Category: Critical Care
Posted: 6/24/2014 by Mike Winters, MBA, MD
(Updated: 2/27/2026)
Click here to contact Mike Winters, MBA, MD
Prophylactic FFP for Procedures?
Category: Visual Diagnosis
Posted: 6/22/2014 by Haney Mallemat, MD
(Updated: 6/23/2014)
Click here to contact Haney Mallemat, MD
35 year-old female presents with nausea and vomiting 1 week post-op for an abdominal surgery. Abdominal ultrasound is below; what's the diagnosis?
Small bowel obstruction (SBO)
Ultrasound for Small bowel obstruction (SBO)
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Orthopedics
Keywords: knee, injury, dislocation (PubMed Search)
Posted: 6/21/2014 by Michael Bond, MD
(Updated: 2/27/2026)
Click here to contact Michael Bond, MD
Some quick facts about Knee Injuries:
Category: Pediatrics
Keywords: Ultrasound, pediatrics, appendicitis (PubMed Search)
Posted: 6/20/2014 by Jenny Guyther, MD
Click here to contact Jenny Guyther, MD
Category: Toxicology
Keywords: NAC, acetaminophen (PubMed Search)
Posted: 6/19/2014 by Hong Kim, MD
Click here to contact Hong Kim, MD
NAC is an effective antidote against acetaminophen (APAP) toxicity in preventing acute hepatotoxicity. It provides cysteine that is essential for glutathione synthesis and its availability is rate limiting.
Currently, PO and IV formulation is available in the U.S. Regardless of the route, NAC is equally effective in preventing APAP induced acute hepatotoxicity when administered within 8 hours after single acute ingestion. 1
Adverse effects of NAC
1. Anaphylactoid reaction
a. More frequently reported with IV administration and during the first regimen of NAC (150 mg/kg over 60 min) administration. (dose and rate dependent)
b. Higher risk of anaphylactoid reaction in patients with negative APAP vs. patients with elevated APAP level.2
c. Management: Benadryl as needed and slow infusion rate.
2. Hyponatremia in children if inappropriate volume of diluent (D5W) used. Dose calculator: http://acetadote.com/dosecalc.php
3. Laboratory: increase Prothrombin time (PT).3
4. Fatality from iatrogenic NAC overdose has been reported.
Advantage of IV NAC
1. Convenience
2. 100% bioavailability
3. Shorter hospital length of stay
4. Minimum GI symptoms (nausea & vomiting) compared to PO route
Indication of IV NAC
1. Severe hepatotoxicity or fulminant liver failure
2. APAP poisoning during pregnancy
3. Unable to tolerate PO intake (nausea, vomiting, altered mental status)
However many clinicians administer IV NAC for their advantages over PO NAC.
Take home message:
1. PO and IV NAC are equally effective when administered within 8 hours after single acute ingestion.
2. Anaphylactoid reaction is frequently encountered AE during the infusion of 1st NAC regimen and patients with negative/low APAP level may be at higher risk.
3. No emergent need to start NAC in presumed acetaminophen overdose patients prior to obtaining APAP level.
Category: International EM
Keywords: Schistosomiasis, parasites, international (PubMed Search)
Posted: 6/18/2014 by Andrea Tenner, MD
Click here to contact Andrea Tenner, MD
Clinical Presentation:
A 35-year-old female presents to your emergency department complaining of fever, malaise, myalgias, headache and an urticarial rash. Her physical exam reveals a papular rash and hepatosplenomegaly. You also find out that she traveled to Sudan 6 weeks earlier. She stayed mostly in Kharotum, but while there, she swam in the Nile. You send a smear for malaria, which is negative. What other major parasite should you consider?
Diagnosis:
Discussion:
While the acute presentation is generally non-specific, chronic complications may be more serious. Many organ systems can be impacted and symptoms of chronic infection can include liver dysfunction, including portal hypertension and esophageal varacies or hematuria and renal failure.
Treatment:
Bottom Line:
Consider a broader differential in travelers. There are many infectious killers that can be easily treated.
University of Maryland Section of Global Emergency Health
Author: Jon Mark Hirshon, MD, MPH, PhD
Category: Critical Care
Keywords: Thrombelastography, TEG, ROTEM, Hemorrhagic Shock (PubMed Search)
Posted: 6/13/2014 by John Greenwood, MD
Click here to contact John Greenwood, MD
Thrombelastography for Management of Non-Traumatic Hemorrhagic Shock
The use of thrombelastography (TEG, ROTEM) has traditionally been utilized and studied in the management of acute coagulopathy of trauma (ACoT) developed by patients in hemorrhagic shock secondary to trauma.
Functional coagulation tests such as the TEG may provide valuable information when resuscitating the hemorrhaging patient, especially if there is any concern for an underlying coagulopathy.
The following is a TEG recently returned during the resuscitation of a 60 y/o male with a history of HCV cirrhosis presenting with hemorrhagic shock secondary to a massive upper GIB. The University's Massive Transfusion Protocol was promptly activated and at this point, the patient had received approximately 4 units of PRBCs & FFP along with 1 liter of crystalloid. His Hgb was 5, PT/PTT/INR were undetectable, and his fibrinogen was 80.
Below is a table that simplifies the treatment, based on the test's abnormalities:
After reviewing the initial TEG, all perameters were abnormal in addition to the presence of significant fibrinolysis. The patient was given an additional 4 units of FFP, DDAVP, cryoprecipitate, a unit of platelets, and aminocaproic acid. The patient still required significant resuscitation, however bleeding had significantly decreased as well has his pressor requirement. Below is the patient's follow-up TEG 2 hours later.
There is growing enthusiasm for the use of functional coagulopathy testing in the patient with hemorrhagic shock. Early resuscitation with blood products as your fluid of choice with limited fluid administration while arranging for definitive source control are critical, but also consider early thrombelastography to detect additional causes for uncontrolled hemorrhage.
References
Follow Me On Twitter: @JohnGreenwoodMD
email: johncgreenwood@gmail.com
Category: Visual Diagnosis
Posted: 6/15/2014 by Haney Mallemat, MD
(Updated: 6/16/2014)
Click here to contact Haney Mallemat, MD
41year-old male without past medical history presents with the image below. What's the diagnosis and what's the most likely causative organism?

Gram-Negative web-space infection; most common etiologic organism is Pseudomonas
Gram Negative Web-space Infections
Gram-negative infections may occur in toe web-spaces of healthy patients, especially in areas with hyperhidrosis (excessive perspiration) and macerated skin.
Common organisms include Pseudomonas; others include Corynebacterium minutissimum (causes erythrasma, chronic superficial infection of the intertriginous areas of the skin), and other gram-negative bacteria
Woods-light examination may be clinically helpful if Pseudomonas is suspected (fluoresce green) and erythrasma will fluoresce coral red. KOH direct examination for fungal elements may show the presence of dermatophytes or Candida.
Treatment:
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Wolff, K., & Johnson, R. J. (2009). Fitzpatrick's Color Atlas and Synopsis of Clinical Dermatology. (6th ed., pp. 662-664;698). McGraw-Hill.
http://www.aafp.org/afp/2005/0901/p833.html
http://emedicine.medscape.com/article/1055306-overview
Category: Toxicology
Keywords: methadone, QTc, overdose (PubMed Search)
Posted: 6/9/2014 by Bryan Hayes, PharmD
(Updated: 6/21/2014)
Click here to contact Bryan Hayes, PharmD
Methadone prolongs the QTc interval. Is the degree of QTC widening correlated to worse outcomes after overdose?
The authors of a new study concluded the triage QTc can predict death, intubation, and respiratory arrest. QTc thresholds of 470, 447.5, and 450 msec had sensitivity (95 % CI) and specificity (95 % CI) of 87.5 (47.3-99.7), 86.8 (74.7-94.5), and 77.3 (62.2-88.5), respectively.
My Thoughts
Respiratory depression is the predominant cause of death in methadone overdoses. QTc interval prolongation may have the potential to help predict outcomes, but the QTc thresholds in this study were really not that prolonged. Patients on chronic methadone without overdose have baseline QTc intervals longer than those in this study after overdose.
Application to Clinical Practice
Many factors contribute to the ultimate disposition of methadone overdose cases. Even if QTc widening is correlated to outcomes, it really won't change our management.
Farsi D, et al. The correlation between prolonged corrected QTc interval with the frequency of respiratory arrest, endotracheal intubation, and mortality in acute methadone overdose. Cardiovasc Toxicol 2014 May 9. [Epub ahead of print] [PMID 24811951]
Follow me on Twitter (@PharmERToxGuy) or Google Plus (+bryanhayes13)
Category: International EM
Keywords: Malaria, International, Travel, fever (PubMed Search)
Posted: 6/11/2014 by Andrea Tenner, MD
Click here to contact Andrea Tenner, MD
Case Presentation:
A 64 yo male with a history of IDDM presents with generalized fatigue. He felt so weak last night that he missed his pm dose of Lantus and vomited this morning. He arrived with a critically elevated BG of 590. He flew to the US from Sierra Leone 3 days ago.
Labs include:
Wbc 3.5 Plt 34 Hb 12 Hct 36
Na 125 CL 93 Co2 14 K 4.5 BUN 25 Cr 1.9 Glu 590 AG 18
VBG pH 7.23
Clinical Question:
Other than treating his diabetic ketoacidosis and renal failure, would you send any further tests?
Answer:
Thick smear for Malaria.
Bottom Line:
University of Maryland Section of Global Emergency Health
Author: Bradford Schwartz, MD
Ansari, Khoharo, Akhund, and Qureshi. Thrombocytopenia in plasmodium falciparum malaria.J Ayub Med Coll Abbottabad. 2009 Apr-Jun;21(2):145-7.
Kumar and Shashirekha. Thrombocytopenia--an indicator of acute vivax malaria. Indian J Pathol Microbiol. 2006 Oct;49(4):505-8.
Lacerda, Mourao, Coelho, and Santos. Thrombocytopenia in malaria: who cares? Mem Inst Oswaldo Cruz. 2011 Aug;106 Suppl 1:52-63.
Category: Critical Care
Posted: 6/10/2014 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Visual Diagnosis
Posted: 6/8/2014 by Haney Mallemat, MD
(Updated: 6/9/2014)
Click here to contact Haney Mallemat, MD
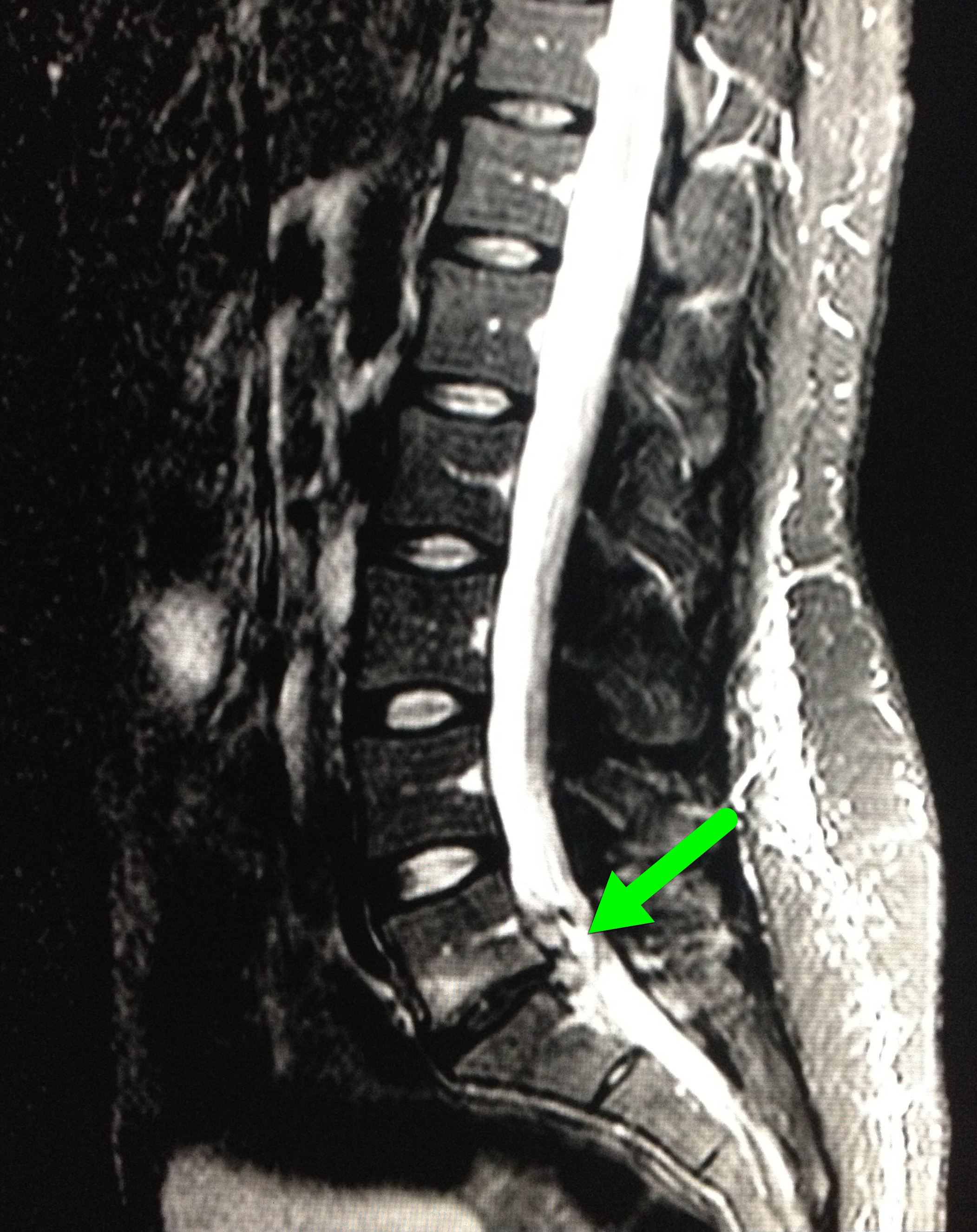
28 year-old female with history of chronic back pain presents with right-foot numbness and inability to move her foot at the ankle joint. What’s the diagnosis and what neurologic finding would you expect to find?

Large disc bulge at L5-S1
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Pharmacology & Therapeutics
Keywords: cellulitis, antibiotic, outpatient (PubMed Search)
Posted: 5/31/2014 by Bryan Hayes, PharmD
(Updated: 8/15/2014)
Click here to contact Bryan Hayes, PharmD
In a prospective cohort of 598 ED patients, 5 risk factors were independently associated with uncomplicated cellulitis patients who fail initial antibiotic therapy as outpatients and require a change of antibiotics or admission to hospital:
Patients presenting with uncomplicated cellulitis and any of these risk factors may need to be considered for observation +/- IV antibiotics.
Peterson D, et al. Predictors of Failure of Empiric Outpatient Antibiotic Therapy in Emergency Department Patients with Uncomplicated Cellulitis. Acad Emerg Med 2014; 21(5):526-31. [PMID 24842503]
Follow me on Twitter (@PharmERToxGuy) and Google Plus (+bryanhayes13)
Category: Toxicology
Keywords: lidocaine, bupivacaine (PubMed Search)
Posted: 6/5/2014 by Fermin Barrueto
(Updated: 2/27/2026)
Click here to contact Fermin Barrueto
This is a must memorize simple table of the toxic doses of local anesthetics. Toxicity of local anesthetics starts with slurred speech, lethargy to seizures and lethal cardiac dysrhythmias. There should be zero tolerance to actual cause toxicity when repairing a laceration or performing a fascia iliaca block.
Remember that a Bupivcaine solution 0.5% = 0.5 g/dL (%=g/dL) so a 70kg person, you can use a maximum of 2mg/kg x 70kg person. You can inject 140 mg in a 70kg person. This is a maximum volume injection of 28 mL if you were doing a fascia iliaca block. You can double the volume if you use a more dilute solution of 0.25%.
| Local Anesthetic | mg/kg |
| Bupivacaine | 2 |
| Ropivacaine | 3 |
| Lidocaine | 4 |
| Lidocaine with Epinephrine | 6 |
| Prilocaine | 6 |
Treatment for cardiac dysrhythmias due to local anesthetics is 20% lipid emulsion therapy - don't follow ACLS protocol as epinephrine or other antidysrhythmics (especially lidocaine) will be lethal.
Category: International EM
Posted: 6/4/2014 by Walid Hammad, MD, MBChB
Click here to contact Walid Hammad, MD, MBChB
General Information:
This year there have been over 280 cases of measles in the US, spanning 18 states; early recognition is key to preventing transmission.
Remember the 3 c's for recognition:
Cough, Coryza (runny nose), Conjunctivitis + febrile rash
-Incubation period is 10-12 days
-Symptoms usually start with fever, followed by rash 2-3 days later starting from the hairline and spreading to the trunk and extremities
-Completion of the first series of vaccines provides 90-95% immunity from measles
Relevance to the EM Physician:
-Immediately place any patient suspected of having measles on airborne precautions
-Look for koplik spots on the oral mucosa (commonly described as appearing like small grains of salt)
-Complications include diarrhea, otitis media, “measles croup,” pneumonia, encephalitis (1/1000 cases), and death (2-3/1000 cases)
-Post exposure prophylaxis (PEP) is recommended for unvaccinated exposed individuals and is effective up to 72 hours after exposure; however, vaccination is contraindicated in pregnant women
Bottom Line:
-The incidence of measles is rising sharply in the US. Vaccination, early detection, and post exposure prophylaxis for exposed individuals is key to reversing this trend.
University of Maryland Section of Global Emergency Health
Author: Bradford Schwartz, MD
1. CDC. Measles-January 1-May 23, 2014. MMWR 2014; 63;(1-4).
2. CDC. Prevention of Measles, Rubella, Congenital Rubella Syndrome, and Mumps, 2013: Summary Recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR 2013;62(RR04);1-34.
3. CDC. Measles Questions and answers. http://www.immunize.org/catg.d/p4209.pdf
4. CDC. Measles-Rubeola. http://www.cdc.gov/measles/index.html
5. Perry and Halsey. Clinical Significance of Measles: A Review. J Infect Dis. 2004 May 1;189 Suppl 1:S4-16.
Category: Critical Care
Keywords: bleeding, coagulopathy, dabigatran, PCC, (PubMed Search)
Posted: 6/3/2014 by Feras Khan, MD
(Updated: 2/27/2026)
Click here to contact Feras Khan, MD
Emergent reversal of Dabigatran
What is it:
Direct thrombin inhibitor used for stroke prevention in non-valvular atrial fibrillation
When do I worry about reversal:
Patients can have clinically important bleeding (GI hemorrhage, or Intracranial bleeding) or need reversal for emergent surgery
Patients with renal failure can have a prolonged medication effect
What can I do:
1. Activated charcoal: good for recent overdose or recent ingestion (within 2 hours)
2. Hemodialysis: around 60-65% can be removed within 2-4 hrs; putting in a dialysis line can be…bloody
3. FFP: in rat studies, has been shown to reduce the volume of intracranial hemorrhage. Unknown in humans. No good evidence of use based on coagulation mechanisms. Still worth a try though.
4. Recombinant activated factor VII: Has been shown to correct the bleeding time in animal studies. Probably the best bet in severe bleeding
5. Pro-thrombin complex concentrate: has been shown to decrease the bleeding time in animal studies
How do I monitor effect?
No great way here. Check aPTT and thrombin time (TT). At supra-therapeutic doses there is no good test.
Coming attractions: Dabigatran-fab for emergent reversal (see previous pearl: https://umem.org/educational_pearls/2415/)
Kaatz, S et al. Guidance on the emergent reversal of oral thrombin and factor Xa inhibitors. American Journal of Hematology. 2012.
Category: Visual Diagnosis
Posted: 6/2/2014 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
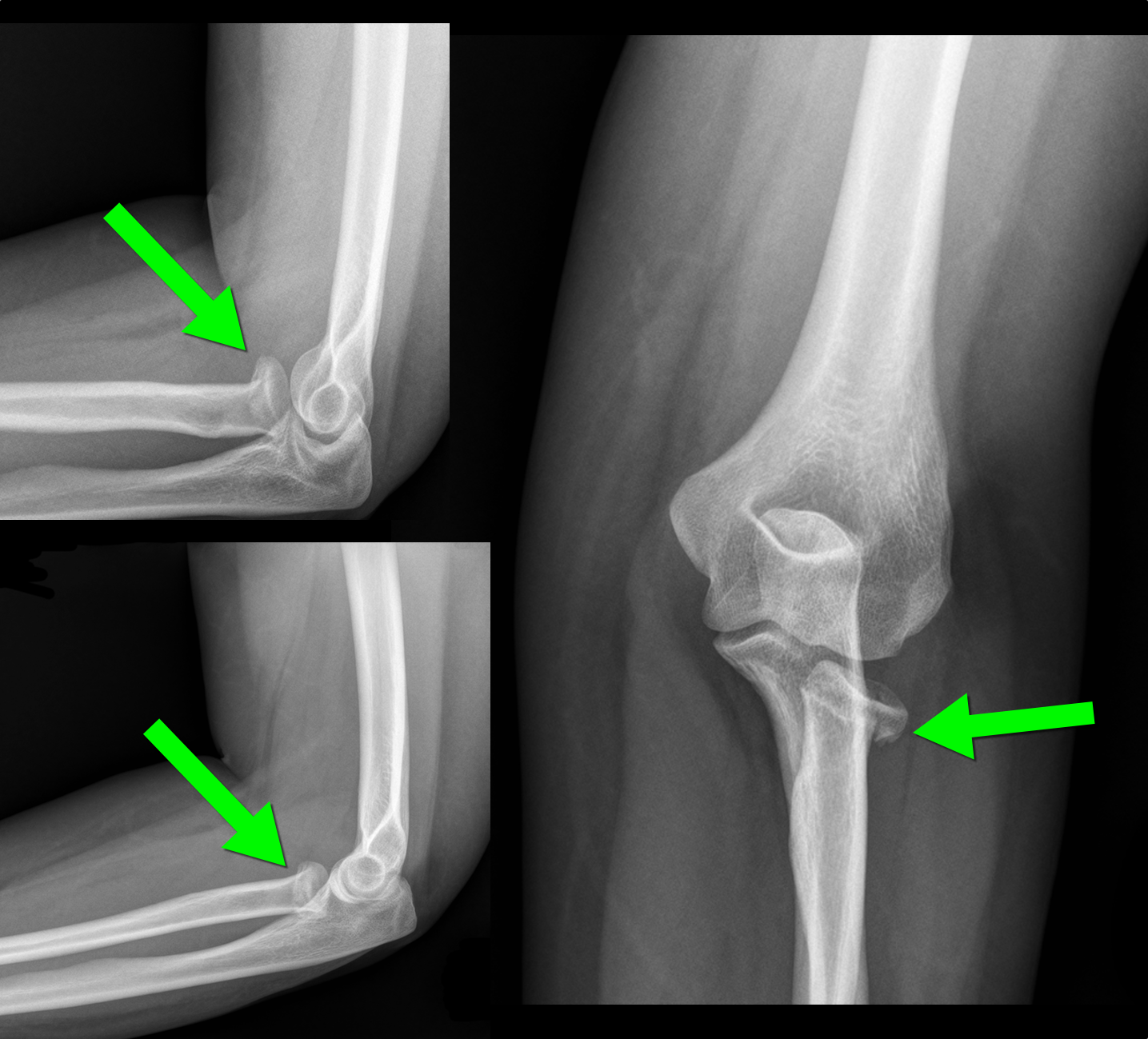
30 year-old female with elbow pain following a fall. What's the diagnosis? (bonus points if you name the fracture with an associated radio-ulnar joint dislocation)

Radial Head Fracture
 d
d
http://www.wheelessonline.com/ortho/radial_head_frx
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Orthopedics
Posted: 6/1/2014 by Michael Bond, MD
Click here to contact Michael Bond, MD
When examining a knee for a meniscal injury the commonly described tests are the McMurray Test and Apley Test. However, these tests have sensitivities of 48-68% and 41% respectfully, and specificities of 86-94% and 86-93% respectfully. Depending on whether you are looking at the medical or lateral meniscus.
The Thessaly Test that was first described in 2005 can be performed with knee in either 5 or 20 degrees of flexion and has a senstivity of 89-92% and specificity of 96-97% when performed in 20 degrees flexion. The test also tends to be easier to perform.
To perform the test:
Essentially you and your patient will look like you are doing the twist as they rotate their knee with you holding their hands.
A video of the technique can be found at http://youtu.be/R3oXDvagnic
The Journal of Bone and Joint Surgery (American). 2005;87:955-962.
Category: Toxicology
Keywords: seizure, overdose (PubMed Search)
Posted: 5/29/2014 by Fermin Barrueto
(Updated: 2/27/2026)
Click here to contact Fermin Barrueto
Seizure is a very common effect seen in many overdoses. Think about the following drugs which have a higher propensity for seizure as noted in a Swiss study of over 15000 patients and isolating to single drug overdoses:
The most prevalent pharmaceuticals were mefenamic acid (51 of the 313 cases), citalopram (34), trimipramine (27), venlafaxine (23), tramadol (15), diphenhydramine (14), amitriptyline (12), carbamazepine (11), maprotiline (10), and quetiapine (10).
The drug mefenanamic acid is not used much in the USA but citalopram, venlafaxine and tramadol as well as the most prelavent bupropion which was number one in the study are all commonly prescribed in the USA. Keep a watchful eye if you see any of these drugs on a drug list or as an overdose.
Category: International EM
Keywords: diarrhea, international, infectious disease, stool, parasite (PubMed Search)
Posted: 5/28/2014 by Andrea Tenner, MD
(Updated: 2/27/2026)
Click here to contact Andrea Tenner, MD
General Information:
Bottom Line for the EM Physician: Use these guidelines to test stool only when helpful to patient care and avoid flushing resources down the toilet.
University of Maryland Section of Global Emergency Health
Author: Alex Skog
DuPont HL. Acute infectious diarrhea in immunocompetent adults. N Engl J Med. 2014 Apr 17;370(16):1532–40.
Fischer Walker CL, Perin J, Aryee MJ, Boschi-Pinto C, Black RE. Diarrhea incidence in low- and middle-income countries in 1990 and 2010: a systematic review. BMC Public Health. 2012;12:220.
