate and can be found worldwide. Suspect in patients who have febrile syndromes and travel to areas where they may consume unpasteurized cheese.
University of Maryland Section of Global Emergency Health
Author: Andi Tenner, MD, MPH
Older Americans, pregnant women face highest risk from Listeria food poisoning. http://www.cdc.gov/media/releases/2013/p0604-listeria-poisoning.html
http://www.cdc.gov/listeria
Category: Critical Care
Posted: 6/11/2013 by Mike Winters, MBA, MD
Click here to contact Mike Winters, MBA, MD
Rhabdomyolysis in the Critically Ill
Shapiro ML, Baldea A, Luchette FA. Rhabdomyolysis in the Intensive Care Unit. J Intensive Care Med 2012; 27:335-342.
Category: Visual Diagnosis
Posted: 6/10/2013 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
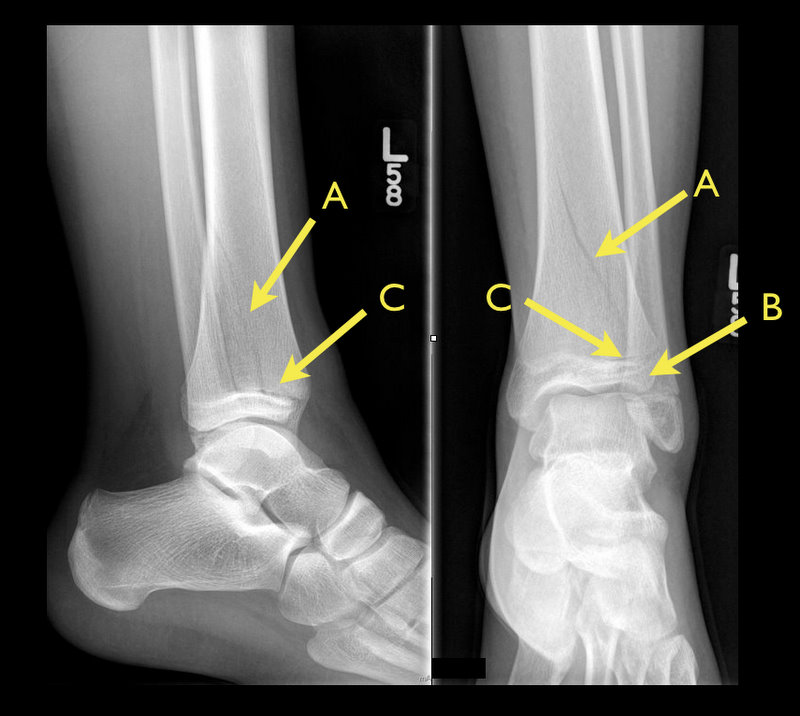
13 year-old female with ankle pain following fall down escalator. What's the diagnosis?

Answer: Tri-plane ankle fracture
Tri-plane Fractures

Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Cardiology
Posted: 6/9/2013 by Semhar Tewelde, MD
Click here to contact Semhar Tewelde, MD
Khoo C, Chakrabarti S, et al. Recognizing Life-Threatening Causes of Syncope. Cardiology Clinics. Volume 31, Feb, 2013
