Category: Orthopedics
Keywords: mono, spleen (PubMed Search)
Posted: 8/9/2014 by Brian Corwell, MD
Click here to contact Brian Corwell, MD
Return to Play After Infectious Mononucleosis (IM)
-Long incubation period make it difficult to determine source or onset
Presentation often atypical with nothing more than fatigue, decreased energy or decreased athletic performance.
DDX: Herpes simplex, HIV, CMV, toxo and strep (simultaneous infection may be seen in up to 30%)
Classic 3 to 5 day prodromal period (malaise, fatigue, anorexia)
Symptoms then progress into the classic “triad” of IM
Fever, pharyngitis, lymphadenopathy (esp. posterior cervical nodes)
May also have posterior palantine petechiae ( of cases), jaundice, exudative pharyngitis, rash and splenomegaly)
Rash (10% to 40%), transient, generalized maculopapular, petechial or urticarial)
Most commonly seen in patients treated with PCN antibiotics
Splenomegaly is an important complication in the athletic population
Mononucleosis makes the spleen susceptible to rupture (traumatic or spontaneous)
- Lymphocytic proliferation enlarges the spleen beyond protection from the ribs
- Physical examination has been shown to be unreliable for determining splenomegaly
- Highest risk is in the first 21 days (rare after 28 days)
Ultrasound is the modality of choice
-Splenomegaly peaks at 2 to 3 weeks and resolves in the majority between 4 to 6 weeks
Return to play is generally allowed after 4 weeks from diagnosis in the absence of splenomegaly and resolution of symptoms.
Category: International EM
Keywords: hypothermia, cold, environmental (PubMed Search)
Posted: 8/9/2014 by Jon Mark Hirshon, MPH, MD, PhD
(Updated: 2/3/2026)
Click here to contact Jon Mark Hirshon, MPH, MD, PhD
General Information:
Hypothermia is when the body’s core temperature is less than 35º C. Often thought as a winter disease, it can occur in nearly any climate or weather condition. However, a number of cold related conditions can occur without a drop in core body temperature.
Specific Cold Related Conditions:
Bottom line:
Remember that cold related injuries can occur without core hypothermia. Don’t forget the tetanus and antibiotics, as indicated.
Pathophysiology, management and complications of hypothermia. Lantry J, Dezman Z, Hirshon JM. Br J Hosp Med (Lond). 2012 Jan; 73(1):31-7.
Category: Pediatrics
Posted: 8/9/2014 by Rose Chasm, MD
Click here to contact Rose Chasm, MD
Category: Critical Care
Posted: 8/5/2014 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
There are many ventilator modes to choose from, but almost every mode can be distilled down to its basic principles by understanding the “Three T's of Mechanical Ventilation”
Trigger: You must determine whether the vent or patient will trigger a mechanical breath. For example, machine-triggered breaths (a.k.a. control mode of ventilation) are used for paralyzed patients and will deliver a breath after a period of time has elapsed (e.g., if RR is 10/min, then a breath is given every 6 seconds). On the other hand, if a patient’s respiratory drive is intact (a.k.a. assist-mode) than the patient triggers the breath when the vent detects a patient induced change in airflow or airway pressure. These two modes can also be mixed together.
Target: Mechanical breaths must have a specific target, either a target airway pressure or a tidal volume. Because pressure and volume are directly related, pick the variable you want to target and the other parameter will vary depending on the patient’s intrinsic physiology. For example, if you choose to target a specific tidal volume, we may get one plateau pressure in a patient with normal lungs, but a higher plateau pressure in another patient with stiffer lungs.
Terminate: You must decide when the mechanical breath (i.e., inspiration) terminates and expiration begins. Termination occurs: 1) after a set inspiratory time has elapsed in certain pressure-targeted modes, 2) when a predefined target volume has been achieved (i.e., volume-cycled modes), or 3) when airflow has been reduced by a certain percentage (as in pressure-support ventilation; to be discussed separately)
Let’s put this all together by looking at an example: pressure control ventilation (rate = 12/min and target pressure 20cm H20). Trigger: Because this is a “control”, not assist mode, the machine will trigger a breath 12 times per minute or every 5 seconds. Target: Here we chose to have pressure be the target, so when the ventilator triggers a breath it will deliver a constant airway pressure of 20 cmH2O until we tell the vent terminate that breath. Terminate: the constant airway pressure will be turned off after a fixed period of time has elapsed; for this example we will set the inspiratory time as 1 second, then expiration begins. Now, after a few vent breaths we will observe the results of our settings and reassess; if the resulting tidal volume is lower than what we wanted, we will increase the target pressure to increase the tidal volume. If the tidal volume is higher than what we wanted, we will reduce the target pressure to reduce the tidal volume. We can also tweak the inspiratory time to manipulate the tidal volume, but this does so to a lesser degree.
Try to break down your favorite modes of ventilation using the Three T’s and see if this helps you understand vent modes better.
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Visual Diagnosis
Posted: 8/4/2014 by Haney Mallemat, MD
(Updated: 8/12/2014)
Click here to contact Haney Mallemat, MD
40 year-old female presents with painful lesions and ulcers on lower extremities. She has had this before, but never to this extent. She also has a history of DVT. What’s the diagnosis?
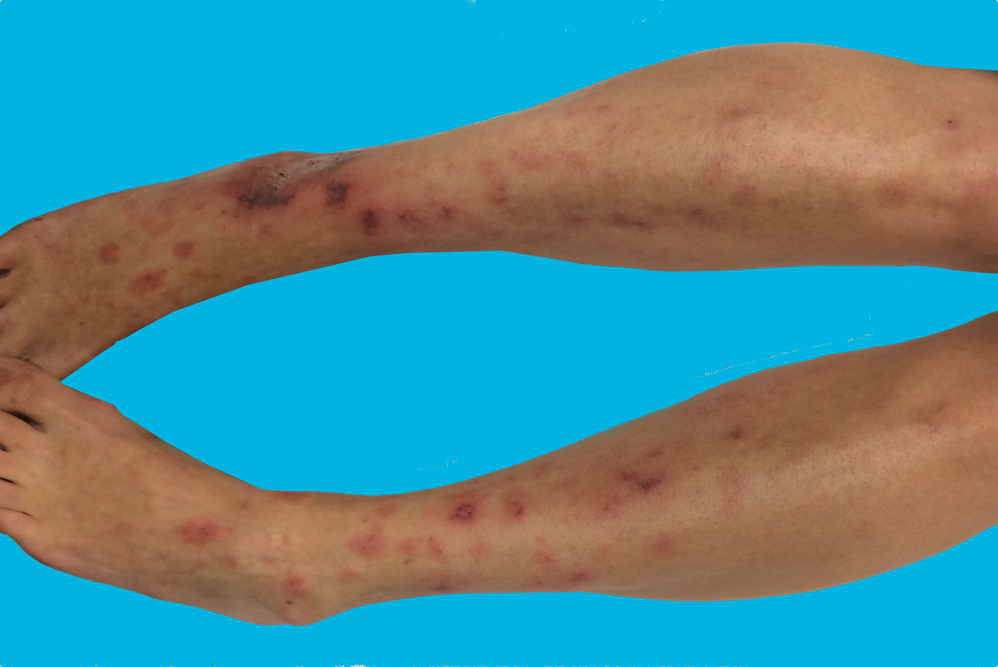
Answer: Livedoid vasculopathy or Livedoid vasculitis (LV)
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Cardiology
Keywords: Hypertrophic Cardiomyopathy (PubMed Search)
Posted: 8/3/2014 by Semhar Tewelde, MD
Click here to contact Semhar Tewelde, MD
Advances in Hypertrophic Cardiomyopathy (HCM)
- HCM is a genetically transmitted autosomal dominant disorder with two variants: hypertrophic obstructive cardiomyopathy (HOCM), also known as idiopathic hypertrophic subaortic stenosis (IHSS) or asymmetric septal hypertrophy, and non-obstructive hypertrophic cardiomyopathy (HNCM), also known as Yamaguchi syndrome.
- The most serious complication of both variants of HCM is sudden cardiac death (SCD) and end-stage heart failure, which rapidly progresses to cardiac death after its occurrence.
- Beta-blockers (1st line) and non-dihydropyridine calcium channel blockers are effective at improving clinical symptoms (syncope, dyspnea, chest pain, and exertional intolerance, etc.) however neither alone nor combined halt the progressive LV remodeling and prevent end-stage heart failure.
- Cardiac transplantation is the only treatment available for end-stage heart failure, but must occur before the onset of pulmonary hypertension, kidney malfunction, and thromboembolism for success.
- Class Ia anti-arrhythmic, disopyramide has been shown to be effective for symptomatic improvement (NYHA classification), but does not improve overall LV function or hypertrophy.
- A recent study found that another class Ia anti-arrhythmic, cibenzoline has been shown not only to reduce symptoms, but also improved LV diastolic dysfunction and induced a regression of LV hypertrophy. In this study cibenzoline has halted the progression of HCM to end-stage heart failure.
Hamada M, Ikeda S, et al. Advances in medical treatment of hypertrophic cardiomyopathy. Journal of Cardiology. July 2014 (64):1;1-10.
Category: Pharmacology & Therapeutics
Keywords: oseltamivir, critically ill, high-dose, influenza, Tamiflu (PubMed Search)
Posted: 7/28/2014 by Bryan Hayes, PharmD
(Updated: 8/2/2014)
Click here to contact Bryan Hayes, PharmD
Despite the lack of strong evidence to support the recommendation, the severity of the 2009 influenza pandemic prompted the World Health Organization (WHO) to advise that higher doses of oseltamivir (150 mg twice daily) and longer treatment regimens (> 5 days) should be considered when treating severe or progressive illness.
So, does the data support higher dosing in critically ill influenza patients?
A new systematic review concluded that "the small body of literature available in humans does not support routine use of high-dose oseltamivir in critically ill patients."
Flannery AH, et al. Oseltamivir dosing in critically ill patients with severe influenza. Ann Pharmacother 2014;48(8):1011-8. [PMID 24816209]
Follow me on Twitter (@PharmERToxGuy) or Google Plus (+bryanhayes13)
Category: Toxicology
Keywords: Bath salts, mephedrone, agitated delirium (PubMed Search)
Posted: 7/31/2014 by Kishan Kapadia, DO
Click here to contact Kishan Kapadia, DO
Bath salts (synthetic cathinones) commonly contain multipe synthetic drugs and can be ingested, smoked, or administered intravenously. The designer stimulant mephedrone (4-methylcathinone) is among the most popular of the derivatives of the naturally occurring psychostimulant cathinone. Bath salt use is on the rise and is responsible for a large number of ED visits.
In spite of their ban, bath salts are still available over the counter in specialty shops and through the Internet with common product names such as: "Ivory Wave," "Cloud 9," "Purple Wars," "Vanilla Sky," "Bliss," etc. They are commonly marketed with the disclaimer, "not for human consumption."
Their presentation mimics other sympathetic drugs through pathways similar to amphetamines. The primary psychological effects have a duration of roughly 3-4 hours, with physiologic effects lasting from 6-8 hours.
| Physical Effects | Behavioral & Mental Status Effects |
| Tachycardia | Agitation |
| Hypertension | Paranoia |
| Dysrhythmias | Hallucinations |
| Hyperthermia | Psychosis |
| Seizures | Violent behavior |
| Sweating | Delusions |
Management is largely supportive and includes IV hydration, benzodiazepines, and close monitoring in the ICU setting.
Imam SF, Patel H, Mahmoud M, et.al. Bath salts intoxication: A case series. JEM 2013;45(3):361-365.
Category: International EM
Keywords: Ebola, hemorrhagic fever, international (PubMed Search)
Posted: 7/30/2014 by Jon Mark Hirshon, MPH, MD, PhD
(Updated: 2/3/2026)
Click here to contact Jon Mark Hirshon, MPH, MD, PhD
General Information:
Ebola is a deadly hemorrhagic fever of the virus family Filoviridae.
Clinical Information:
Treatment and Public Health
Bottom Line:
While the likelihood of general dissemination to the general U.S. population is very low, U.S. healthcare workers need to be aware and alert for the signs and symptoms of Ebola for patients recently returned from West Africa.
References: http://www.cdc.gov/ebola
Current CDC advisory: http://emergency.cdc.gov/han/han00363.asp
Category: Critical Care
Keywords: epinephrine, im, anaphylaxis, allergic reaction, observation (PubMed Search)
Posted: 7/29/2014 by Feras Khan, MD
Click here to contact Feras Khan, MD
Observation after giving IM Epi for allergic reactions or anaphylaxis
Background
Question
Meta-analysis
Results
Limitations
What to do?
Grunau B, et al. Incidence of Clinically Important Biphasic Reactions in Emergency Department Patients with Allergic Reactions or Anaphylaxis. Annals of Emergency Medicine. Vol 63, No 6; June 2014 736-743.
Category: Visual Diagnosis
Posted: 7/27/2014 by Haney Mallemat, MD
(Updated: 7/28/2014)
Click here to contact Haney Mallemat, MD
2-day old baby boy presents with forceful vomiting of entire feeds, bloated belly, and has not passed stools since birth. What's the diagnosis?
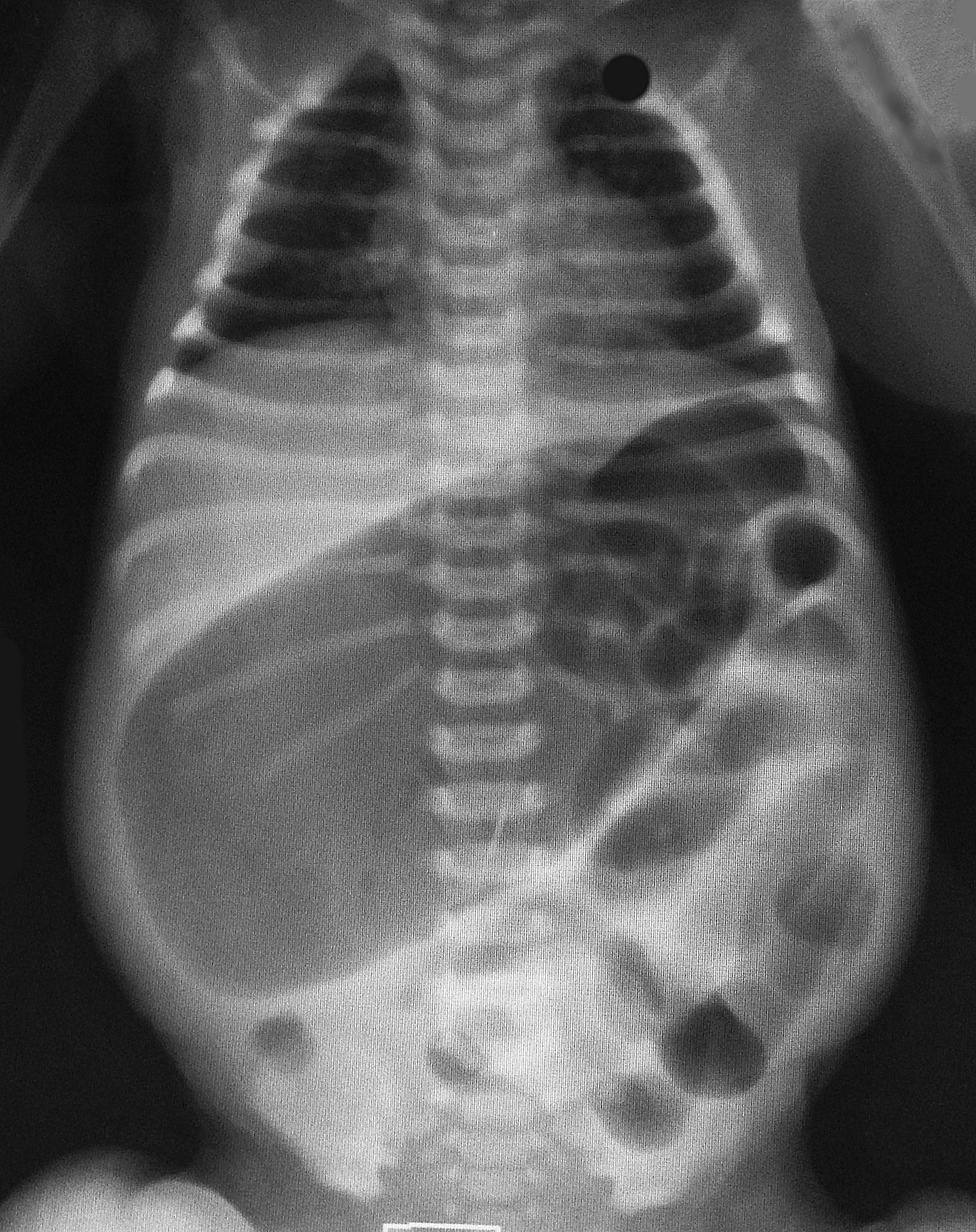
Colonic atresia
Colonic Atresia
Small bowel atresia
Meconium plug syndrome
Hirschsprung's disease
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
http://emedicine.medscape.com/article/934014-overview
Category: Cardiology
Posted: 7/27/2014 by Semhar Tewelde, MD
(Updated: 2/3/2026)
Click here to contact Semhar Tewelde, MD
HIV & Atherosclerosis
Advances in antiretroviral treatment has increased the life expectancy of patients with HIV significantly, AIDS-related deaths have fallen by 30% since they peaked in 2005.
HIV infection predisposes to a chronic inflammatory and immunologic dysfunctional state, subsequent highly active antiretroviral treatment (HAART) results in metabolic changes and dyslipidemia.
In the post-HAART era, CAD is now considered to be the main cause of heart failure in HIV-infected patients, superseding the prior most common etiologies myocarditis and opportunistic infections.
The presentation of CAD in HIV-infected patients is largely similar to that in the general population with the exception is that they present at a younger age.
Certain antiretroviral agents specifically protease inhibitors have conventionally been associated with lipid dysfunction, further complicating the HIV-infected patients milieu.
Recent research has shown that a C-C chemokine receptor-type 5 (CCR5) antagonists has emerged as a potential target both as an antiretroviral agent as well as in the process of arresting atherogenesis, but warrants more research.
Ng B, MacPherson P, et al. Heart failure in HIV infection: focus on the role of atherosclerosis. Current Opinion in Cardiology. Issue: Volume 29(2) pgs. 174-179 March 2014.
Category: Orthopedics
Keywords: Spinal Cord injury (PubMed Search)
Posted: 7/13/2014 by Brian Corwell, MD
(Updated: 7/23/2014)
Click here to contact Brian Corwell, MD
Cervical Cord Neuropraxia (CCN)
A concussion of the spinal cord as a result of an on-field collision.
A transient motor and/or sensory disturbance, lasting less than 24 hours.
A distinct and separate entity from spinal cord injury resulting in quadriplegia
Incidence 7.3 per 10,000 athletes
Approx. 50% of players experiencing CCN who return to play, have a second episode
The risk of this second episode is inversely proportional to the size of the cervical bony canal
Athletes with narrow canal diameter are more likely to have a 2nd episode
Those with normal canal diameter (14 mm on MRI) have a 5% risk
Those with a narrow canal (9 mm or less)) have a greater than 50% risk.
Whether repeat episodes lead to permanent spinal cord injury is unknown
Bell, Gordon. Return to play after Cervical Cord Neuroplraxia.2014
Category: Toxicology
Keywords: ondansetron (PubMed Search)
Posted: 7/24/2014 by Fermin Barrueto
(Updated: 2/3/2026)
Click here to contact Fermin Barrueto
Ondansetron is a highly effective anti-emetic that, since it has gone generic, is also quite inexpensive. There have been some reports of QT prolongation and cardiac arrhythmias especially with the high-dose 32mg IV dose for chemotherapy patients.
Is still safe in our ED population? A large systematic review was done in this month's Ann Emerg Med July 2014,p19-31.
Take Home Points:
1) No reports of arrhythmia associated with single dose administration identified
2) 80% of 60 unique reports were IV
3) 83% had significant PMH or already on a QT prolonging drug
Conclusion: Ondansetron doesn't warrant routine EKG or electrolyt screening in oral administration.High dose IV and High Risk patients do require more vigilance with EKG and electrolyte screening.
Category: Neurology
Keywords: intracranial hemorrhage, ICU, clinical decision rule (PubMed Search)
Posted: 7/23/2014 by Danya Khoujah, MBBS
Click here to contact Danya Khoujah, MBBS
Maybe not! A new prospective study looked at 600 adult trauma patients presenting with mild traumatic intracranial hemorrhage (with a GCS 13-15), and derived a clinical instrument that predicted the need for a “critical care intervention” (and therefore needing an ICU level of care). These interventions included intubation, neurosurgical intervention and need for invasive monitoring, among other things.
The derived instrument consisted of 4 variables:
1. GCS less than 15
2. Non-isolated head injury
3. Age 65 years or older
4. Evidence of swelling or shift on the initial head CT
The presence of at least one of these variables predicted the need for critical intervention, identifying 114 of the 116 patients who actually did require it, making it 98.3% sensitive.
This clinical decision rule is yet to be externally validated.
Nishijima D K, et al. Derivation of a Clinical Decision Instrument to Identify Adult Patients with Mild Traumatic Intracranial Hemorrhage at Low Risk for Requiring ICU Admission. Ann Emerg Med 63(2014); 448-456
Category: Critical Care
Posted: 7/22/2014 by Mike Winters, MBA, MD
Click here to contact Mike Winters, MBA, MD
Predicting Neurologic Outcome in Patients Treated with TTM
Golan E, et al. Predicting neurologic outcome after targeted temperature management for cardiac arrest: Systematic review and meta-analysis. Crit Care Med 2014; 42:1919-30.
Category: Visual Diagnosis
Posted: 7/21/2014 by Haney Mallemat, MD
(Updated: 7/22/2014)
Click here to contact Haney Mallemat, MD
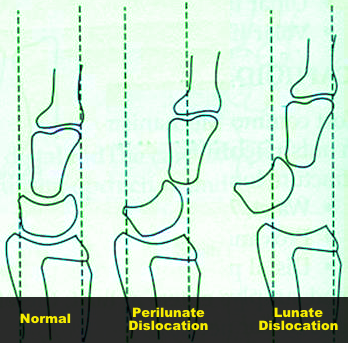
45 year-old right-hand dominant patient presents with right hand pain from a prior injury to hand. Patient has also been injecting subcutaneous heroin into hand for relief. What's the diagnosis?

Perilunate dislocation (volar displacement)...and severe hand cellulitis.
Perilunate and Lunate dislocations
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Cardiology
Keywords: ARVD (PubMed Search)
Posted: 7/20/2014 by Semhar Tewelde, MD
Click here to contact Semhar Tewelde, MD
ECG Risk Predication in ARVD
Arrhythmogenic right ventricular dysplasia (ARVD) is a genetically determined cardiomyopathy characterized by fibrofatty replacement of the right ventricle (RV) predisposing to ventricular arrhythmias, heart failure, and sudden cardiac death (SCD).
Twelve-lead electrocardiography (ECG) is an easily obtainable and noninvasive risk stratification tool for major adverse cardiac event (MACE); defined as a composite of cardiac death, heart transplantation, survived sudden cardiac death, ventricular fibrillation, sustained ventricular tachycardia, or arrhythmic syncope.
ARVD ECG findings that predict adverse outcome are not well known.
A multicenter, observational, long-term study, found ECG findings were quite useful for risk stratification of MACE, specifically:
- Repolarization criteria
- Inferior leads T wave inversions
- Precordial QRS amplitude ratio of ≤0.48
- QRS fragmentation
Saguner A, Ganahi S, et al. Usefulness of Electrocardiographic Parameters for Risk Prediction in Arrhythmogenic right ventricular dysplasia. American Journal of Cardiology. May 15, 2014. Vol 113, Issue 10,1728-34.
Category: International EM
Keywords: Smallpox, public health, infectious diseases (PubMed Search)
Posted: 7/19/2014 by Jon Mark Hirshon, MPH, MD, PhD
Click here to contact Jon Mark Hirshon, MPH, MD, PhD
· Smallpox (Variola):
o Only eradicated human infectious disease.
o Prior to the advent of vaccination, it killed an estimated 400,000 Europeans annually and was a major cause of blindness.
· Major potential as a bioterrorism agent:
o Now only supposed to exist in two laboratories in the world (at the CDC in Atlanta, Georgia and in the Vector Institute in Koltsovo, Russia).
· Recently, previously unknown vials of active virus from the 1950s were found in a NIH laboratory in Maryland.
· Clinical Presentation:
o Incubation is usually 10-12 days (range 7-17 days)
o Signs and symptoms include:
§ Febrile (38.8-40.0C) prodome lasting 1-4 days, headache, myalgia (esp. back/spinal pain), pharyngitis, chills, abdominal pain
§ Rash: classically round and well circumscribed. May be confluent or umbilicated. The rash evolves slowly: macules to papules to pustules to scabs.
· It is important to differentiate smallpox from chicken pox (Varicella):
o Smallpox: Significant prodrome. Centrifugal rash (trunk to extremities). Can involve soles and palms. Lesions are in the same stage of development on any one part of the body.
o Chickenpox: Minimal prodrome. Centripetal rash (extremities to trunk). Seldom on soles and palms. Asynchronus evolution of rash.
Bottom Line:
Smallpox is a global public health emergency and requires immediate reporting. If the clinical presentation is unclear, discuss with local infectious disease experts or public health officials.
Category: Pediatrics
Keywords: tympanostomy tubes, antibiotics, otorrhea (PubMed Search)
Posted: 7/18/2014 by Jenny Guyther, MD
Click here to contact Jenny Guyther, MD
Up to 26% of patients with tympanostomy tubes (PE tubes) can suffer from clinically manifested otorrhea. This is thought to be the result of acute otitis media that is draining through the tube. Previous small studies suggested that antibiotic ear drops are as effective or more effective and with less side effects for its treatment. This study compared treatment with antibiotic/glucocorticoid ear drops (hydrocortisone-bacitracin-
Study population: Children 1-10 years with otorrhea for up to 7 days in the Netherlands
Exclusion criteria included: T > 38.5 C, antibiotics in previous 2 weeks, PE tubes placed within 2 weeks, previous otorrhea in past 4 weeks, 3 or more episodes of otorrhea in past 6 months
Patient recruitment: ENT and PMD approached pt with PE tubes and they were told to call if otorrhea developed and a home visit would be arranged
Study type: open-label, pragmatic, randomized control trial
Primary outcome: Treatment failure defined as the presence of otorrhea observed otoscopically
Secondary outcome: based on parental diaries of symptoms, resolution and recurrence over 6 months
Results: After 2 weeks, only 5% of the ear drop group compared to 44% of the oral antibiotic group and 55% of the observation group still had otorrhea. There was not a significant difference between those treated with oral antibiotics and those that were observed. Otorrhea
lasted 4 days in the ear drop group compared to 5 days with oral antibiotics and 12 days with observation (all statistically significant).
Key differences: The antibiotic dosing and choice of ear drops are based on availability and local organism susceptibility.
Bottom line: For otorrhea in the presence of PE tubes, ear drops (with a non-aminoglycoside antibiotic and a steroid) may be more beneficial than oral antibiotics or observation.
van Dongen TM, van der Heijden GJ, Venekamp RP, Rovers MM, Schilder AG. A trial of treatment for acute otorrhea in children with tympanostomy tubes. N Engl J Med 2014; 370:723-33.
