Category: Critical Care
Posted: 9/2/2014 by Haney Mallemat, MD
(Updated: 10/1/2014)
Click here to contact Haney Mallemat, MD
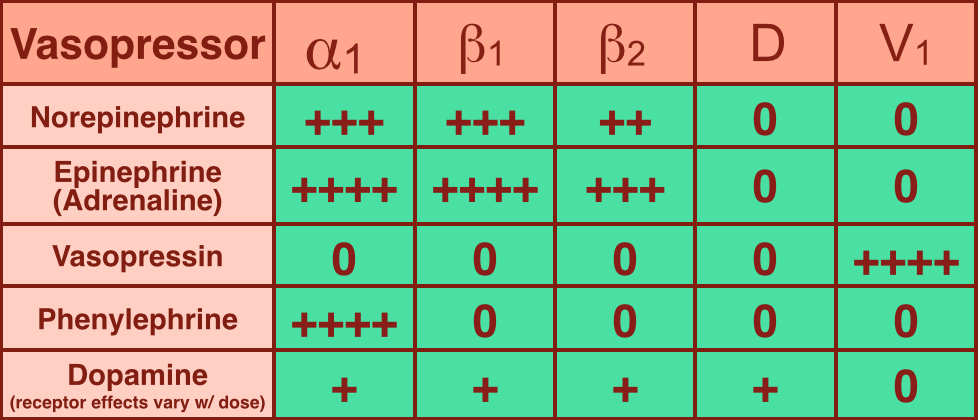
Vasopressors are used in shock-states to increase mean arterial pressure (MAP) and improve distal tissue perfusion. Additionally, some agents have effects on the heart to augment cardiac output.
Receptors that vasopressors work on include:
Norepinephrine (NE): excellent vasopressor for most types of shock and recommended as a first-line agent in the Surviving Sepsis Guidelines.
Epinephrine (a.k.a. Adrenaline): in several countries the first-line agent for shock (including sepsis).
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Visual Diagnosis
Posted: 9/1/2014 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
You are scaning the liver with ultrasound and you see this. What's the diagnosis?
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Cardiology
Keywords: Sick Sinus Syndrome (PubMed Search)
Posted: 8/31/2014 by Semhar Tewelde, MD
Click here to contact Semhar Tewelde, MD
Sick Sinus Syndrome
- Sick sinus syndrome (SSS) is a cardiac conduction disorder characterized by symptomatic dysfunction of the sinoatrial (SA) node.
- SSS usually manifests as sinus bradycardia, sinus arrest, or sinoatrial block, and is sometimes accompanied by supraventricular tachydysrhythmias.
- Symptoms of SSS include: syncope, dizziness, palpitations, exertional dyspnea, fatigability from chronotropic incompetence, heart failure, and angina.
- Clinically significant SSS typically requires pacemaker implantation. Approximately 30% to 50% of pacemaker implantation in the United States list SSS as the primary indication.
- 2 large, prospective cohorts with an average follow-up of 17 years, observed the incidence of SSS increases with age, does not differ between men and women, and is lower among blacks than whites.
- Risk factors for SSS included greater BMI & height, elevated NT-proBNP level & cystatin C level, longer QRS interval, lower heart rate, hypertension, and right bundle branch block.
Jensen P, Gronroos N, et al. Incidence of and Risk Factors for Sick Sinus Syndrome in the General Population. Journal of the American College of Cardiology. Vol 64 Issue 6, pages 531-538
Category: Orthopedics
Keywords: radiology, ankle, fracture (PubMed Search)
Posted: 8/30/2014 by Michael Bond, MD
Click here to contact Michael Bond, MD
Some radiology pearls concerning ankle pain and fractures courtesy of David Bostick and Michael Abraham
Maisonneuve fracture – fracture of the medial malleolus with disruption of the tibiofibular syndesmosis with associated fracture of the proximal fibular shaft (http://radiopaedia.org/articles/maisonneuve-fracture)
When to look for high fibular fracture
Always look for avulsion fracture of 5th metatarsal styloid in patients with ankle pain and
no obvious fractures
Dans-Weber Classification – for lateral malleolar fractures (http://radiopaedia.org/articles/ankle-fracture-classification-weber)
Category: Neurology
Keywords: basics, trauma, critical care (PubMed Search)
Posted: 8/28/2014 by Danya Khoujah, MBBS
(Updated: 2/3/2026)
Click here to contact Danya Khoujah, MBBS
Elevated intracranial pressure (ICP), defined as >20mmHg, is frequently encountered in patients with severe traumatic brain injury (TBI). A step-wise approach would include:
1. Analgesia and sedation: frequently forgotten.
2. Hyperosmolar agents: both hypertonic saline and mannitol can be used. Neither is superior.
3. Induced arterial blood hypocarbia using hyperventilation (must monitor for cerebral ischemia)
4. Barbiturates (last resort due to side effects)
5. Surgical:
a. CSF drain
b. Decompressive craniectomy: benefits challenged by the DECRA study
Stocchetti N, Maas AIR. Traumatic Intracranial Hypertension. N Engl J Med 2014; 370:2121-30.
Category: Critical Care
Keywords: immunonutrition, enteral feeding (PubMed Search)
Posted: 8/26/2014 by Feras Khan, MD
(Updated: 2/3/2026)
Click here to contact Feras Khan, MD
Background
Data
What to do
Category: Visual Diagnosis
Posted: 8/25/2014 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
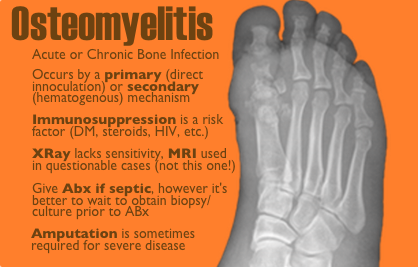
50 year-old female with diabetes complains of pain and discharge from a poorly healing wound. XRay below. What's the diagnosis?

Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Cardiology
Keywords: GRACE score (PubMed Search)
Posted: 8/24/2014 by Semhar Tewelde, MD
(Updated: 2/3/2026)
Click here to contact Semhar Tewelde, MD
GRACE Score
- The Global Registry of Acute Coronary Events (GRACE) is an international database tracking outcomes of patients presenting with acute coronary syndromes (ACS).
- GRACE score is calculated based on 8 variables: Age, HR, systolic BP, creatinine, killip class, ST-segment deviation on EKG, cardiac biomarkers, and cardiac arrest on admission.
- Several reports have shown that the GRACE score is a better predictor of clinical outcome (risk of death or the combined risk of death or myocardial infarction at 6 months) than the TIMI score.
- A recent study evaluated the relationship between GRACE score & severity of coronary artery disease (CAD) angiographically evaluated by Gensini score in patients with NSTE-MI.
- Results showed that the GRACE score has significant relation with the extent & severity of CAD as assessed by angiographic Gensini score.
- GRACE score was shown to be important both for determining the severity of the CAD and predicting death within 6 months of hospital discharge from NSTE-MI.
Cakar M, Sahinkus S, et al. Relation between the GRACE score and severity of atherosclerosis in acute coronary syndrome. Journal of Cardiology. 2014 Vol 63, Issue 1, Pgs 24-28.
Category: Orthopedics
Keywords: Jumpers knee, knee pain (PubMed Search)
Posted: 8/24/2014 by Brian Corwell, MD
(Updated: 2/3/2026)
Click here to contact Brian Corwell, MD
Patellar tendonitis aka jumpers knee
Activity related knee pain due to degenerative, micro injury rather than an inflammatory process
Up to 20% in jumping athletes
Anterior knee pain during or after activity
Bassett Sign:
a) Tenderness to palpation with knee in full extension (patellar tendon relaxed)
b) No tenderness with knee in flexion (patellar tendon tight)
Category: Toxicology
Keywords: e-cigarettes (PubMed Search)
Posted: 8/21/2014 by Fermin Barrueto
(Updated: 2/3/2026)
Click here to contact Fermin Barrueto
E-cigarette popularity has increased and with that another possible source of toxicity. The most recent MMWR shows how e-cigarette use has increased over the past 5 years. The general toxicity involves nicotine toxicity with nausea, vomiting, eye irritation as the major sources of toxicity. Only one reported death where the nicotine reservoir was accessed and then injected IV in a suicide attempt.
There are some reports of asthma exacerbations but is more likely due to the vapor flavor and not the nicotine.
Category: International EM
Keywords: hyperthermia, hypothermia, environmental, international (PubMed Search)
Posted: 8/12/2014 by Jon Mark Hirshon, MPH, MD, PhD
(Updated: 8/20/2014)
Click here to contact Jon Mark Hirshon, MPH, MD, PhD
General Background:
Heat transfer is important to understand, especially when evaluating and treating someone who is hyperthermic or hypothermic. Are they really hot (or cold) from exposure, or is there an underlying metabolic or toxicological cause?
Mechanisms of Heat Transfer:
There are 4 main methods of heat transfer:
Bottom line:
When evaluation someone for hyper- or hypothermia from a potential environmental exposure, be sure to obtain the history about where they were found and the circumstances in which they were found. This can help you develop your diagnostic differential.
Reference: Pathophysiology, management and complications of hypothermia. Lantry J, Dezman Z, Hirshon JM. Br J Hosp Med (Lond). 2012 Jan; 73(1):31-7.
Category: Critical Care
Posted: 8/19/2014 by Mike Winters, MBA, MD
(Updated: 2/3/2026)
Click here to contact Mike Winters, MBA, MD
Sepsis Pearls from the Recent Literature
Category: Visual Diagnosis
Posted: 8/18/2014 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
A critically-ill patient requires fluid resuscitation. Someone hands you a bag of this. What’s the pH of this fluid?
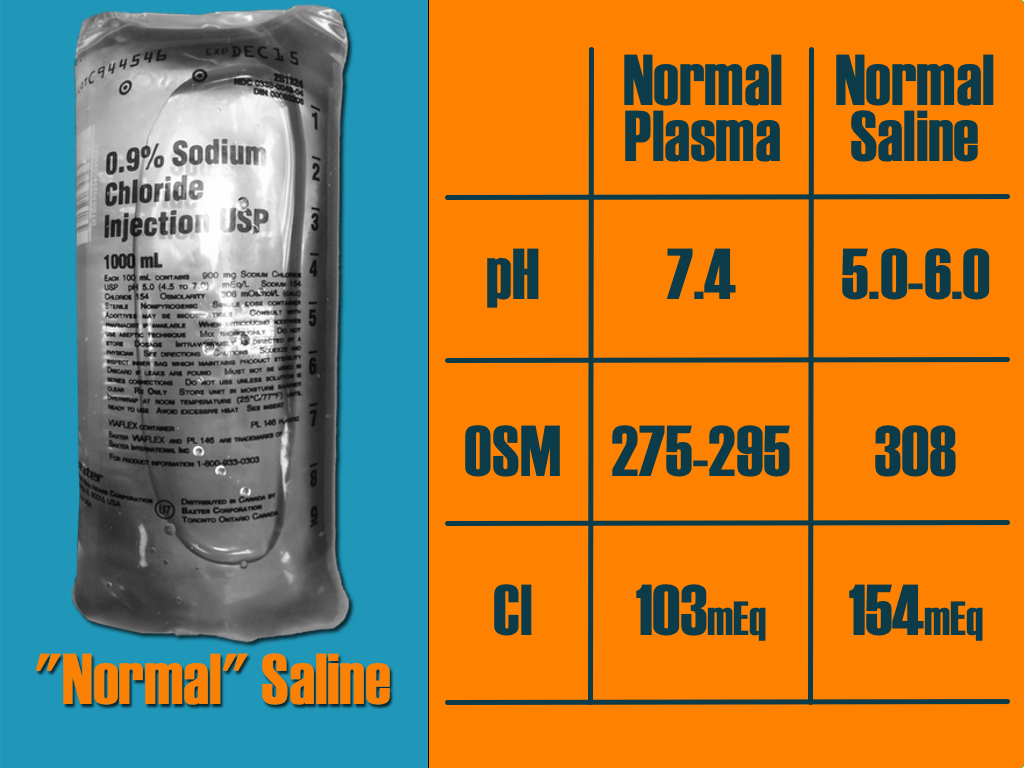
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Cardiology
Keywords: Nonatherosclerotic Coronary Artery Disease (PubMed Search)
Posted: 8/17/2014 by Semhar Tewelde, MD
(Updated: 2/3/2026)
Click here to contact Semhar Tewelde, MD
Nonatherosclerotic Coronary Artery Disease
- Nonatherosclerotic coronary artery disease (NACAD) is a term used to describe a category of diseases, which include: spontaneous coronary artery dissection (SCAD), coronary fibromuscular dysplasia (FMD), ectasia, vasculitis, embolism, vasospasm, or congenital anomaly.
- NACAD is an important cause of myocardial infarction (MI) in young women, but is often missed on coronary angiography.
- A small retrospective study of women <50 years of age with ACS found that 54.8% had normal arteries, 30.5% atherosclerotic heart disease (ACAD), 13% nonatherosclerotic coronary artery disease (NACAD), and 1.7% unclear etiology.
- NACAD accounted for 30% of MI’s with SCAD & Takotsubo cardiomyopathy accounting for the majority of cases.
Saw J, Aymong E, et al. Nonatherosclerotic Coronary Artery Disease in Young Women. Canadian Journal of Cardiology. 2014/07 Vol 30:Issue 7, pgs 814-819.
Category: Orthopedics
Keywords: Back Pain, Prednisone (PubMed Search)
Posted: 8/17/2014 by Michael Bond, MD
(Updated: 2/3/2026)
Click here to contact Michael Bond, MD
Is there any benefit to the use of prednisone in the treatment of lower back pain? One study showed that about 5% of patients receive prednisone for the treatment of their low back pain, but does it work.
A recent study by Eskin et al published in the Journal of Emergency Medicine looked at this question. They conducted a randomized controlled trial of 18-55 year olds with moderately severe low back. Patients were randomized to receive prednisone 50mg for 5 days or placebo.
The study enrolled a total of 79 patients, and 12 were lost to follow up. At followup there was no difference in their pain, or in them resuming normal activities, returning to work, or days lost from work. To make matters worse more patients in the prednisone group sought additional medical treatment 40% versus 18%.
Conclusion: With the results of this study we should continue the treatment of low back pain with non-steroidials, muscle relaxants and exercise. There does not appear to be any role for steroids in the treatment of these patients.
Eskin B, Shih RD, Fiesseler FW, et al. Prednisone for emergency department low back pain: a randomized controlled trial. Journal of Emergency Medicine. 2014;47(1):65–70. doi:10.1016/j.jemermed.2014.02.010.
Category: Pediatrics
Keywords: URI, sinusitis (PubMed Search)
Posted: 8/15/2014 by Jenny Guyther, MD
Click here to contact Jenny Guyther, MD
6-7% of kids presenting with upper respiratory symptoms will meet the definition for ABS.
The American Academy of Pediatrics (AAP) reviewed the literature and developed clinical practice guideline regarding the diagnosis and management of ABS in children and adolescents.
The AAP defines ABS as: persistent nasal discharge or daytime cough > 10 days OR a worsening course after initial improvement OR severe symptom onset with fever > 39C and purulent nasal discharge for 3 consecutive days.
No imaging is necessary with a normal neurological exam.
Treatment includes amoxicillin with or without clauvulinic acid (based on local resistance patterns) or observation for 3 days.
Optimal duration of antibiotics has not been well studied in children but durations of 10-28 days have been reported.
If symptoms are worsening or there is no improvement, change the antibiotic.
There is not enough evidence to make a recommendation on decongestants, antihistamines or nasal irrigation.
Wald et al. Clinical Practice Guideline for the Diagnosis and Management of Acute Bacterial Sinusitis in Children Aged 1 to 18 Years. Pediatrics. Volume 132, Number 1, July 2013.
Category: Toxicology
Keywords: acute kidney injury, AKI, synthetic cannabinoid (PubMed Search)
Posted: 8/13/2014 by Bryan Hayes, PharmD
(Updated: 8/14/2014)
Click here to contact Bryan Hayes, PharmD
Since synthetic cannabinoids arrived on the scene, we have become familiar with their sympathomimetic effects such as emesis, tachycardia, hypertension, agitation, hallucinations, and seizures.
Acute kidney injury is also being linked to synthetic cannabinoid use. Several clusters have been described in a handful of states, the most recent coming from Oregon with 9 patients.
AKI seems to be one more adverse effect to be on the lookout for when evaluating patients after synthetic cannabinoid use.
Centers for Disease Control and Prevention (CDC). Acute kidney injury associated with synthetic cannabinoid use – multiple states, 2012. MMWR Morb Mortal Wkly Rep 2013;62:93-8.
Bhanushali GK, et al. AKI associated with synthetic cannabinoids: a case series. Clin J Am Soc Nephrol 2013;8:523-6. [PMID 23243266]
Thornton SL, et al. Synthetic cannabinoid use associated with acute kidney injury. Clin Toxicol 2013;51:189-90. [PMID 23473465]
Buser GL, et al. Acute kidney injury associated with smoking synthetic cannabinoid. Clin Toxicol 2014;52:664-73. [PMID 25089722]
Follow me on Twitter (@PharmERToxGuy) or Google Plus (+bryanhayes13)
Category: Critical Care
Keywords: cardiomyopathy, sepsis, septic shock, pressors, inotropes, epinephrine, norepinephrine, dobutamine (PubMed Search)
Posted: 8/12/2014 by John Greenwood, MD
Click here to contact John Greenwood, MD
Should I Give My Patient with Septic Cardiomyopathy Fluids?
The incidence of acute LV dysfunction in septic shock is estimated to occur in 18 - 46% of patients within the first 24 hours of shock. Unlike the "classic" pattern of cardiogenic shock where LV filling pressure is high, in septic shock there are normal or low LV filling pressures.
Three therapeutic options should be strongly considered in the patient with a septic cardiomyopathy [CM]:
Recommended Reading
Vieillard-Baron, A. Septic cardiomyopathy. Ann Intensive Care. 2011; 1:6.
Follow me on Twitter @JohnGreenwoodMD
For more critical care pearls & education check out http://www.marylandccproject.org
Category: Visual Diagnosis
Posted: 8/11/2014 by Haney Mallemat, MD
(Updated: 8/12/2014)
Click here to contact Haney Mallemat, MD
30 year-old female with complains of night sweats and painful lesions on her fingertips. What’s the diagnosis and list some things to have in the differential diagnosis?

Answer: Osler Nodes
Osler notes are painful, palpable, and erythematous lesions secondary to the deposition of immune-complexes within the pads of digits.
Although classically associated with infective endocarditis, some authors claim that it may be seen in only 10-23% of confirmed cases. Therefore the differential diagnosis should also include:
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Cardiology
Posted: 8/10/2014 by Semhar Tewelde, MD
Click here to contact Semhar Tewelde, MD
- Toxic effects of tricyclic antidepressants (TCA) are result of the following 4 pharmacologic properties:
1. Inhibition of norepinephrine & serotonin reuptake --> resultant seizure
2. Anticholinergic activity --> resultant altered mental status, tachycardia, mydriasis, ileus
3. Direct alpha-adrenergic blockade --> resultant hypotension
4. Cardiac myocyte sodium channel blockade --> resultant widened QRS
- A QRS interval greater than 100 milliseconds has ~30% chance of developing seizures and ~15% chance of developing a life-threatening cardiac arrhythmia.
- A QRS interval greater than 160 milliseconds increases the chance of ventricular arrhythmias to greater than 50%.
- Clinical pearl: A very wide complex ventricular rhythm, concomitant hypotension and/or seizure disorder is suspicious for toxic ingestion and standard ACLS algorithm will not suffice, treatment must address the underlying culprit (i.e. TCA --> Tx. fluids, vasopressors, sodium bicarbonate, and intravenous lipid emulsion).
Kerr GW, McGuffie AC, Wilkie S. Tricyclic antidepressant overdose: a review. Emerg Med J. Jul 2001;18(4):236-41.
