Category: Pharmacology & Therapeutics
Keywords: sodium, piperacillin/tazobactam, ampicillin, moxifloxacin, metronidazole (PubMed Search)
Posted: 4/13/2015 by Bryan Hayes, PharmD
(Updated: 5/2/2015)
Click here to contact Bryan Hayes, PharmD
Aside from sodium chloride and sodium bicarbonate, several commonly used emergency department medications (namely IV antibiotics) contain a significant amount of sodium. In patients with heart failure or other conditions requiring sodium restriction, judicious use should be considered.
Notes:
Ampicillin/sulbactam [package insert]. Metronidazole [package insert]. Moxifloxacin [package insert]. Nafcillin [package insert]. Piperacillin/tazobactam [package insert]. Ticarcillin/clavulanate [package insert].
Follow me on Twitter (@PharmERToxGuy) or Google Plus (+bryanhayes13)
Category: Toxicology
Keywords: morphine, clopidogrel (PubMed Search)
Posted: 4/30/2015 by Fermin Barrueto
Click here to contact Fermin Barrueto
There are some studies that have shown that NSTEMI patients have done worse when administered opioids. Most studies were not well controled and the exact mechanism was not clear. This study adds a biological mechanism to these fidnings.
Hobl et al. showed clopidogre concentrations delayt peak yhours, have overall decrease AUC and actually decrease active metabolites when morphine is administered IV. Morphine may not be the right choice in any ACS that receives clopidogrel.
Hobl et al. Morphine Decreases Clopidogrel Concentrations and Effects: A Randomzed Double-Blid, Placebo-Controlled Trial. Journal of the American College of Cardiology 2014; 63(7): 630-635.
Category: International EM
Keywords: Surgey, anesthesia, trauma (PubMed Search)
Posted: 4/29/2015 by Jon Mark Hirshon, MPH, MD, PhD
Click here to contact Jon Mark Hirshon, MPH, MD, PhD
A Lancet Commission on Global Surgery has just published a 56 page article about the need to improve access to surgery and anesthesia care. Its five key messages are:
The need for high quality acute care, both for urgencies and emergencies, is clearly an important component of providing “universal access to safe, affordable surgical and anaesthesia care”- the vision of the Commission.
Global Surgery 2030: evidence and solutions for achieving health, welfare, and economic development: http://dx.doi.org/10.1016/S0140-6736(15)60160-X
Global surgery—going beyond the Lancet Commission: http://dx.doi.org/10.1016/S0140-6736(15)60465-2
Category: Critical Care
Posted: 4/28/2015 by Mike Winters, MBA, MD
Click here to contact Mike Winters, MBA, MD
SIRS and Severe Sepsis Screening
Kaukonen KM, Bailey M, Pilcher D, et al. Systemic Inflammatory Response Syndrome Criteria in Defining Severe Sepsis. NEJM 2015;372:1629-38.
Category: Visual Diagnosis
Posted: 4/27/2015 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
70 year-old female presents from a nursing home with fever and abdominal pain. A right upper quadrant ultrasound is shown, what's the diagnosis?
Acalculous cholecystitis
Acalculous Cholecystitis
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Orthopedics
Keywords: back pain, ESR, CRP, malignancy (PubMed Search)
Posted: 4/25/2015 by Brian Corwell, MD
Click here to contact Brian Corwell, MD
In cases of suspected spinal infection, the sensitivity of an elevated WBC count (35-61%), ESR (76-95%) and CRP (82-98%) may help guide further evaluation or consideration of other entities.
Incorporation of ESR/CRP into an ED decision guideline may help differentiate those patients in whom MRI may be performed on a nonemergent basis.
An elevated ESR (>20 mm/hour) also has a role in the diagnostic evaluation of occult malignancy (sensitivity 78%, specificity 67%).
Davis DP, Salazar A, Chan TC, Vilke GM. Prospective evaluation of a clinical decision guideline to diagnose spinal epidural abscess in patients who present to the emergency department with spine pain: Clinical article. Journal of Neurosurgery: Spine. 2011;14(6):765-770.
Deyo RA, Diehl AK. Cancer as a cause of back pain. Journal of general internal medicine. 1988;3(3):230-238.
Category: Neurology
Keywords: tumor, seizure, stroke (PubMed Search)
Posted: 4/23/2015 by Danya Khoujah, MBBS
Click here to contact Danya Khoujah, MBBS
Some medical issues arise in patients with brain tumors:
// Steroids are used to decrease vasogenic edema, especially preop or during radiation therapy. Patients are ideally gradually weaned off steroids. Dexamethasone is most commonly used. 1-2% of patients are at risk for adrenal suppression.
// Infections: Post-op wound infections can be delayed up to months, especially in patients on steroids.
// Antiepileptics: Although technically not recommended in patients with brain tumors who have not had seizures (American Academy of Neurology 2010), many surgeons continue to prescribe antiepileptics preoperatively and then discontinue them by 1 month postop if the patients remain seizure-free. Levetiracetam is emerging as the drug of choice due to favorable side effect profile.
// Thromboembolism: Brain tumors are considered very high risk for venous thromboembolism. Low-molecular-weight heparin is the treatment of choice, with warfarin being an acceptable substitute.
// Arterial thrombosis and ischemic stroke: Risk is increased with certain medications, and thrombolysis is contraindicated.
Pruitt AA. Medical Management of Patients with Brain Tumors. Continuum 2015;21(2):314 331
Category: Critical Care
Keywords: large hemispheric infarct, acute ischemic infarct, stroke (PubMed Search)
Posted: 4/20/2015 by John Greenwood, MD
(Updated: 4/21/2015)
Click here to contact John Greenwood, MD
Updates in the Management of Large Hemispheric Infarction
Large hemispheric infarctions (LHI) are estimated to occur in 2-8% of all hospitalized ischemic strokes and 10 15% of all MCA territory infarcts. LHI carry high rates of morbidity and mortality, in fact, if left untreated associated cerebral edema can rapidly progress to transtentorial herniation and death in 40 80% of patients.
Recognized risk factors for progressive cerebral edema include:
Evidence based medical strategies for LHI include:
Prophylactic hemicraniectomy
Bottom Line: Early recognition of large hemispheric stroke is critical as it is associated with a high rate of morbidity and mortality. Aggressive medical management and early neurosurgical involvement may improve outcomes.
References
Follow me on Twitter @JohnGreenwoodMD
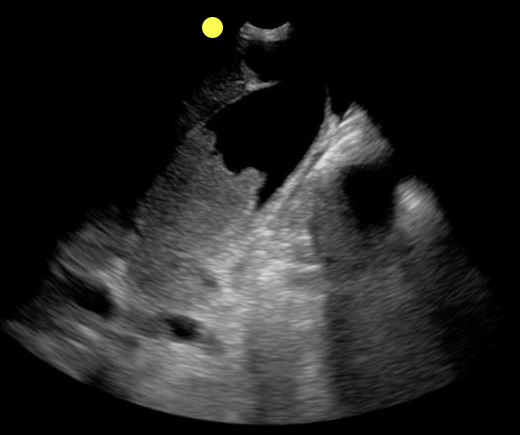
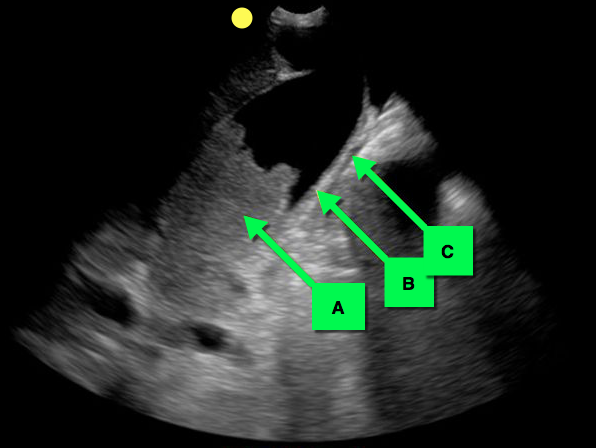
Category: Visual Diagnosis
Posted: 4/20/2015 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
You see the following on a parasternal long-axis view; what's the diagnosis and what coronary distribution is involved?
Severe hypokinesis with anterioseptal wall motion abnormality.
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Cardiology
Posted: 4/19/2015 by Semhar Tewelde, MD
(Updated: 2/2/2026)
Click here to contact Semhar Tewelde, MD
Cardiac Sarcoidosis
- Cardiac Sarcoidosis (CS) is reported to involve ~2-5% of patients with systemic sarcoidosis. An increasing proportion of patients are presenting with isolated CS.
- Isolated CS is associated with a higher female predominance; severe LV involvement, heart failure, and poor prognosis.
- Manifestations range from symptomatic conduction disturbances, dysrhythmias, progressive heart failure, and silent myocardial granulomas - leading to sudden cardiac death.
- CS is a serious condition with a quoted 5-year survival ~60-75%.
- Corticosteroid therapy is considered cornerstone in management, but evidence is largely observational and no randomized trials have been performed to date.
Kandolin R, Lehtonen J, et al. Cardiac Sarcoidosis. Circulation 131 (7) Feb. 2015.
Category: Orthopedics
Keywords: knee, hip, back, pain, acetaminophen (PubMed Search)
Posted: 4/18/2015 by Michael Bond, MD
(Updated: 2/2/2026)
Click here to contact Michael Bond, MD
Is acetaminophen good for pain control in patients with Osteoarthritic of the Knee or Hip or Low Back Pain? Most of my patients request narcotics, but conventional teaching is that we should try to start with Acetaminophen or NSAIDs.
This recent study, http://www.bmj.com/content/350/bmj.h1225, published in the BMJ analyzed 13 studies looking at over 5400 patients. In the end, they found that acetaminophen did not appear to improve pain, disability or the patient’s quality of life in patients with back pain. Also, there was a small improvement in pain and disability in those with hip and knee pain, but it was not deemed clinically significant.
Even worse, patients taking acetaminophen had a 4x greater chance of having abnormal liver function tests.
This meta-analysis really questions whether Acetaminophen should be first line therapy in patients with osteoarthritis of the knees or hips, or in those with low back pain. For now I will stick with a course of a NSAID. Especially with the risk of unintentional overdose if they are taking other over the counter medicaitons that might also contain acetaminophen.
Machado GC, Maher CG, Ferreira PH, Pinheiro MB, Lin CW, Day RO, McLachlan AJ, Ferreira ML. Efficacy and safety of paracetamol for spinal pain and osteoarthritis: systematic review and meta-analysis of randomised placebo controlled trials. BMJ. 2015 Mar 31;350:h1225. doi: 10.1136/bmj.h1225
Category: Pediatrics
Keywords: Traumatic lumbar punctures, fever, infants (PubMed Search)
Posted: 4/17/2015 by Jenny Guyther, MD
Click here to contact Jenny Guyther, MD
Approximately ¼ of lumbar punctures (LP) are traumatic or unsuccessful in infants. What is the implication of this?
A retrospective cross sectional study over a 10 year period at Boston Children’s Hospital looked at infants aged 28 to 60 days who had blood cultures sent from the Emergency Department and who had LPs performed. The ED clinicians at this facility routinely follow the “Boston Criteria” to identify infants at low risk for spontaneous bacterial infection (SBI). Traumatic LPs were defined as CSF red cell count greater than or equal to 10x10^9 cells/L while an unsuccessful LP was defined as one where no CSF was available for cell counts. A small portion of the unsuccessful LPs did not have CSF cultures sent.
173 infants had traumatic or unsuccessful LPs. The SBI rate did not differ between the normal LP and the traumatic and unsuccessful LP infants. Median hospital charges were higher in the traumatic or unsuccessful LPs compared to the normal LP group ($ 5117 US dollars versus $ 2083 US dollars).
Bottom Line: Traumatic or unsuccessful LPs lead to higher hospital charges.
Pingree EW, Kimia, AA and Nigrovic LE. The Effect of Traumatic Lumbar Puncture on Hospitalization Rate for Febrile Infants 28 to 60 Days of Age. Academic Emergency Medicine 2015; 22: 240-243.
Category: International EM
Keywords: Children, unintentional injuries, burns, drownings, falls, road crashes, poisoning (PubMed Search)
Posted: 4/16/2015 by Jon Mark Hirshon, MPH, MD, PhD
(Updated: 5/6/2015)
Click here to contact Jon Mark Hirshon, MPH, MD, PhD
In 2011, approximately 630,00 children under 15 died from unintentional injuries. Injuries are the leading cause of childhood deaths in children over 9 years old. Ninety-five percent of these childhood injuries occur in lower- and middle-income countries.
The 2008 World Report on Child Injury Prevention listed the following as the top five causes of pediatric injury deaths globally:
1) Road Crashes- approximately 260,000/year
2) Drowning- approximately 175,0000/year
3) Burns- approximately 96,000/year
4) Falls- approximately 47,000/year
5) Poisoning (unintentional)- approximately 45,000/year
Many of these deaths occur around the home and could be prevented through proven prevention measures, which include:
· Child appropriate seatbelts and helmets
· Separate children from vehicular traffic
· Limit hot tap water temperature
· Placing medications and potentially harmful household products in child proof containers
· Draining unnecessary water from baths and buckets
· Redesigning nursery furniture, toys and playground equipment
· Strengthening emergency medical services
http://www.who.int/violence_injury_prevention/child/injury/en/
http://www.who.int/violence_injury_prevention/child/injury/world_report/report/en/
Category: Critical Care
Posted: 4/14/2015 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
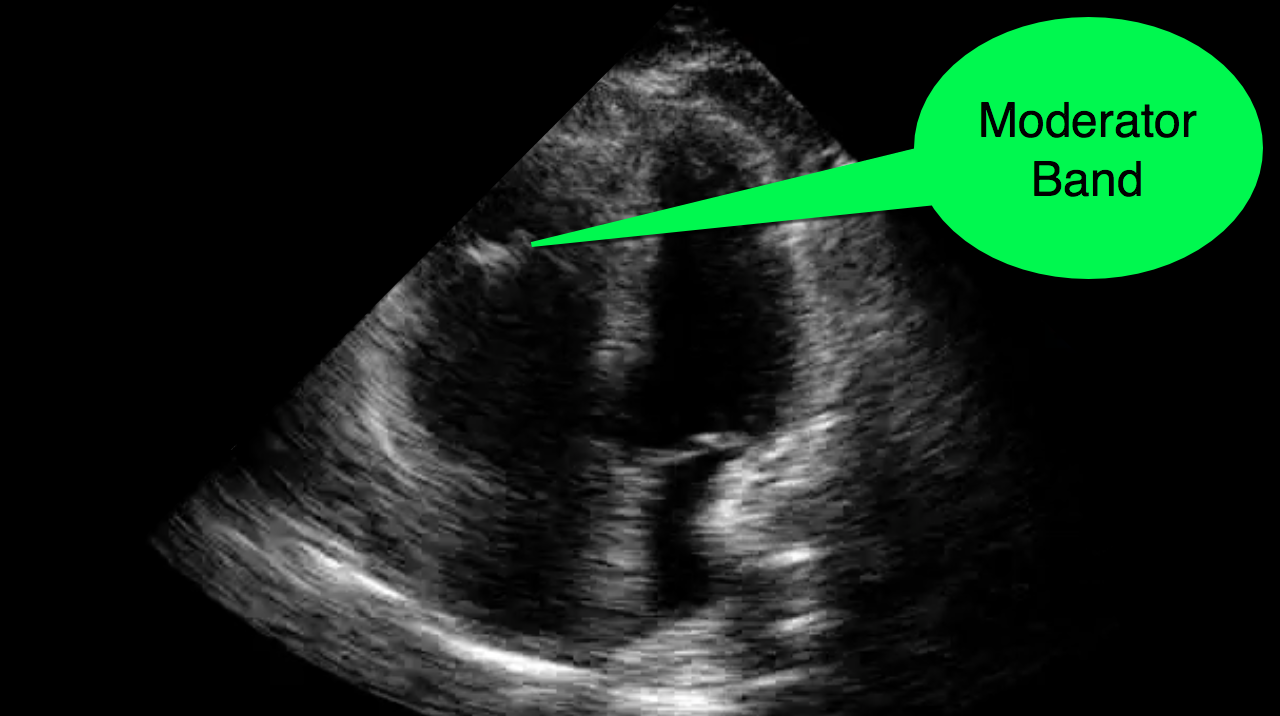
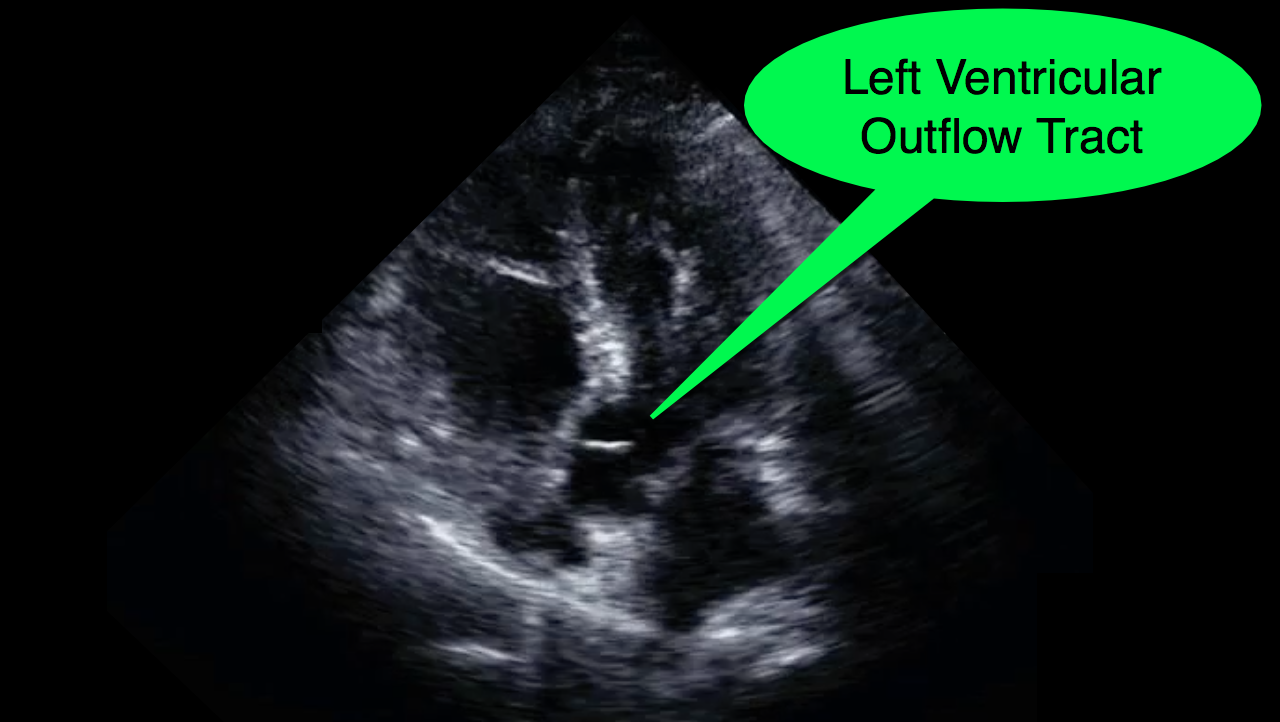
You decide to do a R.U.S.H. exam on your hypotensive patient and perform an apical four-chamber view.You see one of the two clips below; are there any tricks to figure out which is the left ventricle and which is the right ventricle?

Tricks to distinguish the RV from LV in apical four-chamber view
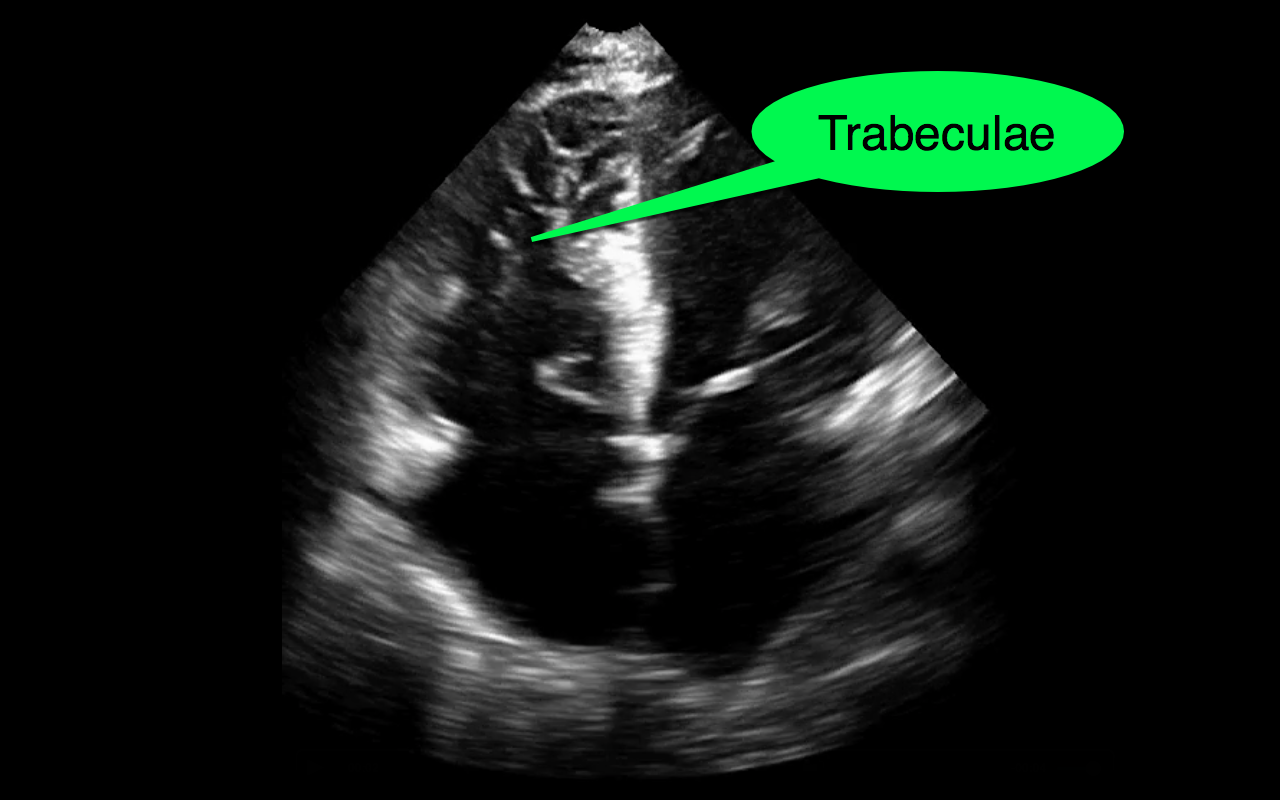
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Visual Diagnosis
Posted: 4/13/2015 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
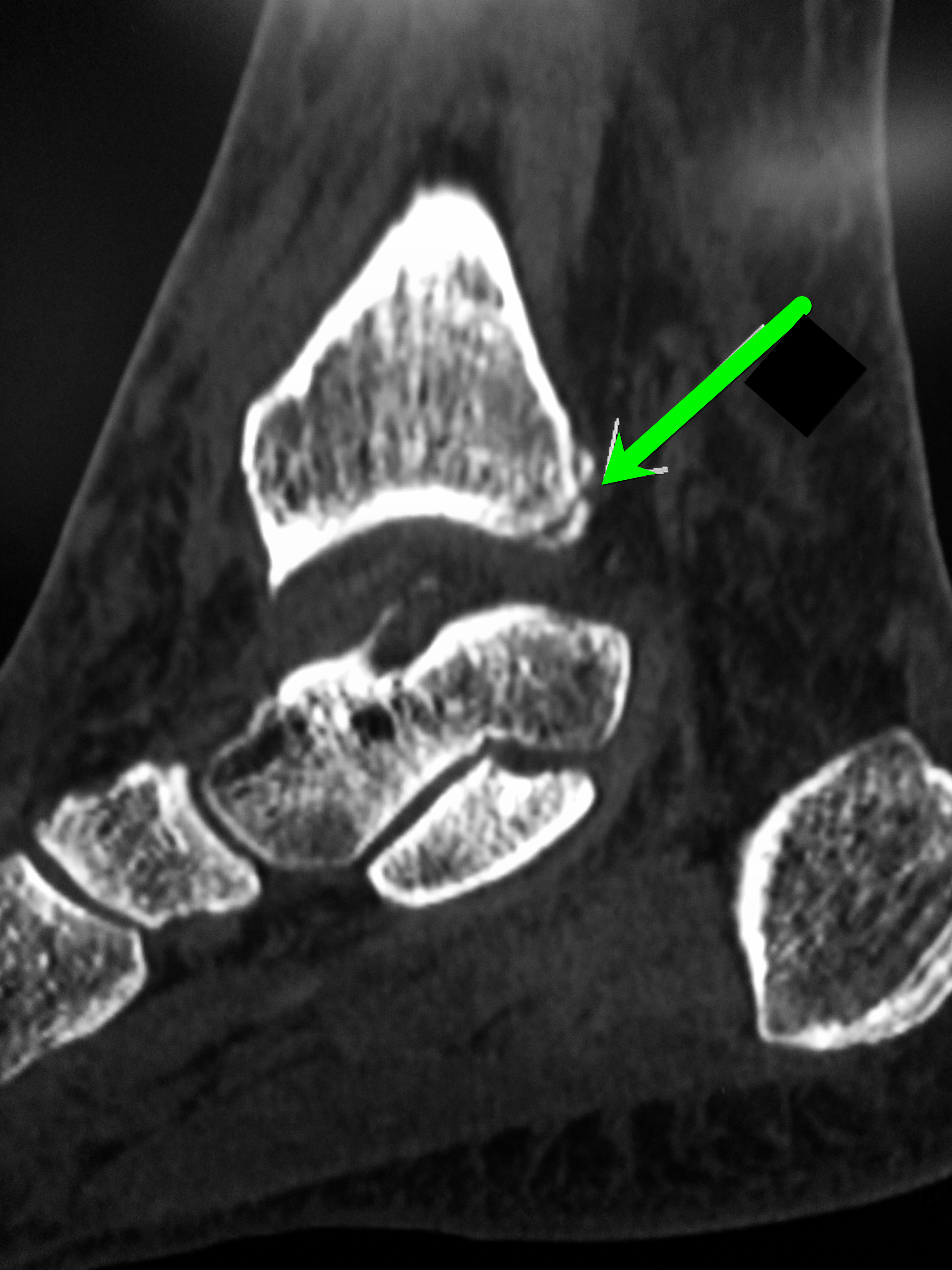
Patient presents with leg and ankle pain after a fall 3 weeks earlier. Initial ankle Xrays were negative. Patient presents today with persistent leg and ankle pain. What's the diagnosis and what other imaging would you perform and why?

Proximal fibula fracture; have a high-clinical suspicion for a Maisonneuve fracture and consider CT scan of the ankle
Maisonneuve fracture
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Toxicology
Keywords: Delirium tremens, DTs, alcohol withdrawal, seizures (PubMed Search)
Posted: 4/7/2015 by Bryan Hayes, PharmD
(Updated: 4/9/2015)
Click here to contact Bryan Hayes, PharmD
A new study from South Korea identified 3 potential clinical predictors of developing delirium tremens in patients presenting to the ED with alcohol withdrawal seizures.
If one or more is present, these findings may help assess alcohol withdrawal patients for the risk of developing DTs.
Application to Clinical Practice
Kim DW, et al. Clinical predictors for delirium tremens in patients with alcohol withdrawal seizures. Am J Emerg Med 2015 Feb 23. [Epub ahead of print, PMID 25745798]
Follow me on Twitter (@PharmERToxGuy) or Google Plus (+bryanhayes13)
Category: Neurology
Keywords: Intracerebral hemorrhage, ICH score, prognostication, early decisions to limit medical treatment (PubMed Search)
Posted: 4/8/2015 by WanTsu Wendy Chang, MD
(Updated: 10/14/2015)
Click here to contact WanTsu Wendy Chang, MD
Prognostication in intracerebral hemorrhage - A self-fulfilling prophecy?
The ICH Score is a validated outcome prediction model for intracerebral hemorrhage (ICH) developed from clinical and neuroimaging characteristics on presentation.
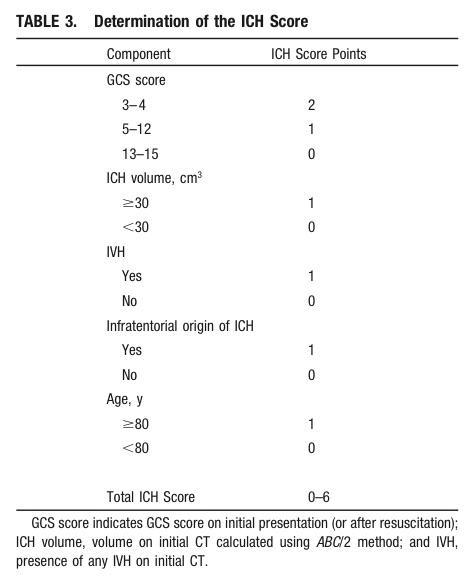
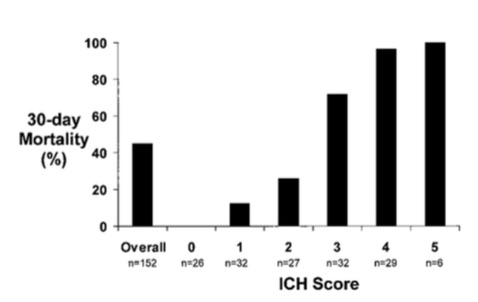
While predictive models are often used in clinical care for prognostication, is it a self-fulfilling prophecy to make early decisions to limit medical treatments based on these models?
Morgenstern et al. conducted an observational study across 5 hospitals looking at 30-day mortality of patients with ICH with initial GCS <12 who received full medical care for at least 5-days following symptom onset.
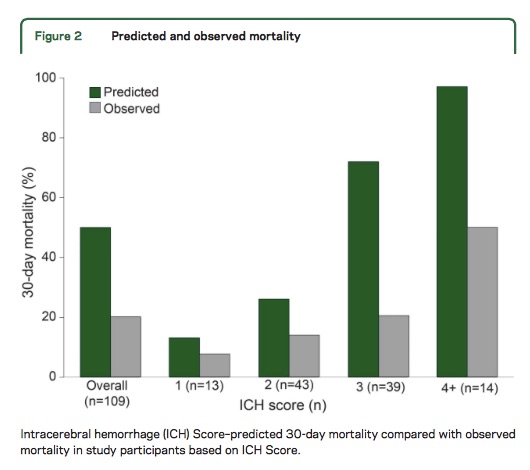
Take Home Point: The ICH Score is a useful tool for stratifying patient severity, but one should be cautious in using the model to provide specific numerical values as outcome predictions.
Hemphill JC, Bonovich DC, Besmertis L, Manley GT, Johnston SC. The ICH Score. A simple, reliable grading scale for intracerebral hemorrhage. Stroke 2001;32:891-897.
Morgenstern LB, Zahuranec DB, Sanchez, BN, et al. Full medical support for intracerebral hemorrhage. Neurology 2015;84:1-6.
Follow me on Twitter @EM_NCC
Category: Critical Care
Keywords: NIPPV (PubMed Search)
Posted: 4/7/2015 by Feras Khan, MD
Click here to contact Feras Khan, MD
Cabrini L et al. Noninvasive ventilation and survival in acute care settings: a comprehensive systematic review and metaanalysis of randomized controlled trials. Crit Care Med 2015; 43:880-888.
Category: Visual Diagnosis
Posted: 4/6/2015 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
25 year-old male with the acute onset of right flank pain. Ultrasound of the right flank is shown. What's the diagnosis?
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Cardiology
Posted: 4/5/2015 by Semhar Tewelde, MD
(Updated: 2/2/2026)
Click here to contact Semhar Tewelde, MD
The Heart Is Just a Muscle
- Heart failure and peripheral myopathies share similar symptoms such as exertional fatigue, weakness, and dyspnea.
- The role of endomyocardial biopsy (EMB) to aid in the diagnosis of new-onset heart failure is controversial and major society guidelines recommend against this procedure in the routine evaluation of patients with heat failure.
- Nevertheless when symptoms of heart failure persist despite conventional imaging modalities and treatment one must consider uncommon conditions, such as mitochondrial disorders.
- Mitochondrial disorders are characterized as clinical syndromes and patients can present with any one of the following: ophthalmoplegia, proximal muscle weakness, isolated myopathy with exercise intolerance and myalgia, severe myopathy of infancy or childhood, or multisystem involvement with myopathy.
- Myocardial tissue is highly dependent on mitochondria for energy production and is therefore susceptible to defects in mitochondrial function. Cardiac manifestations of these syndromes include both arrhythmias and cardiomyopathy.
McGarrah R. et al. The Heart is Just a Muscle. Circulation. March 2015.
