Category: Critical Care
Posted: 10/14/2014 by Mike Winters, MBA, MD
(Updated: 2/3/2026)
Click here to contact Mike Winters, MBA, MD
Hemoglobin Threshold in Septic Shock
Holst LB, et al. Lower versus higher hemoglobin threshold for transfusion in septic shock. NEJM 2014; [published online]
Category: Visual Diagnosis
Posted: 10/13/2014 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
A neck ultrasound is performed during endotracheal intubation. What is labeled "A", what is labeled "B" and what's the diagnosis?
Answer:
A: Trachea
B: Esophagus
This is an esophageal intubation! Take out the tube and try again. Check out this podcast for more on the technique from my good friends at the ultrasound podcast
Here's a summary:
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Cardiology
Posted: 10/12/2014 by Semhar Tewelde, MD
(Updated: 2/3/2026)
Click here to contact Semhar Tewelde, MD
Kounis Syndrome (Part II)
- KS can develop from multiple etiologies: hymenoptera, proteins, vasoactive amines, histamine, acetylcholine, multiple antibiotics, and various medical conditions (angioedema, serum sickness, asthma, stress-induced cardiomyopathy).
- Hypersensitivity myocarditis and KS are two cardiac entities of allergic etiology affecting the myocardium and coronary arteries, respectively. These two entities can mimic each other and can be clinical indistinguishable.
- Presence of eosinophil’s, atypical lymphocytes, and giant cells on myocardial biopsy suggests hypersensitivity myocarditis.
- There is evidence showing use of corticosteroids with vasospastic angina with evidence of allergy or the presence of symptoms refractory to high-dose vasodilators has been reported to resolve symptoms.
Kounis GN, Soufras GD, Kouni SA, et al. Hypersensitivity myocarditis and hypersensitivity coronary syndrome (Kounis syndrome). Am J Emerg Med 2009;27:506–508.
Vivas D, Rubira JC, Ortiz AF, et al. Coronary spasm and hypersensitivity to amoxicillin: Kounis or not Kounis syndrome? Int J Cardiol 2008;128:279–281.
Category: Airway Management
Keywords: Concussion, patient education (PubMed Search)
Posted: 10/11/2014 by Brian Corwell, MD
Click here to contact Brian Corwell, MD
There is no effective pharmacologic treatment known to hasten recovery from concussion. In future pearls we will examine possible interventions that may help.
The importance of educating our patients was demonstrated in two studies looking at concussion education. Patients were separated into 2 groups. The intervention group received a booklet of information discussing common symptoms of concussion, suggested coping strategies and the likely time course of recovery. At a 3 month follow-up evaluation, the intervention group reported fewer symptoms. This was repeated in pediatric patients with similar results.
Take Home: Consider taking the time to put such an information sheet together for concussed patients seen in the ED.
Ronsford J, et al. Impact of early intervention on outcome after mild traumatic head in adults. 2002
Category: Pediatrics
Posted: 10/10/2014 by Rose Chasm, MD
(Updated: 2/3/2026)
Click here to contact Rose Chasm, MD
Bennett NJ, et al. Pediatric Pneumonia Treatment and Management. Medscape. April 2014.
AAP. Management of Communty-Acquired Pneumonia in Infants and Children Older than 3 Months of Age. Pediatrics. Vol 128 No 6 December 1, 2011.
Category: Toxicology
Keywords: calcium channel blocker, poisoning (PubMed Search)
Posted: 10/6/2014 by Bryan Hayes, PharmD
(Updated: 10/11/2014)
Click here to contact Bryan Hayes, PharmD
In a precursor to a forthcoming international guideline on the management of calcium channel blocker poisoning, a new systematic review has been published assessing the available evidence.
A few findings from the systematic review:
Stay tuned for the international guideline coming out soon. One treatment recommendation from the new guideline, reported at the 8th European Congress on Emergency Medicine last month, is not to use glucagon.
St-Onge M, et al. Treatment for calcium channel blocker poisoning: a systematic review. Clin Toxicol 2014. [Epub ahead of print]. [free full-text PDF]
Follow me on Twitter (@PharmERToxGuy) or Google Plus (+bryanhayes13)
Category: Neurology
Keywords: Hydrocephalus, CSF shunt malfunction, ventriculomegaly, Evans' ratio (PubMed Search)
Posted: 10/8/2014 by WanTsu Wendy Chang, MD
Click here to contact WanTsu Wendy Chang, MD
Hydrocephalus is a disorder of cerebrospinal fluid (CSF) accumulation. Acute obstructive hydrocephalus such as in subarachnoid hemorrhage and CSF shunt malfunction can cause a rapid rise in intracranial pressure. Nonobstructive hydrocephalus is associated with subacute symptoms. Clinical features of acute obstructive hydrocephalus include headache, blurred vision, papilledema, ocular palsies, nausea and vomiting, and decreased level of consciousness.
Evaluation of hydrocephalus in the ED should include neuroimaging, typically noncontrast head CT given its wide availability. CT characteristics of hydrocephalus can be seen in Figure 1: ventriculomegaly with dilated 3rd ventricle, dilated 4th ventricle, and presence of temporal horns.
When evaluating patients with pre-existing hydrocephalus for worsening symptoms, such as in the evaluation of CSF shunt malfunctions, it is helpful to compare the head CT or MRI for interval ventricular enlargement. Two simple measurements can be taken on a CT or MRI for objective comparisons (Figure 2).
Evans' ratio = A/B = Maximum width of frontal horns (A) divided by maximum width of inner skull (B) at the same CT/MRI level
C = Width of 3rd ventricle
Use of acetazolamide to decrease CSF production is not effective in long-term treatment of hydrocephalus. About 75% of patients with hydrocephalus require CSF shunt placement.
Shprecher D, Schwalb J, Kurlan R. Normal pressure hydrocephalus: diagnosis and treatment. Curr Neurol Neurosci Rep. 2008;8(5):371-376.
Poca MA, Sahuquillo J. Short-term medical management of hydrocephalus. Expert Opin Pharmacother. 2005;6(9):1525-1538.
Anvekar B 2011, Neuroradiology Cases, viewed 8 October 2014,
Category: Misc
Keywords: app pearls apple google (PubMed Search)
Posted: 10/7/2014 by Kevin Hamilton
Click here to contact Kevin Hamilton
We are proud to announce the release of our new UMEM Pearls App, now available in the Apple App Store and the Google Play Marketplace! You will now be able to pull down pearl content for offline viewing, in addition to having all of the pearls in searchable format available on your mobile devices.
Click either of the following links on your mobile device to download your Pearls App today!
Category: Critical Care
Posted: 10/6/2014 by John Greenwood, MD
(Updated: 10/7/2014)
Click here to contact John Greenwood, MD
The ARISE Trial
Early, aggressive resuscitation and attention to detail are essential element of managing critically ill patients. This past week the ARISE trial was published - a 2nd large, randomized control study to examine the benefit of protocolized vs. usual care in patients with severe sepsis and septic shock.
What were the main findings? After enrolling 1,600 patients who presented to the ED in severe sepsis or septic shock:

Bottom Line: Resuscitation goals for the patient with septic shock should include:
Additional therapeutic goals should be made on a patient by patient basis. Reassess your patient frequently, pay attention to the details, and you will improve your patient’s mortality.
Suggested Reading
Follow Me on Twitter: @JohnGreenwoodMD
Category: Visual Diagnosis
Posted: 10/6/2014 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
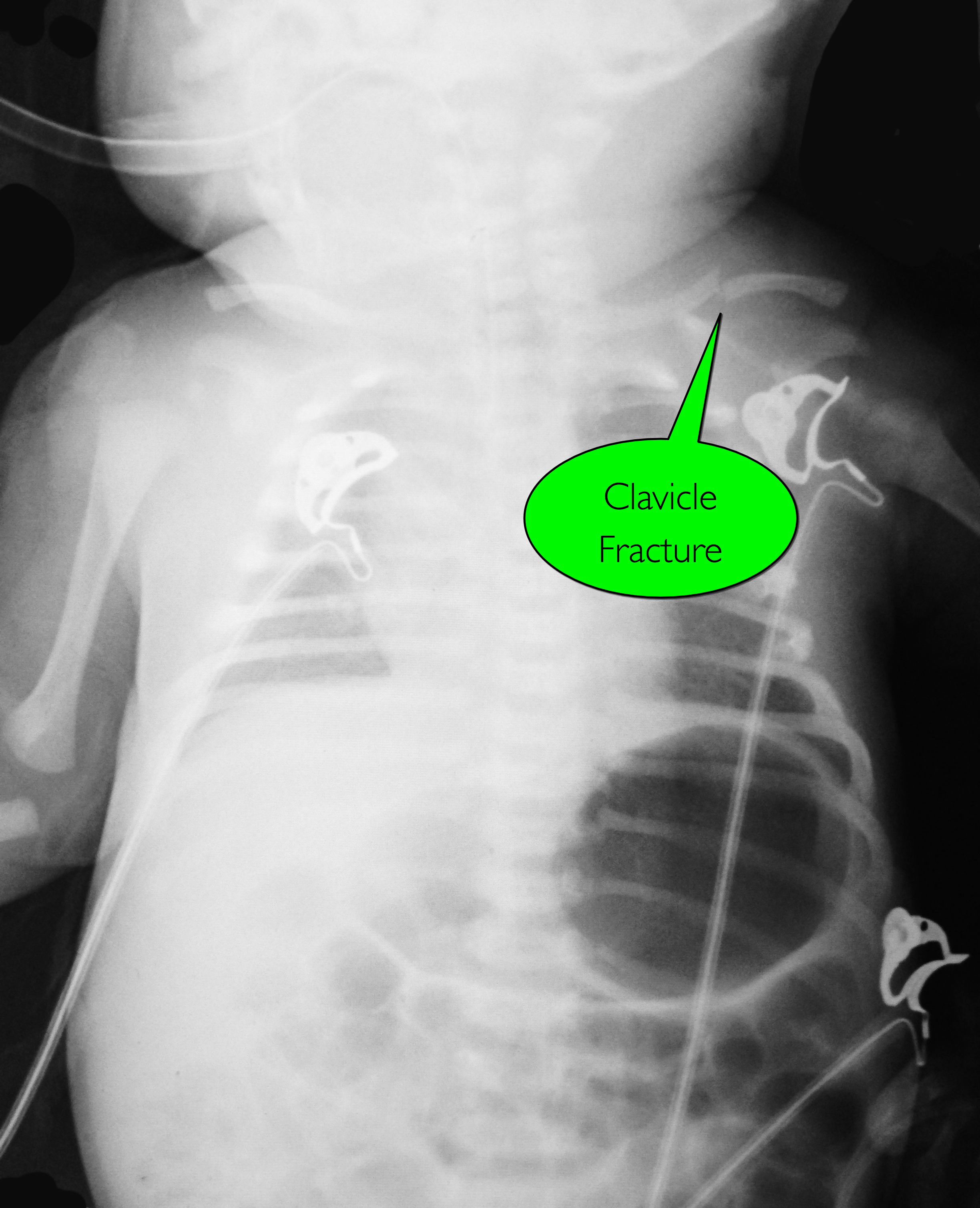
7d old child presents with difficulty feeding,vomiting one time, and now with intermittent apneic episodes. What's the diagnosis? (Careful....this one is tricky!)
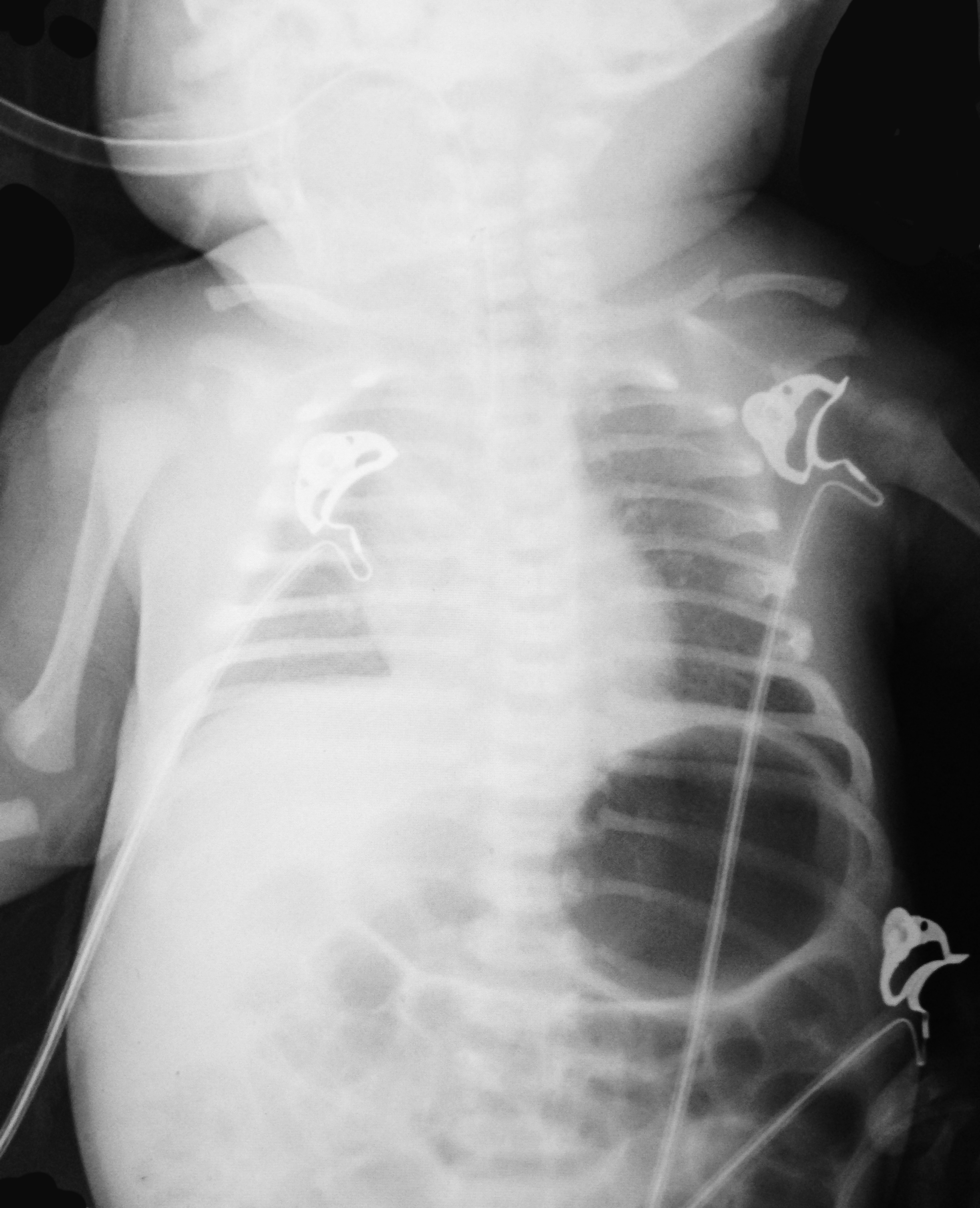
Answer: Workup should include an ALTE and sepsis evaluation PLUS evaluation for non-accidental trauma
Non-accidental trauma (NAT)
NAT is most prevalent in children 0-3 months of age.
Classic metaphyseal lesions, rib fractures, and fractures in various stages of healing are most commonly described in children.
How do we know this is not just birth trauma from a shoulder dystocia, large for gestational age, or difficult vaginal delivery?
Subperiosteal new bone formation appears as a:
NAT Work-up:
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Cardiology
Posted: 10/4/2014 by Semhar Tewelde, MD
Click here to contact Semhar Tewelde, MD
Kounis Syndrome (Part I)
- Kounis & Zavras (1991) described the syndrome of allergic angina and allergic myocardial infarction, currently known as Kounis syndrome (KS). Braunwald (1998) noted vasospastic angina can be induced by allergic reactions, with mediators such as histamine and leukotrienes acting on coronary vascular smooth muscle.
- Two subtypes have been described: type I, occurring in patients without predisposing factors for CAD often caused by coronary artery spasm and type II, occurring with angiographic evidence of coronary disease when the allergic events induce plaque erosion or rupture.
- This syndrome has been reported in association with a variety of medical conditions, environmental exposures, and medication exposures. Entities such as Takotsubo cardiomyopathy, drug-eluted stent thrombosis, and coronary allograft vasculopathy also appear to be associated with this syndrome.
- Clinical presentation includes: symptoms and signs of an allergic reaction and acute coronary syndrome: chest pain, dyspnea, faintness, nausea, vomiting, syncope, pruritus, urticaria, diaphoresis, pallor, palpitations, hypotension, and bradycardia.
Kounis GN, Kounis SA, Hahalis G, et al. Coronary artery spasm associated with eosinophilia: another manifestation of Kounis syndrome? Heart Lung Circ 2009;18:163–164.
Mytas DZ, Stougiannos PN, Zairis MN, et al. Acute anterior myocardial infarction after multiple bee stings. A case of Kounis syndrome. Int J Cardiol 2009;134:e129–e131.
Category: Pharmacology & Therapeutics
Keywords: beta-lactam, piperacillin/tazobactam, critically ill (PubMed Search)
Posted: 9/27/2014 by Bryan Hayes, PharmD
(Updated: 10/4/2014)
Click here to contact Bryan Hayes, PharmD
Beta-lactam antimicrobials (penicillins, cephalosporins, and carbapenems) are frequently used for empiric and targeted therapy in critically ill patients. They display time-dependent killing, meaning the time the antibiotic concentration is above the minimin inhibitory concentration (MIC) is associated with improved efficacy.
Two new pharmacodynamic/pharmacokinetic studies suggest that current beta-lactam antimicrobial dosing regimens may be inadequate.
Antimicrobial dosing in critically ill patients is complex. Current dosing of beta-lactams may be inadequate and needs to be studied further with relation to clinical outcomes.
Follow me on Twitter (@PharmERToxGuy) or Google Plus (+bryanhayes13)
Category: International EM
Keywords: Influenza (PubMed Search)
Posted: 10/1/2014 by Jon Mark Hirshon, MPH, MD, PhD
(Updated: 10/29/2014)
Click here to contact Jon Mark Hirshon, MPH, MD, PhD
INFLUENZA
What is it?
Why do we care about influenza?
Bottom line
Category: Toxicology
Keywords: Digoxin, Cardioactive Steroids, Digitoxin, Digoxin-specific Fab Fragment (PubMed Search)
Posted: 10/1/2014 by Kishan Kapadia, DO
Click here to contact Kishan Kapadia, DO
Cardioactive steroids are among the many treatments used for CHF, and for the control of ventricular response rate in atrial tachydysrhythmias. There are many sources of cardioactive steroids:
Pharmaceutial: Digoxin, Digitoxin
Plants: Oleander, Yellow Oleander, Foxglove, Lily of the Valley, Dogbane, Red Squill
Animal: Bufo marinus toad
It is a potent Na+-K+-ATPase inhibitor and can lead to hyperkalemia in acute ingestion with associated signs and symptoms of N/V, abdominal pain, bradycardia and possibly, hypotension.
Toxicity should be suspected with bidirectional ventricular tachycardia or atrial tachycardia with high-degree AV block
Therapeutic range of digoxin of 0.5 - 2.0 ng/mL is helpful but not a sole indicator of toxicity
Indication for antidote (Digoxin-specific Antibody Fragments) include:
1) Digoxin-related life-threatening dysrhythma
2) Serum K+ > 5.0 mEq/L in acute ingestion
3) Serum digoxin concentration >15ng/mL at any time, or >10 ng/mL 6 hours postingestion
4) Ingestion of 10 mg in adult; 4 mg in pediatric
5) Poisoning by non-digoxin cardioactive steroid
Goldfrank's Toxicologic Emergencies, 9th edition
Category: Critical Care
Posted: 9/30/2014 by Haney Mallemat, MD
(Updated: 10/1/2014)
Click here to contact Haney Mallemat, MD
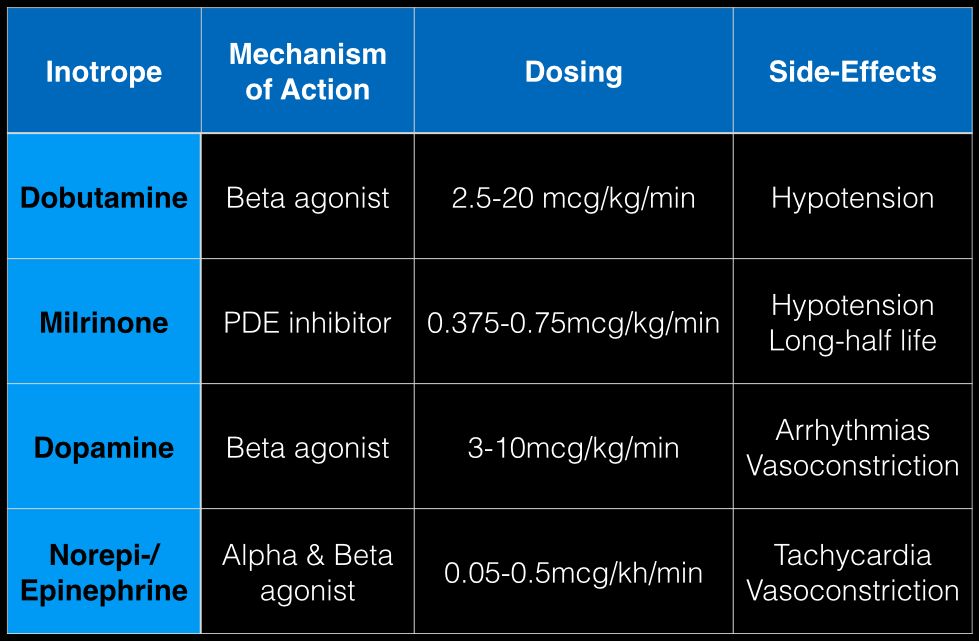
The last Back to the Basics post discussed the use of vasopressors to improve hemodynamics by increasing arterial (and venous) tone. This time we’ll discuss the use of agents to increase inotropy for patients with severe systolic dysfunction / failure.
Dobutamine: a direct b1 and b2-receptors agonist. It has no peripheral vasoconstrictor properties, so if blood pressure increases it occurs secondary to increased cardiac output. Unfortunately, blood pressure may be decreased in some patients due to its peripheral vasodilatory effects; in these cases it may need to be used with a vasopressor.
Milrinone: augments contractility by increasing intracellular Ca levels via cellular phosphodiesterase inhibition. Because it does not work on beta-receptors, it might be preferred for patients taking beta-blockers requiring inotropic support. It may cause peripheral vasodilation and hypotension, but this may be a benefit if pulmonary artery pressure is elevated as reductions in pulmonary artery pressure lead to improvements in right ventricular function. It has a long-half life and should be avoided in patients with renal impairment.
Dopamine: chemical precursor to norepinephrine and technically a vasopressor. At moderate doses (3-10 mcg/kg/min) it works on beta-receptors to increase myocyte contractility. At higher doses works primarily as a vasopressor, which may reduce cardiac output due to higher afterload.
Norepinephrine/epinephrine: has alpha and beta properties that lead to increased peripheral vasoconstriction, but also increases inotropy and chronotropy (faster heart rate)
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)a
Category: Visual Diagnosis
Posted: 9/28/2014 by Haney Mallemat, MD
(Updated: 10/1/2014)
Click here to contact Haney Mallemat, MD
Person presents with painless vision loss after seeing flashes of light. Ultrasound is below. What's the diagnosis?
Answer: Vitreous hemorrhage with retinal detachment
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Cardiology
Posted: 9/28/2014 by Semhar Tewelde, MD
(Updated: 2/3/2026)
Click here to contact Semhar Tewelde, MD
Ventricular Arrhythmias Originating from the Moderator Band
- Ventricular arrhythmias originating from the moderator band (MB) often have a distinct morphology
- Typically MB arrhythmias have a left bundle branch block pattern, QRS with a late precordial transition (>V4), a rapid down stroke of the QRS in the precordial leads, and a left superior frontal plane axis
- MB arrhythmias are often associated with PVC-induced ventricular fibrillation
- Catheter ablation is quite effective at termination of the arrhythmias and facilitated with intracardiac echocardiography (ICE)
Sadek M, Benhayon D, et al. Idiopathic ventricular arrhythmias originating from the moderator band: Electrocardiographic characteristics and treatment by catheter ablation. Heart Rhythm. Aug 2014
Category: Orthopedics
Keywords: Sciatica, radiculopathy, imaging (PubMed Search)
Posted: 9/19/2014 by Brian Corwell, MD
(Updated: 9/27/2014)
Click here to contact Brian Corwell, MD
Back pain with radiculopathy can be very distressing to a patient and they have heard from their medically savvy neighbor that a MRI is the way to go. Now, armed with this knowledge, they are in your ED with earplugs in hand...
A few minutes of reassurance and education can save in both cost and ED throughput.
In one study researchers performed MRIs on asymtomatic adult patients.
Almost two-thirds (64%) had abnormal discs
Just over half (52%) had bulging discs
Almost a third (31%) had disc protrusions
Further, finding a bulging disc already suggested by your history and physical examination does not change management. The majority of these patients improve with conservative treatment within four to to six weeks.
Restrict ED MRI use for the evaluation of suspected cauda equina, epidural abscess and spinal cord compression.
Category: Pediatrics
Keywords: E. coli, O0157:H7, hematochezia, diarrhea (PubMed Search)
Posted: 9/26/2014 by Mimi Lu, MD
Click here to contact Mimi Lu, MD
There are numerous different causes of pediatric hemorrhagic diarrhea. Consider a pediatric patient with bloody diarrhea as being at risk for developing hemolytic uremic syndrome. Most cases of hemolytic uremic syndrome are caused by O157:H7 strains of E Coli that release Shiga-like toxin from the gut. Systemic release of the toxin causes microvascular thromboses in the renal microvasculature. The characteristic microangiopathic hemolysis results with anemia, thrombocytopenia and peripheral schistocytes seen on laboratory studies, in addition to acute renal failure.
Antibiotics have been controversial in the treatment of pediatric hemorrhagic diarrhea due to concern that they worsen toxin release from children infected with E Coli O157:H7 and thus increase the risk of developing hemolytic uremic syndrome. Numerous previous studies have provided conflicting data regarding the true risk (1). A recent prospective study showed antibiotic treatment increases the risk (2). Most recommendations warn against using antibiotics to treat pediatric hemorrhagic diarrhea unless the patient is septic.
Bottom line: Avoid treating pediatric hemorrhagic diarrhea with antibiotics
References:
1. Systematic review: are antibiotics detrimental or beneficial for the treatment of patients with Escherichia coli O157:H7 infection? Alimentary Pharmacology & Therapeutics. Volume 24, Issue 5, pages 731–742, September 2006
2. Risk factors for the hemolytic uremic syndrome in children infected with Escherichia coli O157:H7: a multivariable analysis. Clin Infect Dis. 2012 Jul;55(1):33-41. doi: 10.1093/cid/cis299. Epub 2012 Mar 19.
Category: Toxicology
Keywords: disulfiram (PubMed Search)
Posted: 9/25/2014 by Fermin Barrueto
(Updated: 2/3/2026)
Click here to contact Fermin Barrueto
When you prescribe certain medications, it may require some further instructions to avoid ethanol or a disulfiram like reaction (nausea, vomiting, flushing) may occur. Keep this short list in your brain:
1) Particular cephalosporins: cefotetan is a the one more likely
2) Nitrofurantoin
3) Sulfonylureas: chlorpropamide and tolbutamide
4) Metronidazole
5) Trimethoprim-sulfamethoxazole
Goldfranks 8th Edition, p1179
