Category: Orthopedics
Keywords: heel, pain, causes (PubMed Search)
Posted: 1/17/2015 by Michael Bond, MD
(Updated: 2/2/2026)
Click here to contact Michael Bond, MD
We often think of Plantar Fascitis as the cause of heel pain but there are a lot of other causes. Some of those include:
Category: Toxicology
Keywords: intraosseous, hydroxocobalamin, cyanide poisoning (PubMed Search)
Posted: 1/15/2015 by Hong Kim, MD
(Updated: 2/2/2026)
Click here to contact Hong Kim, MD
Hydroxocobalamin is an effective cyanide antidote when administered intravenously. Although intraosseous (IO) access is often used in critically ill patients with difficult or delayed IV access, the efficacy of IO administration has not been investigated until recently.
In a recent randomized animal study, acute cyanide toxicity was induced in two groups of swine where 150 mg/kg Hydroxocobalamin was administered via IV vs. IO. The survival rate, reversal of hypotension, and laboratory results were similar between the IV and IO group.
The finding of this study suggest that IO administration of Hydroxocobalamin is as efficacious as IV administration and its administration in acute cyanide toxicity should not be delayed due to lack of IV access when IO access is available.
Bebarta VS, Pitotti RL, Bondreau S and Tanen DA. Intraosseus versus intravenous infusion of hydroxocobalamin for the treatment of acute severe cyanide toxicity in a swine model. Academic Emergency Medicine. 2014; 21 (11): 1203-1211.
Category: Neurology
Keywords: traumatic brain injury, progesterone, neuroprotectant, clinical trials, PROTECT III, SYNAPSE (PubMed Search)
Posted: 1/14/2015 by WanTsu Wendy Chang, MD
Click here to contact WanTsu Wendy Chang, MD
Is progesterone yet another disappointing neuroprotectant?
Traumatic brain injury (TBI) affects more than 1.7 million persons in the U.S. annually. The incidence of TBI is increasing globally, especially in developing countries. Despite improvement in trauma systems and critical care, the morbidity and mortality associated with severe TBI remain high.
Progesterone has been shown in preclinical and phase 2 randomized clinical trials to have pluripotent neuroprotective properties and improve mortality in TBI.
Two multicenter phase 3 trials were recently completed and published in the December 25th issue of the New England Journal of Medicine. However, their results were disappointing.
Both studies used the Glasgow Outcome Scale (GOS) or Extended Glasgow Outcome Scale (GOS-E) at 6 months as their primary outcome. The GOS and GOS-E capture the degree of recovery from brain injury in terms of disability, stratified into levels by death, vegetative state, severe disability, moderate disability, and good recovery.
Progesterone was not found to have any benefit in functional outcome at 6 months.
Both of these studies were well designed and conducted. However, they were based on small effect sizes of the phase 2 trials. In addition, they had very favorable outcome rates in the placebo group, thereby making it hard to demonstrate a benefit by their sample sizes.
There has been a long history of failed neuroprotectant trials likely due to the complex and variable injury mechanisms involved in TBI. The currently available outcome measures are also insensitive to the targeted mechanistic endpoints. More research is needed to understand not only potential therapies but also how to select appropriate patients for these therapies.
Take Home Point: Progesterone does not have any clear benefit in TBI at this time.
Wright DW, Yeatts SD, Silbergleit R, et al. Very early administration of progesterone for acute traumatic brain injury. N Engl J Med. 2014;371(26):2457-2466.
Skolnick BE, Maas AI, Narayan RK, et al. A clinical trial of progesterone for severe traumatic brain injury. N Engl J Med. 2014;371(26):2467-2476.
Category: Critical Care
Keywords: diaphragm weakness, respiratory failure (PubMed Search)
Posted: 1/13/2015 by Feras Khan, MD
Click here to contact Feras Khan, MD
Diaphragm weakness and its significance
There are several ways to monitor diaphragm strength and function
Clinical Relevance
Curr Opin Crit Care. 2015 Feb;21(1):34-41. doi: 10.1097/MCC.0000000000000168.
Monitoring and preventing diaphragm injury.
Category: Visual Diagnosis
Posted: 1/12/2015 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
60 year-old male presents with rhinorrhea, body aches, and dry cough for two days. He recently moved here from Kentucky. What’s the diagnosis (please note that there are several differentials based on CXR)?
Answer Histoplasmosis
Histoplasma capsulatum is the fungus that causes histoplamosis, and is endemic to soil in the “Histo belt” of the U.S. (including all of Arkansas, Kentucky, Missouri, Tennessee, and West Virginia and parts Alabama, Illinois, Indiana, Iowa, Kansas, Louisiana, Maryland, Mississippi, Nebraska, Ohio, Oklahoma, Texas, and Virginia); it is found internationally as well.
Outbreaks have occurred following digging up the ground at construction at sites where this yeast lives in the soil, but spores can also become airborne and inoculate people.
Most cases are asymptomatic, but it is associated with a variety of pulmonary syndromes and can have extrapulmonary findings such as splenic calcifications. Disseminated disease typically occurs in immunocompromised patients
Treatment includes itraconazole for mild to moderate disease and amphotericin for disease that is severe or widespread disease.
Differentials:
- Blastomycosis
- Septic emboli
- Sarcoidosis
- Tuberculosis (milliary)
- Aspergillosis
- Carcinoid lung tumor
- Atypical or viral pneumonias
Category: Cardiology
Posted: 1/12/2015 by Semhar Tewelde, MD
(Updated: 2/2/2026)
Click here to contact Semhar Tewelde, MD
APACHE-HF Scoring System
The Acute Physiology and Chronic Health Evaluation (APACHE) scoring system was established in the 1980's to predict critically ill patient prognosis (APACHE II, III, and IV have been published in last two decades).
The APACHE II scoring system involves combining 3 separate scores (acute physiology score, chronic health score, and age), which can be cumbersome to apply & thus is not often utilized in the emergency department (modified APACHE II doesn't include chronic health score & is less taxing).
No unique scoring system for acute heart failure (AHF) has been analyzed until present; the APACHE-HF score includes 8 criteria: mean arterial pressure (MAP), pulse, sodium, potassium, hematocrit, creatinine, age, and glasgow coma score (GCS).
AHF in-hospital mortality data was analyzed and compared using APACHE II, modified APACHE II, and APACHE- HF scores and the predictive value of the APACHE-HF score was found to be optimal when compared to the others.
Hirotake O, Akihiro S, et al. New scoring system (APACHE-HF) for predicting adverse outcomes in patients with acute heart failure: Evaluation of the APACHE II and Modified APACHE II scoring systems. Journal of Cardiology. Volume 64, Issue 6, Pages 421-510 (December 2014)
Category: Orthopedics
Keywords: Contusion, hematoma (PubMed Search)
Posted: 1/10/2015 by Brian Corwell, MD
Click here to contact Brian Corwell, MD
Mechanism: Direct blow to anterior thigh (Football/basketball) or from a ball traveling at a high rate of speed (field hockey/lacrosse).
Exam: focal tenderness and edema. Pain may be severe and worse with active contraction and passive stretch. Hematoma may already be present. Amount of passive knee flexion at 24 hours can be a clue to the severity of the hematoma.
Treatment: Crutches if pain with weight-bearing. Ice. Immobilization in 120 degrees of flexion immediately after the injury for the first 24 hours may be beneficial.
-Bandage entire lower limb. Provide crutches and pain medication. Soft tissue therapy is contraindicated for the first 48 hours and when instituted must be gentle and cause no pain. Risk of re-bleeding is greatest in first 7 to 10 days.
http://fce-study.netdna-ssl.com/2/images/upload-flashcards/75/20/63/5752063_m.jpg
Category: Pediatrics
Posted: 1/10/2015 by Rose Chasm, MD
(Updated: 2/2/2026)
Click here to contact Rose Chasm, MD
Andolfatto G, et al. Intranasal ketamine for analgesia in theemergency department: a prospective observational study. Acad Emerg Med. 2013. Oct;20(10):1050-4.
Tsze DS, et al. Intranasal ketamine for procedural sedation in pediatric laceration repair: a preliminary report. Pediatr Emerg Care. 2012. August;28(8);767-70.
Hall D, et al. Intranasal ketamine for procedural sedation. Emerg Med J. 2014;31:789-90.
Category: Toxicology
Keywords: whole bowel irrigation, WBI, GI decontamination (PubMed Search)
Posted: 1/6/2015 by Bryan Hayes, PharmD
(Updated: 1/15/2015)
Click here to contact Bryan Hayes, PharmD
Application to Clinical Practice
WBI can facilitate removal of select toxicants from the gastrointestinal tract in some patients, but there is no convincing evidence from clinical studies that it improves the outcome of poisoned patients.
Thanacoody R, et al. Position paper update: Whole bowel irrigation for gastrointestinal decontamination of overdose patients. Clin Toxicol 2015;53(1):5-12. [PMID 25511637]
Follow me on Twitter (@PharmERToxGuy) or Google Plus (+bryanhayes13)
Category: International EM
Keywords: Tuberculosis, infectious disease (PubMed Search)
Posted: 1/7/2015 by Jon Mark Hirshon, MPH, MD, PhD
Click here to contact Jon Mark Hirshon, MPH, MD, PhD
Tuberculosis (TB) is a major infectious disease that occurs worldwide.
Fortunately, public health and clinical measures have had some success.
Bottom line:
http://www.who.int/mediacentre/factsheets/fs104/en/
http://www.cdc.gov/tb/topic/treatment/
Category: Critical Care
Posted: 1/6/2015 by Mike Winters, MBA, MD
Click here to contact Mike Winters, MBA, MD
"PQRST" - Capnography in Cardiac Arrest
Heradstveit BE, Heltne JK. PQRST - A unique aide-memoire for capnography interpretation during cardiac arrest. Resuscitation 2014; 85:1619-20.
Category: Visual Diagnosis
Posted: 1/5/2015 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
A male patient presents with right lower quadrant pain. The ultrasound is shown at the point of maximal tenderness. The diameter of the structure (image on right) is about 0.94cm. What is this structure and what's the diagnosis?
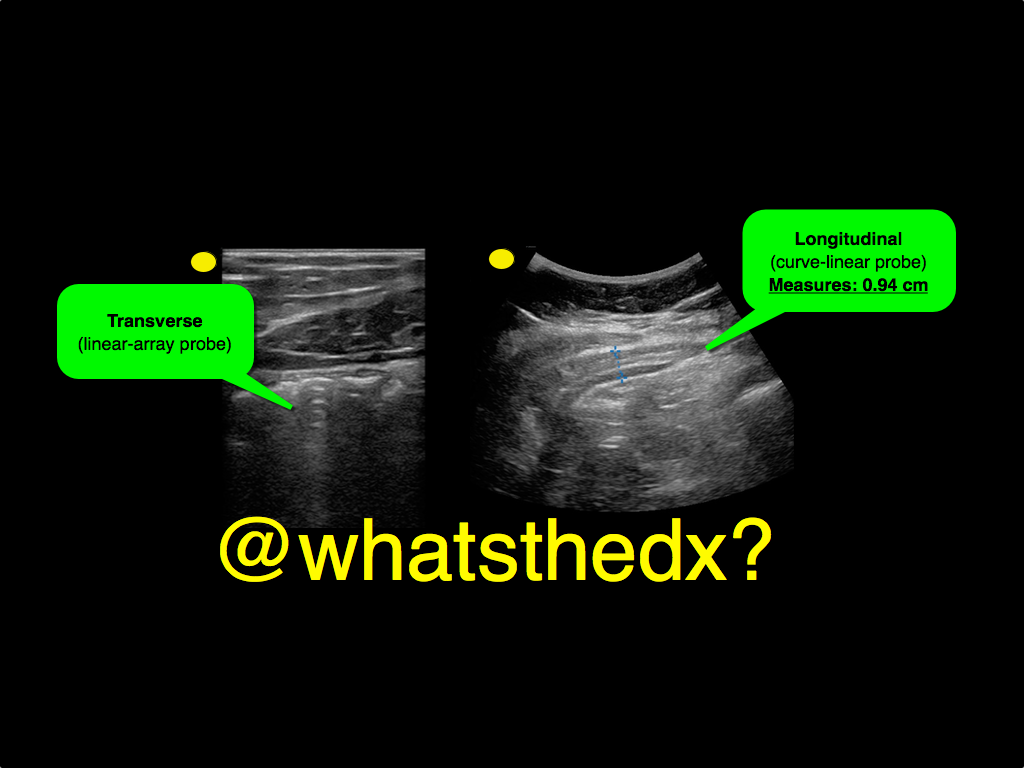
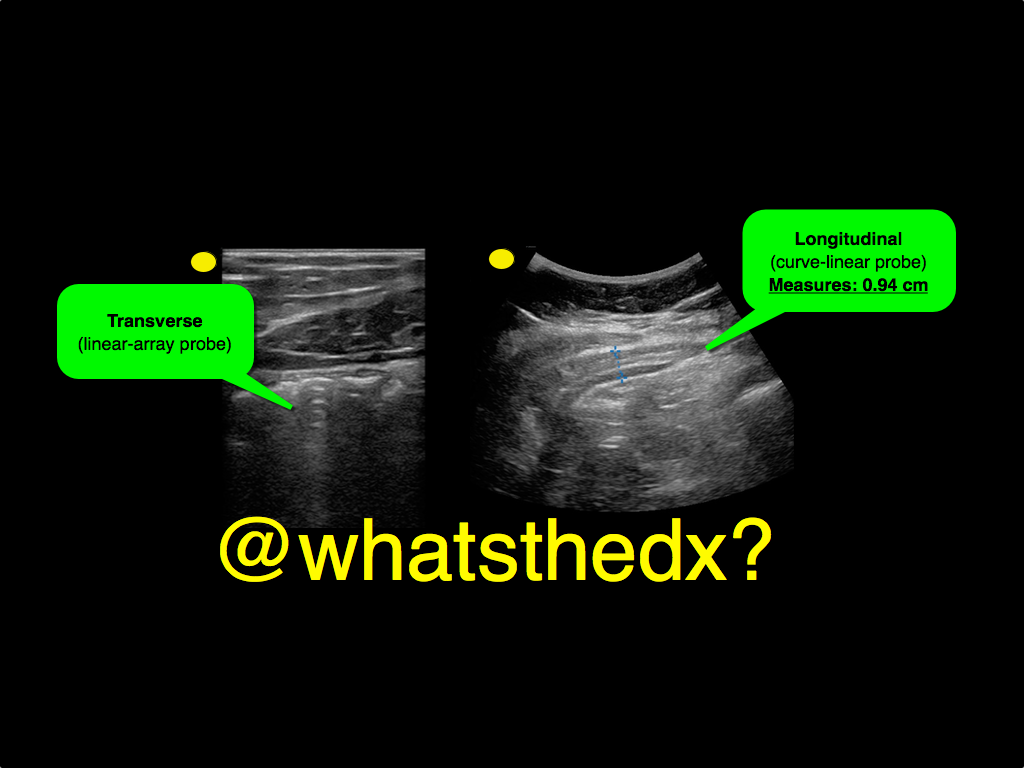
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Pediatrics
Keywords: intraosseous access, pediatrics (PubMed Search)
Posted: 1/3/2015 by Ashley Strobel, MD
(Updated: 2/2/2026)
Click here to contact Ashley Strobel, MD
Are you comfortable with Intraosseous Catheter Placement in Children during a code? A pediatric code or child in distress is also distressing to care providers. Your staff may not feel comfortable with IO access in children. Read on to be more comfortable with your options as IO access in children can be difficult, especially the chubby toddlers. The basics for a patient in distress are "IV, O2, Monitor". Access is vital to giving resuscitation medications.
Indications for IO access: Any child in whom IV access cannot readily be obtained, but is necessary.
All IOs are 15G for infusion equal to central vascular access.
Different colors indicate different sizes:
Preferred sites:
Kids-do NOT use the sternum or distal radius
The reference from NEJM has videos to review placement and different tools (manual, EZ IO, and autoinjector).
Category: Pharmacology & Therapeutics
Keywords: headache, migraine, metoclopramide, magnesium (PubMed Search)
Posted: 12/31/2014 by Bryan Hayes, PharmD
(Updated: 1/3/2015)
Click here to contact Bryan Hayes, PharmD
Does IV magnesium have a role in the management of acute migraine headache in the ED? A new study says yes. [1]
Intervention
What They Found
Magnesium sulfate was more effective in decreasing pain severity at 20-min (pain scale 5.2 vs. 7.4) and 1-h (2.3 vs. 6.0) and 2-h (1.3 vs. 2.5) intervals after treatment (p < 0.0001) compared to treatment with dexamethasone/metoclopramide.
Follow me on Twitter (@PharmERToxGuy) or Google Plus (+bryanhayes13)
Category: International EM
Keywords: Injuries, alcohol, fireworks (PubMed Search)
Posted: 12/31/2014 by Jon Mark Hirshon, MPH, MD, PhD
(Updated: 1/7/2015)
Click here to contact Jon Mark Hirshon, MPH, MD, PhD
As you get ready to celebrate the coming of a new year, it is important to be safe while you are having a good time.
Injuries seen during holidays, such as new years, include:
If you are working, be ready to see increased alcohol and injury related visits.
If you are off and plan to celebrate, be sure to identify a designated driver or an alternate means of getting home.
Have a Happy and Safe 2015!
Category: Critical Care
Posted: 12/30/2014 by John Greenwood, MD
Click here to contact John Greenwood, MD
Cartoons Kill: A new high-risk patient for critical illness & death
This past month, the BMJ published an impressive retrospective review that analyzed nearly 80 years of data to find that animated characters in children’s films are in fact at a very high-risk for death when compared to characters in adult dramas.
Films ranged from 1937 (Snow White) to 2013 (Frozen) and were compared against the two highest gossing dramatic films in that same year. The authors found that nearly two thirds of the children’s animated films contained an on-screen death of an important character compared to only half in adult dramas.
Fatalities were most commonly the result of:
Other high-risk animated characters include the parents of the protagonist (17.8% mortality) and nemeses (28.9% mortality). Median survival time was approximately 90 minutes (much less than the usual ED LOS!)
Notable early on-screen deaths included Nemo’s mother being eaten by a barracuda 4 minutes into Finding Nemo, Tarzan’s parents being killed by a leopard 4 minutes into Tarzan, and Cecil Gaines’ father being shot in front of him 6 minutes into The Butler.
The author’s intention was to point out the psychological impact of death on young children, but I think the authors also highlight an important, high-risk patient population that could present to your ED.
Bottom Line: Animated characters should be aggressively resuscitated and strongly considered for admission to a higher level of care should they present to your ED, as they appear to be at high-risk for death and rapid decompensation.
May all of you have a happy and safe 2015!
Reference
1. Colman I, Kingsbury M, Weeks M, et al. CARTOONS KILL: casualties in animated recreational theater in an objective observational new study of kids' introduction to loss of life. BMJ. 2014;349:g7184.
Follow me on Twitter: @JohnGreenwoodMD
Category: Visual Diagnosis
Posted: 12/29/2014 by Haney Mallemat, MD
(Updated: 12/30/2014)
Click here to contact Haney Mallemat, MD
19 year-old male complaining of left arm pain one week after injecting anabolic steroids into his sholder. What's the diagnosis?
Myositis of the deltoid muscle
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Cardiology
Posted: 12/28/2014 by Semhar Tewelde, MD
Click here to contact Semhar Tewelde, MD
Holiday Heart
- Holiday heart commonly refers to alcohol use and rhythm disturbances, particularly supraventricular tachydysrhythmias.
- The most common rhythm disorder is atrial fibrillation (AF), which usually converts to normal sinus rhythm within 24 hours and antiarrhythmic therapy is typically not indicated.
- Analyses of ECGs in patients who have consumed a large quantity of alcohol show prolongation of the PR, QRS, and QT intervals.
- 2014 AHA/ACC/HRS updated guidelines for nonvalvular AF utilize the CHA2DS2-VASc (congestive heart failure, hypertension, age ≥75 years [doubled], diabetes mellitus, prior stroke or TIA or thromboembolism [doubled], vascular disease, age 65 to 74 years, and sex category) score for assessment of stroke risk.
Tonelo D, Providência R, Gonçalves L. Holiday heart syndrome revisited after 34 years. Arq Bras Cardiol. Aug 2013;101(2):183-9.
2014 AHA/ACC/HRS Guideline for the Management of Patients with Atrial Fibrillation: Executive Summary. JACC Vol 64, Issue 21, Dec 2014.
Category: Orthopedics
Keywords: knee dislocation, vascular and nerve injury, vascular emergency (PubMed Search)
Posted: 12/26/2014 by Brian Corwell, MD
(Updated: 12/27/2014)
Click here to contact Brian Corwell, MD
Knee Dislocation
Following reduction and immobilization, a thorough vascular assessment should follow. Any signs of vascular injury should prompt immediate vascular consultation (pallor, absent or diminished pulses)
1) Palpate popliteal and distal pulses
2) Measure ankle-brachial index (*ABI) (<0.9 = abnormal)
3) Duplex ultrasound (if available)
*ABI ratio of SBP in lower (DP/PT) and upper (brachial) extremities.
**Evaluation is often institutional specific. Discuss with your consultants.
A) If strong pulses normal ABI and normal u/s admit patient for observation with serial vascular examinations.
B) If the limb is still well perfused but the pulses are asymmetric or ABI is abnormal or US is abnormal then consult vascular surgery and obtain arteriogram (expanding role for CTA here).
C) If pulses are weak or absent or distal signs of ischemic limb then obtain emergent vascular consultation for surgical repair.
Category: Pediatrics
Posted: 12/27/2014 by Mimi Lu, MD
Click here to contact Mimi Lu, MD
Cyanotic (right to left shunt) Congenital Heart Disease (CHD) lesions can be easily remembered with the 1,2,3,4,5 method.
1- Truncus Arteriosis (ONE trunk)
2- Transposition of the Great Vessels (TWO vessels flipped)
3- TRIcuspid Atresia
4-TETRAlogy of Fallot
5- Total Anomolous Pulmonary Venous Return (TAPVR=5 words/letters)
A few other important DUCTAL-DEPENDENT lesions: Coarctation of the Aorta, Hypoplastic Left Heart Syndrome, and Pulmonary Atresia.
Patients present to the emergency department within the first week of life in severe distress, including hypoxia, tachypnea, and hypotension. The above cyanotic CHD all reflect DUCTAL-DEPENDENT lesions, meaning they need a widely open PDA (which closes in the first week of life) to maintain sufficient oxygenation for viability.
These patients will not survive without timely intervention with prostaglandin (PGE1), so be sure to initiate this life-saving medication as soon as possible! Side effects include apnea…be prepared to intubate your neonate!
