Category: Airway Management
Posted: 9/13/2013 by Rose Chasm, MD
(Updated: 2/3/2026)
Click here to contact Rose Chasm, MD
2012 PREP Self-Assessment. American Academy of Pediatrics
Category: Toxicology
Keywords: hypoglycemia, overdose, diabetes, antidiabetic (PubMed Search)
Posted: 9/10/2013 by Bryan Hayes, PharmD
(Updated: 9/12/2013)
Click here to contact Bryan Hayes, PharmD
With several new diabetes medications available, it is important to know which ones are likely to cause hypoglycemia after overdose. Based on mechanism of action and reported cases, the likelihood of hypoglycemia after overdose is listed below by drug class.
Keep in mind that other drugs can interact with antidiabetics resulting in hypoglycemia. This table applies only to single agent ingestion/administration.
| Drug Class | Examples | Hypoglycemic Potential |
|---|---|---|
| Insulins | Glargine, Aspart, Detemir | High |
| Sulfonylureas | Glyburide, Glipizide | High |
| Meglitinides | Nateglinide, Repaglinide | High |
| Glucagon-Like Peptide-1 (GLP-1) Receptor Agonists | Exenatide | Low-Moderate |
| Alpha-glucosidase inhibitors | Acarbose, Miglitol | Low |
| Thiazolidinediones | Rosiglitazone, Piaglitazone | Low |
| Biguanides | Metformin | Low |
| Dipeptidyl Peptidase 4 (DPP-4) Inhibitors | Sitagliptin, Saxagliptin | Low |
Bosse GM. Chapter 48. Antidiabetics and Hypoglycemics. In: Bosse GM, ed. Goldfrank's Toxicologic Emergencies. 9th ed. New York: McGraw-Hill; 2011. http://www.accesspharmacy.com/content.aspx?aID=6514172. Accessed September 10, 2013.
Follow me on Twitter (@PharmERToxGuy)
Category: International EM
Keywords: climate, infectious, globalization, population, disease (PubMed Search)
Posted: 9/11/2013 by Andrea Tenner, MD
Click here to contact Andrea Tenner, MD
Background Information:
A recent review article in NEJM evaluated what effects globalization and climate change can be expected to have on human health. If global population increases and temperatures continue to rise, diseases that were once limited by either remoteness or climatologic regions may have new geographical spread.
Pertinent Conclusions:
There are three primary ways which climate change may be expected to affect health:
- Primary: Direct biologic consequences (i.e. heat waves, extreme weather events, air pollution)
- Secondary: Risks caused by process changes (i.e. decreased crop yields, tropical vectors with increased spread)
-Tertiary: More diffuse effects (mental health issues in failed farmers, conflict due to scarce water)
Bottom Line:
No matter what your views are on the causes, the current trend is that the overall climate is getting warmer and human population is increasing. Anticipation of possible consequences is key to planning for the future.
University of Maryland Section of Global Emergency Health
Author: Andi Tenner, MD, MPH
McMichael AJ. Globalization, Climate Change, and Human Health. N Engl J Med 2013; 368:1335-1343.
Category: Critical Care
Keywords: critical care, necrotizing pneumonia, infectious disease, pulmonary (PubMed Search)
Posted: 9/5/2013 by John Greenwood, MD
(Updated: 9/10/2013)
Click here to contact John Greenwood, MD
Necrotizing Pneumonia
Necrotizing pneumonia is a rare, but potentially deadly complication of bacterial pneumonia.
It is characterized by the finding of pneumonic consolidation with multiple areas of necrosis within the lung parenchyma. Necrotic foci may coalesce, resulting in a localized lung abscess, or pulmonary gangrene if involving an entire lobe.
Most common pathogens: S. aureus, S. pneumoniae, and Klebsiella pneumonia.
Others include S. epidermidis, E. coli, Acinetobacter baumannii, H. influenzae and Pseudomonas.
Contrast-enhanced chest CT is the diagnostic test of choice and is also helpful in evaluating for parenchymal complications.
Empiric antibiotic therapy should include:
Consider an early surgical evaluation for the patient with necrotizing pneumonia complicated by septic shock, empyema, bronchopleural fistula, or hemoptysis.
Reference
Tsai YF, Ku YH. Necrotizing pneumonia: a rare complication of pneumonia requiring special consideration. Curr Opin Pulm Med. 2012 May; 18(3):246-52.
Category: Visual Diagnosis
Posted: 9/8/2013 by Haney Mallemat, MD
(Updated: 9/9/2013)
Click here to contact Haney Mallemat, MD
This week's case is challenging, but very interesting...
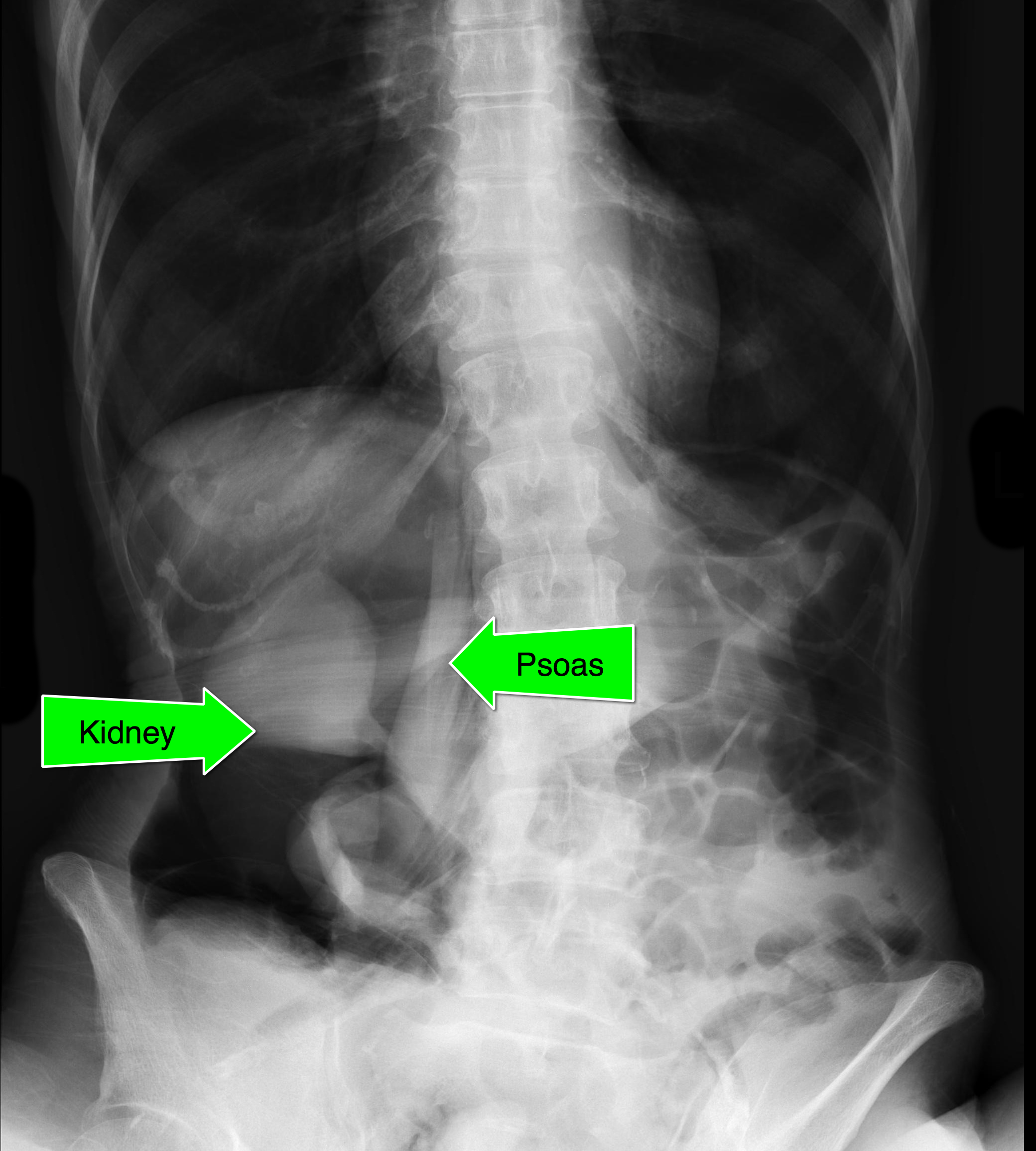
An elderly patient presents with a history of significant weight loss and chronic constipation; abdominal Xray is below. What's the diagnosis? (Hint: why is the right kidney and psoas muscle so well defined?)

Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Cardiology
Posted: 9/8/2013 by Semhar Tewelde, MD
Click here to contact Semhar Tewelde, MD
*Please see the attachment below for Figures A-D
1. Adler A, Rosso R, Viskin D, et al. JACC. Sept. 2013: Vol. 62(10) pgs. 863-868
2. Haissaguerre M., Derval N., Sacher F., et al: Sudden cardiac arrest associated with early repolarization. N Engl J Med 2008; 358: 2016-2023
3. Tikkanen J.T., Anttonen O., Junttila M.J., et al: Long-term outcome associated with early repolarization on electrocardiography. N Engl J Med 2009; 361: 2529-2537
Category: Pharmacology & Therapeutics
Keywords: antibiotic, obese, obesity, critically ill, antimicrobial (PubMed Search)
Posted: 8/31/2013 by Bryan Hayes, PharmD
(Updated: 9/7/2013)
Click here to contact Bryan Hayes, PharmD
Although there is a paucity of data to guide dosing of antimicrobials in the critically ill obese patient, we can draw some conclusions from existing kinetic studies. Assuming normal renal and hepatic function, here's what to do:
Penicillins: Use the high end of dosing range. For example, if the plan is to use piperacillin/tazobactam 3.375 gm IV every 6 hours for a complicated intra-abdominal infection, use 4.5 gm instead.
Cephalosporins: Use the high end of the dosing range.
Carbapenems: Use the high end of the dosing range.
Quinolones: Use the high end of the dosing range.
Aminoglycosides: Dose using adjusted body weight. ABW (kg) = IBW + 0.4 X (actual body weight - IBW)
Vancomycin: 15-20 mg/kg actual body weight every 8 to 12 hours. Adjust based on trough level.
When dosing most antibiotics in critically ill obese patients, use the high end of the dosing range (if not more).
Erstad BL. Dosing of medications in morbidly obese patients in the intensive care unit setting. Intensive Care Med 2004;30(1):18-32. [PMID 14625670]
Medico CJ, Walsh P. Pharmacotherapy in the critical ill obese patient. Crit Care Clin 2010;26(4):679-88. [PMID 20970057]
Follow me on Twitter (@PharmERToxGuy)
Category: Airway Management
Keywords: NMS, haldol, haloperidol, fluphenazine, dantrolene, bromocriptine, diazepam (PubMed Search)
Posted: 9/5/2013 by Ellen Lemkin, MD, PharmD
Click here to contact Ellen Lemkin, MD, PharmD
NMS is most often seen with the typical high potency neuroleptic agents (e.g haldol, fluphenazine)
All classes of antipsychotics can cause NMS, including low potency and newer atypical agents; antiemetics can cause this as well.
Symptoms usually occur after the first 2 weeks of therapy, but may occur after years of use
Signs and symptoms include:
mental status changes
muscular rigidity (“lead pipe”)
hyperthermia (>38 - 40 degrees).
Autonomic instability (tachycardia, tachycardia and diaphoresis)
Treatment includes discontinuation of the offending agent and providing supportive care.
While no clinical trials have ever been undertaken, dantrolene (muscle relaxant) is commonly used.
Bromocriptine (dopamine agonist) may also be used, and amantadine (dopaminergic and anticholinergic agent) is used as an alternative to bromocriptone
Recently, several case reports have documented the successful use of diazepam as a sole pharmacologic agent. This may be an alternative or a supplement to the above agents
Category: Critical Care
Posted: 9/3/2013 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
UEDVT comprise 10% of all DVTs (majority are lower extremity), but incidence of UEDVT is rising; UEDVTs are categorized into distal (veins distal to axillary vein) or proximal (from superior vena cava to axillary vein)
Compared to lower extremity DVT, UEDVTs have lower:
75% of UEDVT are secondary (indwelling catheters, pacemakers, malignancy, etc.) and 25% are primary in nature; #1 primary cause of UEDVT is Paget – Schroetter disease
Up to 25% of patients with primary UEDVTs are eventually found to have an underlying malignancy; patients with idiopathic UEDVT should be referred for cancer workup
Treatment includes removal of the catheter (if no longer needed) and:
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Visual Diagnosis
Posted: 9/2/2013 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
Elderly male presents with headache, confusion, and trouble with gait. What's in your differential diagnosis?
Based on the CT scan shown, the differential here includes epidermoid and arachnoid cyst
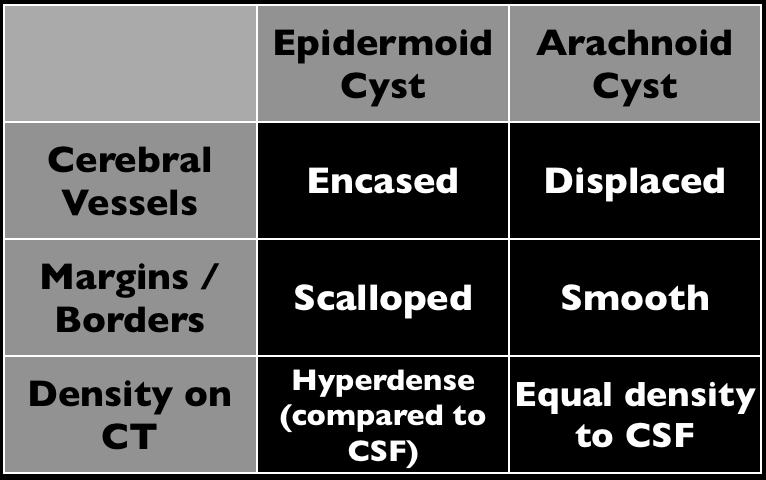
Arachnoid cysts (AC) occur within the cerebrospinal axis and do not communicate with the ventricular system. Most occur in the middle cranial fossa and are typically benign; continuing cerebrospinal fluid
The majority of AC occurs from abnormalities in development, but a small portion occurs secondary to post-surgical adhesions or in association with cancer.
MRI is the test of choice to help define the extent of the cyst as well as determine alternative diagnoses.
Treatment is variable with some experts stating that only symptomatic ACs should be treated with others recommending removal to avoid future complications.
The patient in the stem presented with symptoms secondary to complications from the AC.
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Cardiology
Keywords: Hypertension (PubMed Search)
Posted: 9/1/2013 by Ali Farzad, MD
(Updated: 3/10/2014)
Click here to contact Ali Farzad, MD
Adult ED patients are commonly found to have markedly elevated blood pressures (>160/100) without any signs or symptoms of acute organ injury (ie, cardiovascular, renal, or neurological).
A recently revised ACEP clinical policy aims to guide emergency physicians in the evaluation and management of such patients.
They make the following recommendations (Level C):
Bottom-line:
There's little evidence to guide the decision of which patients with markedly elevated blood pressures to test or treat in the ED. This new clinical policy suggests that routine screening and treatment is not required. Asymptomatic patients should be referred for close follow-up, but consider a BMP in patients with poor follow up.
Want more emergency cardiology pearls? Follow me @alifarzadmd
Wolf SJ, Lo B, Shih RD, et al. Clinical Policy: Critical Issues in the Evaluation and Management of Adult Patients in the Emergency Department with Asymptomatic Elevated Blood Pressure. Ann Emerg Med. 2013;62(1):59–68.
Category: Toxicology
Keywords: flecainide, overdose, sodium channel (PubMed Search)
Posted: 8/29/2013 by Fermin Barrueto
Click here to contact Fermin Barrueto
There are Type 1C Anti-Dysrhythmics, like propafenone and flecainide, that are utilized to suppress atrial fibrillation. They are called Type 1C due to their sodium channel blocking effects. Flecainide has a potent effect on the ECG and has caused significant and resistant widening of the QRS complex.
Typically, a sodium channel blocker like a TCA can be treated with hypertonic sodium bicarbonate but flecainide has been resistant to this at times and there is a reported overdose utilizing magnesium sulfate. (1) Keep that in mind if you were to see a widened QRS complex in the face of a flecainide ingestion.
There has been a Brugada ECG pattern also reported (I know Amal is smiling) (2) ontop of the widened QRS, PR intervals though minimal effect on the QT.
1: Cabrera Ortega M, Gell Aboy J, Díaz Berto E, Monagas Docasal V. [Acute flecainide overdose]. An Pediatr (Barc). 2011 Jan;74(1):56-8. 2: Martínez-Mateo V, Arias MA, Rodríguez-Padial L. [Brugada electrocardiographic pattern elicited by flecainide overdose]. Med Clin (Barc). 2011 Mar 19;136(7):320.
Category: International EM
Keywords: MERS-CoV, Coronavirus, Arabian Peninsula, Infection (PubMed Search)
Posted: 8/28/2013 by Andrea Tenner, MD
Click here to contact Andrea Tenner, MD
General Information:
-MERS-CoV (Middle East Respiratory Syndrome) is a novel coronavirus that produces a SARS-like syndrome. (You might have seen a pearl about this from us in March...)
-Since that time there have been a total of 102 laboratory-confirmed cases with 42 deaths (almost half!)
-All known cases had links to the Arabian Peninsula, although there has been some local non-sustained transmission
Relevance to the EM Physician: Consider MERS-CoV in patients with SARS-like syndrome who have traveled or had contact with someone who has traveled to the Arabian Peninsula within the past 14 days.
Bottom Line: Ask about recent travel in patients with severe acute respiratory illness. If you suspect MERS-CoV, contact your local health department.
University of Maryland Section of Global Emergency Health
Author: Andi Tenner, MD, MPH
http://www.who.int/ith/updates/20130605/en/
http://www.cdc.gov/coronavirus/mers/interim-guidance.html
Category: Critical Care
Keywords: TIA, Minor Stroke, Antiplatelet therapy (PubMed Search)
Posted: 8/27/2013 by Feras Khan, MD
(Updated: 2/3/2026)
Click here to contact Feras Khan, MD
Background
Trial
Results
Conclusions
Bottom Line:
Clopidogrel with Aspirin in Acute Minor Stroke or Transient Ischemic Attack
Y. Wang and Others | N Engl J Med 2013;369:11-19 | Published Online June 26, 2013
Category: Visual Diagnosis
Posted: 8/25/2013 by Haney Mallemat, MD
(Updated: 8/26/2013)
Click here to contact Haney Mallemat, MD
23 year-old patient presents with a rash on his palms and soles. He also states that he had a something strange on his genitals several weeks before. What's the diagnosis and what’s the treatment (including dosing) for this disease?

Centers for Disease Control and Prevention, National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention, Division of STD Prevention. 2010 Treatment Update.
http://www.cdc.gov/std/syphilis/treatment.htm
Follow me on Twitter @criticalcarenow or Google+ (+criticalcarenow)
Category: Cardiology
Posted: 8/25/2013 by Semhar Tewelde, MD
(Updated: 2/3/2026)
Click here to contact Semhar Tewelde, MD
Palmerini T, et al. Clinical Outcomes With Drug-Eluting and Bare-Metal Stents in Patients With ST-Segment Elevation Myocardial Elevation. JACC. 2-13, Vol. 62:2 pgs.196-504
Category: Toxicology
Keywords: Mushroom, vomiting (PubMed Search)
Posted: 8/22/2013 by Fermin Barrueto
(Updated: 2/3/2026)
Click here to contact Fermin Barrueto
We will all see a patient that comes into the Emergency Department stating they have ingested some wild or self-picked mushrooms. Usually they will be actively vomiting and there will be no mushroom to identify. If there is, identification may still be difficult. There are no other clinical relevant symptoms that you can see until its too late. Amanita species is lethal and may require liver transplant. The most important question you can ask after trying to identify the mushroom is:
When did you eat the mushroom and how long after did the vomiting start?
As a general rule (with some exceptions), Amanita species cause vomiting and diarrhea in a delayed fashion 5-6 hours after ingestion. The other non hepatotoxic species usually cause vomiting within 1-3 hours.
Immediate vomiting <6 hrs from time of ingestion is good (usually).
Category: International EM
Posted: 8/21/2013 by Walid Hammad, MD, MBChB
Click here to contact Walid Hammad, MD, MBChB
General Information:
·You must know the diagnosis to deliver effective and high quality care to patients; likewise for health systems to be effective, it is necessary to understand what the global burden of disease is.
·In 1991, the World Bank and World Health Organization launched the Global Burden of Disease Study which as of 2010 evaluates 291 disease and injuries as well as 1160 sequelae of these causes.
·In order to compare the burden of one disease with that of another, you must consider death and life expectancy of persons affected by the disease as well as disability imposed by the condition.
·The combined composite summary metric is termed disability adjusted life years (DALYs).
·There have been three major worldwide studies to date (1990, 2005, 2010) attempting to quantify the burden of disease yet no study to date has ever attempted to quantify the burden of disease requiring emergent intervention.
Bottom Line:
DALYs are a useful tool for quantifying the burden of disease and provides essential input into health policy dialogues to identifies conditions and risk factors that may be relatively neglected and others for which progress is not what was expected. To date, there has been no rigorous scientific effort to quantify the burden of disease worldwide that requires emergent intervention to avoid death and disability.
University of Maryland Section of Global Emergency Health
Author: Emilie J. B. Calvello, MD, MPH
Christopher J.L. Murray, M.D., D.Phil., and Alan D. Lopez, Ph.D. Measuring the Global Burden of Disease. N Engl J Med 2013; 369:448-45
Category: Visual Diagnosis
Posted: 8/19/2013 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
Which echocardiographic view of the heart is this and can you name all 6 segments of the left ventricle? (Hint: A = Anteroseptal wall)
Parasternal short-axis view at the level of the papillary muscles
Category: Orthopedics
Keywords: Charcot Joints (PubMed Search)
Posted: 8/17/2013 by Michael Bond, MD
Click here to contact Michael Bond, MD
Charcot Joint - Neuropathic arthropathy
A Charcot Joint is a progressive degeneration of a weight bearing joint that is normally seen in patients that have decreased peripheral sensation and proprioception.
Conditions associated with Charcot Joints are:
• Alcohol neuropathy
• Cerebral palsy
• Diabetes mellitus
• Spinal Cord Injury
• Strokes
• Syphilis (tabes dorsalis)
The foot is most commonly affected and radiographs can also show bony destruction, bone resorption, and gross deformity. The onset of pain and deformity is typically insidious. Charcot joints are often associated with ulcerations, secondary osteomyelitis, and can lead to amputations.


It is important to recognize the presence of a Charcot Joint so that the patient can be referred to Orthopaedics and treated (often with cast immobilization) to prevent further destruction of the joint.
