Category: Toxicology
Keywords: pharmacology (PubMed Search)
Posted: 1/23/2014 by Fermin Barrueto
(Updated: 2/3/2026)
Click here to contact Fermin Barrueto
Everyone has admitted an altered mental status, patient or bradycardic patient and all of your test results are coming back normal except for a mild increase in creatinine. Take a look at the medication list. Creatinine is a poor indicator of renal function and GFR may be severely impaired even with a mild elevation of creatinine. If you have a predominantly renally excreted drug, you can see toxic effects of a drug even if administered at therapeutic levels.
Common bradycardia inducing medication that is renally cleared: atenolol (very high renal excretion) and digoxin (70%).
Altered Mental Status and on Keppra? Keppra is 100% renally cleared!
Ask your pharmacist for help with the medication list with renal or hepatic insufficiency.
Category: International EM
Keywords: International, snake, venom, (PubMed Search)
Posted: 1/22/2014 by Andrea Tenner, MD
Click here to contact Andrea Tenner, MD
98% of venomous snake bites in the US are due to pit vipers. Occasionally a snake bite is from an exotic venomous snake being kept as a pet. In 2005, 142 exotic poisonous snakes were reported to poison control. It can be very challenging to find antivenom for these exotic animals.
Antivenom is usually specific to a family or subfamily, so the snake must be identified. Most exotic snake owners will know the common name and possibly the scientific name of the animal.
The WHO database of venomous snakes can help with identification of the species and will list antivenom available globally.
Poison centers are essential to help locate the antivenom and assist with treatment.
Relevance to the EM Physician:
When a patient presents with an exotic snake envenomation, the WHO website below can be helpful to identify the species and possible antivenom.
http://apps.who.int/bloodproducts/snakeantivenoms/database/
University of Maryland Section of Global Emergency Health
Author: Jenny Reifel Saltzberg
C Lubich and EP Krenzelok. Exotic snakes are not always found in exotic places: how poison centres can assist emergency departments.” Emerg Med J. 2007 November; 24(11): 796–797.
Melisa W. Lai, et al. 2005 Annual Report of the American Association of Poison Control Centers’ National Poisoning and Exposure Database. Clinical Toxicology, 44:803–932, 2006
http://www.who.int/neglected_diseases/diseases/snakebites/en/index.html
Category: Critical Care
Keywords: arterial line, catheter related blood stream infections (PubMed Search)
Posted: 1/20/2014 by John Greenwood, MD
(Updated: 1/21/2014)
Click here to contact John Greenwood, MD
Arterial Catheter-Related Blood Stream Infections
Whether arterial lines are a potential source of catheter-related blood stream infections (CRBSIs) is highly-debated; however, based on a recent systematic review they are an under recognized and significant source of CRBSIs.
Bottom Line(s)
Follow me on twitter @medicalgraffiti
Category: Visual Diagnosis
Posted: 1/20/2014 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
50 year-old male intubated for respiratory distress. Ultrasound is used post-intubation to confirm tube placement and the following images are obtained. What's the diagnosis?
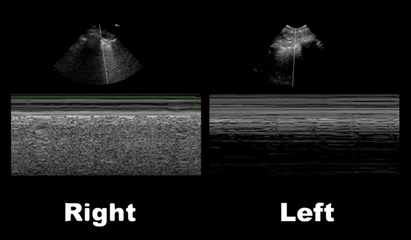
Right main-stem intubation as demonstrated by presence of lung-pulse on the left side
Lung-Pulse
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Cardiology
Posted: 1/19/2014 by Semhar Tewelde, MD
Click here to contact Semhar Tewelde, MD
Pacing Atrioventricular Block
- Atrioventricular (AV) block is classically treated with restoration of heart rate via right ventricular pacing, however high rates of right ventricular pacing is associated w/ left ventricular systolic dysfunction
- A recent multi-center randomized control trial (RCT) assessed the efficacy of right vs biventricular pacing in heart failure w/ AV block [BLOCK HF Trial]
- Primary outcomes of: morbidity, mortality, and adverse left ventricular remodeling were shown to be significantly lower in biventricular vs right ventricular pacing
- In patients with a high rate of pacing and/or an abnormally low left ventricular ejection fraction biventricular pacing may be more advantageous than conventional right ventricular pacing
Curtis A.B., Worley S.J., Adamson P.B.,et al: Biventricular pacing for atrioventricular block and systolic dysfunction. N Engl J Med 2013; 368: 1585-1593
Category: Misc
Keywords: Postoperative, fever, cause (PubMed Search)
Posted: 1/18/2014 by Michael Bond, MD
(Updated: 2/3/2026)
Click here to contact Michael Bond, MD
Post Operative Fever is extremely common, and with the increase in same day surgery this is a common complaint presenting to the ED. The mnemonic "5Ws" are often taught to remember the causes. They are:
Though many surgical textbooks report that atelectasis is the most common cause of early post-operative fever, some even claiming that it is responsible for over 90% of febrile episodes in the first 48 hours after surgery; a recent review in CHEST (reference below) showed that there is no evidence to support this. We often see atelectasis in medical patients too, and few if any of them have fever. The CHEST review found that there was no clear evidence that atelectasis causes fever at all.
Pearl: Temperature >38.9C should raise concern for a true infection, where lower temperatures can be due to pulmonary embolism, DVT, drug fever, etc….
Mavros MN, Velmahos GC, Falagas ME.Atelectasis as a cause of postoperative fever: where is the clinical evidence? Chest. 2011 Aug;140(2):418-24. doi: 10.1378/chest.11-0127. Epub 2011 Apr 28. Review. PMID: 21527508
Category: Pediatrics
Keywords: hyponatremia, maintenance fluid (PubMed Search)
Posted: 1/17/2014 by Jenny Guyther, MD
(Updated: 2/3/2026)
Click here to contact Jenny Guyther, MD
Wang et al. Isotonic Versus Hypotonic Maintenance IV Fluids in Hospitalized Children: A Meta-Analysis. Pediatrics 2014; 133;105.
Category: International EM
Keywords: influenza, China, Asia, Avian, Swine, Global (PubMed Search)
Posted: 1/12/2014 by Andrea Tenner, MD
(Updated: 1/15/2014)
Click here to contact Andrea Tenner, MD
General Information:
The H’s and N’s refer to hemagglutinin and neuraminidase—two proteins on the surface of the Influenza A virus that help it attach. Here’s a quick breakdown of important emerging strains of influenza:
Avian flu:
Swine flu:
Relevance to the EM Physician:
As the frontline against the flu virus, we should know what to expect. H1N1 has predominated this flu season—so far 60% of hospitalizations occurred in patients aged 18-64, which is unusual. H7N9 is new on the scene but might be imported, and H5N1 has arrived.
Bottom Line:
Expect to see more severe illness in the 18-64 y/o age group due to H1N1. Watch for more deadly flu imports--obtain a travel history and notify the CDC of severe influenza-like illness in returned travellers.
University of Maryland Section of Global Emergency Health
Author: Andi Tenner, MD, MPH, FACEP
http://www.cdc.gov/flu/avianflu/h5n1-people.htm
http://www.cdc.gov/flu/weekly/summary.htm
http://www.cdc.gov/flu/avianflu/h7n9-virus.htm
Category: Critical Care
Keywords: brain death (PubMed Search)
Posted: 1/14/2014 by Feras Khan, MD
Click here to contact Feras Khan, MD
Determination of Brain Death
Clinical Examination
If apnea testing cannot be performed due to instability, hypoxia, or cardiac arrhythmias, then a confirmatory test should be performed (from highest to lowest sensitivity):
There is state to state variation on who can perform the test and how many separate examinations need to be performed before brain death can be legally declared.
For a great review on some of the pitfalls in making the diagnosis and difficulties with the examination, please see the attached article.
Category: Visual Diagnosis
Posted: 1/13/2014 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
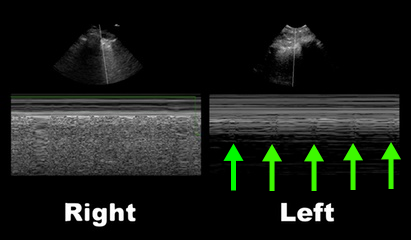
42 year-old male s/p assault complains of right sided facial pain, swelling, and decreased vision. Physical exam reveals subconjunctival hemorrhage, proptosis, afferent pupillary defect, and a firm globe. What's the diagnosis and what's the emergent treatment?

Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Cardiology
Keywords: PVC, Premature ventricular beats, Premature ventricular complexes (PubMed Search)
Posted: 1/12/2014 by Ali Farzad, MD
(Updated: 3/10/2014)
Click here to contact Ali Farzad, MD
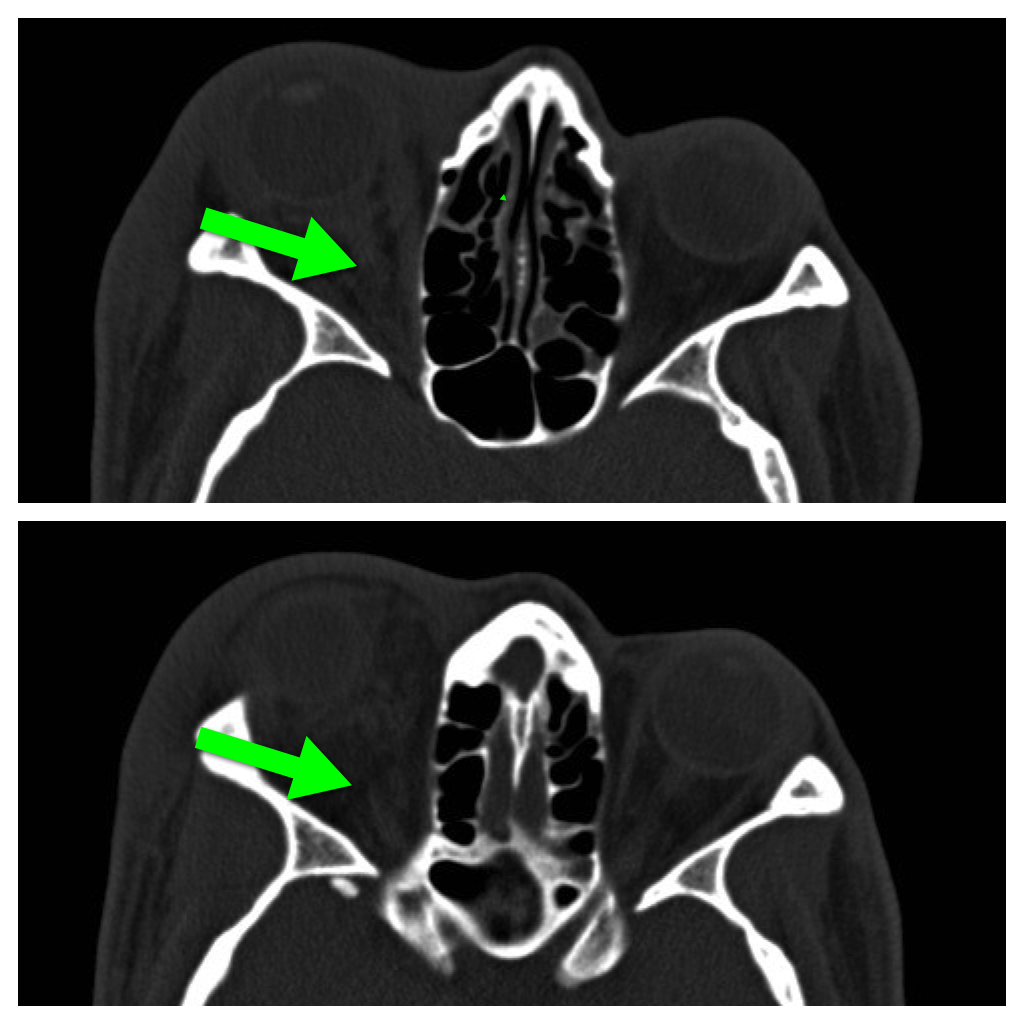
Differentiation between right and left ventricular origin of premature beats can be useful clinically.
PVCs arising from the right ventricle have a left bundle branch block morphology (dominant S wave in V1)
PVCs arising from the left ventricle have a right bundle branch block morphology (dominant R wave in V1)
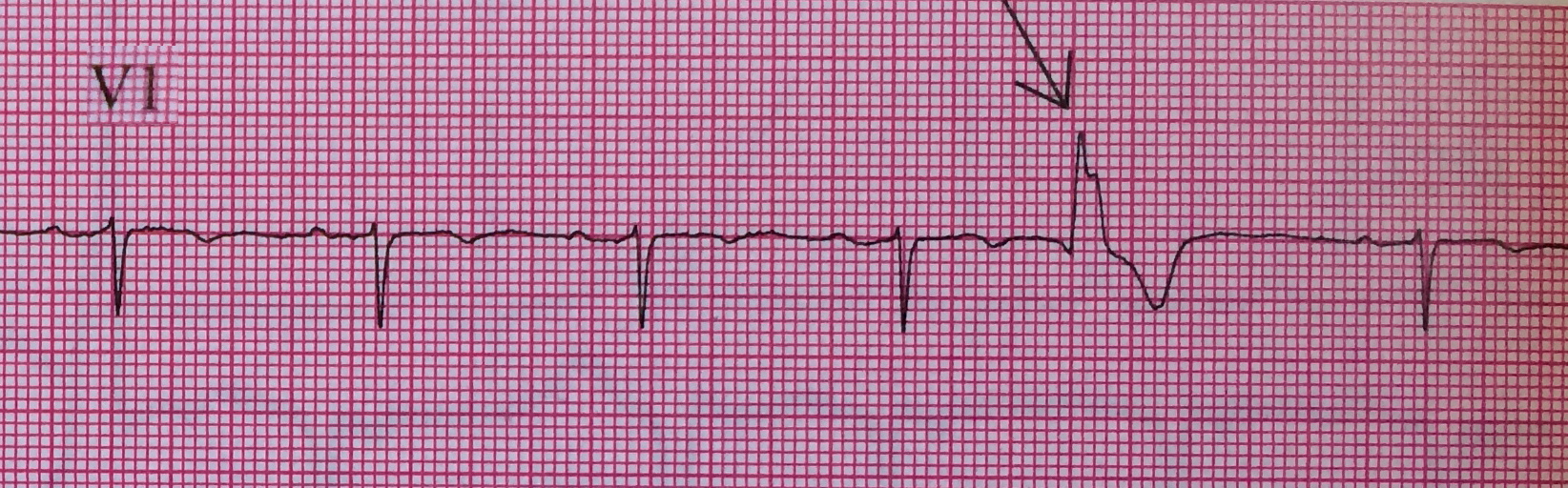
Left Ventricular premature beats are more often associated with heart disease and may precipitate ventricular fibrillation, whereas right ventricular premature beats are commonly seen in individuals with normal hearts.
Want more emergency cardiology pearls? Follow me @alifarzadmd
Wagner, Galen. Chapter 15 - Premature Beats. Marriott's Practical Electrocardiography, 12th Edition. 2013
Category: Orthopedics
Keywords: Osteoarthritis, treatment (PubMed Search)
Posted: 1/11/2014 by Brian Corwell, MD
Click here to contact Brian Corwell, MD
Chronic OA Management, Marc C. Hochberg. Volume 3 December 2013
Category: Toxicology
Keywords: copperhead, snake, envenomation, antivenin, crotalinae, fasciotomy (PubMed Search)
Posted: 1/7/2014 by Bryan Hayes, PharmD
(Updated: 1/9/2014)
Click here to contact Bryan Hayes, PharmD
Current evidence does not support the use of fasciotomy or dermotomy following North American Crotalinae envenomation with elevated intracompartmental pressures. [1]
A new case report of a 17-month old bitten by a copperhead snake reinforces that early and adequate administration of crotaline Fab antivenin is the treatment of choice. [2]
Many experts recommend against measuring compartement pressures altogether; we know it will be elevated.
Follow me on Twitter (@PharmERToxGuy)
Category: International EM
Keywords: MRSA, Vaccine, Staphylococcus (PubMed Search)
Posted: 1/8/2014 by Andrea Tenner, MD
Click here to contact Andrea Tenner, MD
Background Information:
Infections by Staphylococcus aureus cause significant morbidity and mortality around the world, but up until now no effective vaccines have been developed. Some prior attempts at vaccination actually led to higher mortality in the vaccinated group. However, a group at University of Iowa developed a vaccine targeting S. aureus virulence factors that has shown promise in animal models.
Pertinent Study Design and Conclusions:
Bottom Line:
While not available for human use yet, this is the first promising vaccine against S. aureus infections (including MRSA). Stay tuned…
University of Maryland Section of Global Emergency Health
Author: Andi Tenner, MD, MPH, FACEP
Spaulding AR, Salgado-Pabon W, Merriman JA, et al. Vaccination against Staphylococcus aureus pneumonia. J Infect Dis. First published online Dec. 19, 2013 doi:10.1093/infdis/jit823.
Category: Misc
Keywords: Frostbite (PubMed Search)
Posted: 1/7/2014 by Michael Bond, MD
Click here to contact Michael Bond, MD
Category: Critical Care
Posted: 1/7/2014 by Mike Winters, MBA, MD
(Updated: 2/3/2026)
Click here to contact Mike Winters, MBA, MD
Pearls for the Crashing LVAD Patient
Pratt AK, et al. Left ventricular assist device management in the ICU. Crit Care Med 2013; 42:158-168.
Follow me on Twitter (@critcareguys)
Category: Visual Diagnosis
Posted: 1/6/2014 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
37 year-old male presents after sustaining a burn from a pot of boiling water. He states that his skin started to blister a few hours after and it’s quite painful. What type of burn does he likely have?

A non-circumferential, superficial partial-thickness burn; it was treated with Silvadene (silver sulfadiazine)
Burn Classification:

Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Tintinalli, Judith E. (2010). Emergency Medicine: A Comprehensive Study Guide (Emergency Medicine). New York: McGraw-Hill Companies. pp. 1374–1386.
Category: Pediatrics
Keywords: Pediatrics, head lice (PubMed Search)
Posted: 1/6/2014 by Danielle Devereaux, MD
(Updated: 2/3/2026)
Click here to contact Danielle Devereaux, MD
Head lice infestation is a common problem in the United States with treatment costs estimated at 1 billion dollars and cases affecting millions of children each year. Many of these children present to the ED for care...lucky us! Traditional therapies containing permethrin and pyrethrins are having increased rates of treatment failure likely secondary to increasing resistance and medication noncompliance. The typical first line agents require multiple doses. There are safety concerns regarding therapies that contain malathion and lindane in children. Is there another option? Topical ivermectin 0.5% lotion applied to scalp in a single dose has been shown to be effective and safe for treatment of head lice infestation in children older than 6 months. It was FDA approved at the end of 2012. Considerations include cost. Sklice lotion is expensive!
The NEJM article was considered an "editors pick" by the AAP as one of the best articles of 2012-2013.
1. Pariser DM, Meinking TL, Bell M, et al. Topical 0.5% ivermectin lotion for treatment of head lice. N Eng J Med. 2012; 367(18):1687-1693
2. Wright, T. Topical Ivermectin: a new treatment for head lice. AAP Grand Rounds, Feb 2013, Vol 29(2)
3. Frankowski BL, et al. Head Lice. Pediatrics. 2010; 126:392-404
4. Meinking TL, et al. Head Lice. Pediatric Dermatology. 2010; 27(1):19-24
Category: Cardiology
Posted: 1/5/2014 by Semhar Tewelde, MD
Click here to contact Semhar Tewelde, MD
Assessment of Intermediate Coronary Lesions
- Coronary angiography alone to assess CAD is fraught with subjectivity
- Fractional flow reserve (FFR) has become the standard to assess/quantify obstructive CAD; it determines the myocardial flow in the presence of stenosis identifying the lesion responsible for ischemia
- FFR assesses focal stenosis, but does not consider diffuse atherosclerotic narrowing or microcirculatory dysfunction as contributors of ischemic heart disease
- An index of microcirculatory resistance (IMR) can be concomitantly measured with FFR during cardiac catheterization to specifically evaluate the microvasculature
- Coronary flow reserve (CFR) was the 1st proposed method for assessment of intermediate coronary lesion, but proved suboptimal because of its variability especially in patients with microvascular dysfunction (diabetes, prior MI, etc.)
- Utilization of FFR, IMR, and CFR together support the existence of differentiated patterns of ischemic heart disease & may help to determine future ischemic events
Echavarria-Pinto M, Escaned J, Macias E, et al. Disturbed Coronary Hemodynamics in Vessels With Intermediate Stenosis Evaluated With Fractional Flow Reserve: A Combined Analysis of Epicardial and Microcirculatory Involvement in Ischemic Heart Disease. Circulation Volume 128(24), 17 December 2013, p 2557–2566
Category: Pharmacology & Therapeutics
Keywords: droperidol, QT prolongation (PubMed Search)
Posted: 12/31/2013 by Bryan Hayes, PharmD
(Updated: 8/15/2014)
Click here to contact Bryan Hayes, PharmD
46 patients treated with high-dose droperidol (10-40 mg) were studied prospectively with continuous holter recording.
What they did
Patients initially received 10 mg droperidol as part of a standardized sedation protocol (for aggression). An additional 10 mg dose was given after 15 min if required and further doses at the clinical toxicologist's discretion.
Continuous 12-lead holter recordings were obtained for 2-24 hours. QTc > 500 msec was defined as abnormal (with heart rate correction - QTcF).
What they found
Only 4 patients had abnormal QT measurements, three given 10 mg and one 20 mg. All 4 had other reasons for QT prolongation. No patient given > 30 mg had a prolonged QT. There were no dysrhythmias.
What it means
There was little evidence supporting droperidol being the cause and QT prolongation was more likely due to pre-existing conditions or other drugs.
Calver L, et al. High dose droperidol and QT prlongation: analysis of continuous 12-lead recordings. Br J Clin Pharmacol. 2014;77(5):880-6. [PMID 24168079]
Follow me on Twitter (@PharmERToxGuy)
