Category: Orthopedics
Keywords: shoulder, dislocation, GONAIS (PubMed Search)
Posted: 9/19/2015 by Michael Bond, MD
Click here to contact Michael Bond, MD
Shoulder Dislocation Reduction
Do you have a chronic dislocated that frequents your ED? Are you interested in teaching them a way to relocate their shoulder without looking like Mel Gibson from Lethal Weapon, https://youtu.be/Igrdi_lhhW4, then the newly described GONAIS method might be what you are looking for.
This technique has the patient grab the top of a chair with the hand on the affected side, and then slowly equating, effectively bringing the hand and arm above their head. Once in the full squat position the patient can step backwards which should reduce the shoulder. If not they can use the opposite hand to apply pressure to push the humerus backward and reduce the location.
The full article can be found at http://bit.ly/1iZ8a9z
Gonai S, Kamio Y, Matsuoka T, Harunari M, Saito Y, Takuma K. A new autoreduction method for anterior shoulder dislocation: the GONAIS method. Am J Emerg Med. 2015 Jun 14. pii: S0735-6757(15)00492-1. doi: 10.1016/j.ajem.2015.05.053. [Epub ahead of print]
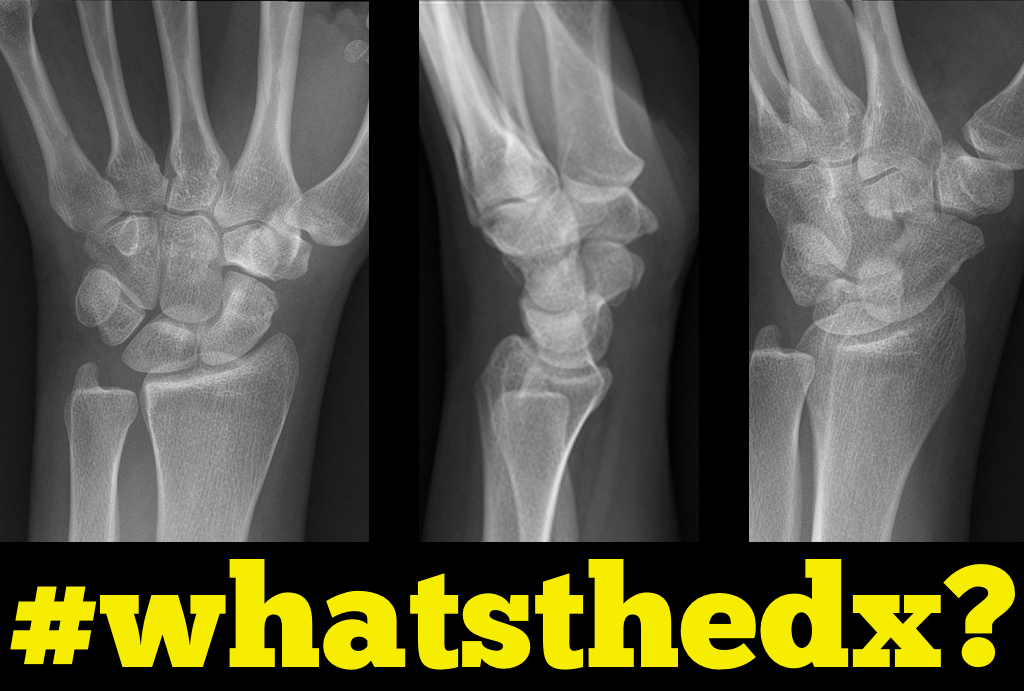
Category: Pediatrics
Keywords: wrist, fracture, trauma (PubMed Search)
Posted: 9/18/2015 by Jenny Guyther, MD
Click here to contact Jenny Guyther, MD
Is there a set of criteria similar to the Ottawa Ankle or Knee Rule that can be applied to the wrist in children?
The Amsterdam Pediatric Wrist Rules are as follows:
-Swelling of distal radius
-Visible deformity
-Painful palpation of the distal radius
-Painful palpation at the anatomical snuff box
-Painful supination
A positive answer to any of these would indicate the need for an xray.
The study referenced attempted to validate these criteria. This criteria is inclusive of the distal radius in addition to the wrist. The sensitivity and specificity were 95.9% and 37.3%, respectively in children 3 years through 18 years. This model would have resulted in a 22% absolute reduction in xrays. In a validation study, 7/170 fractures (4.1%, 95% CI: 1.7- 8.3%) would have been missed using the decision model. The fractures that were missed were all in boys ages 10-15 and were all buckle fractures and one non displaced radial fracture.
Bottom line: This rule can serve as a guide for when to obtain an xray in the setting of trauma, but it is not perfect.
Slaar et al. A clinical decision rule for the use of plain radiography in children after acute wrist injury: development and external validation of the Amsterdam Pediatric Wrist Rules. Pediatr Radiol 2015; published online August 23, 2015.
Category: Toxicology
Keywords: flushed skin (PubMed Search)
Posted: 9/16/2015 by Hong Kim, MD
(Updated: 2/2/2026)
Click here to contact Hong Kim, MD
Monosodium glutamate
Metabisulfites (Na sulfite, Na/K bisfulfite, Na/K metabisulfite, etc.)
Tyramine reaction
Niacin
Trichloroethylene
Scrombroids
Hydroxocobalamin
Category: International EM
Keywords: anthrax, plague, tularemia, botulism, dengue, bioterror (PubMed Search)
Posted: 9/14/2015 by Jon Mark Hirshon, MPH, MD, PhD
(Updated: 9/16/2015)
Click here to contact Jon Mark Hirshon, MPH, MD, PhD
Which infectious disease listed as Class A agents occur naturally, though sporadically within the U.S?
Small pox no longer occurs naturally and other viral hemorrhagic fevers occur in tropical settings.
http://www.cdc.gov/nczved/divisions/dfbmd/diseases/anthrax/technical.html
http://www.cdc.gov/plague/maps/
http://www.cdc.gov/tularemia/statistics/map.html
http://www.cdc.gov/nationalsurveillance/botulism-surveillance.html
http://www.cdc.gov/dengue/epidemiology/
http://emergency.cdc.gov/agent/vhf/
Category: Critical Care
Keywords: Simv, critical care, ventilator (PubMed Search)
Posted: 9/15/2015 by Feras Khan, MD
(Updated: 2/2/2026)
Click here to contact Feras Khan, MD
SIMV (Synchronized intermittent mandatory ventilation)
Category: Visual Diagnosis
Posted: 9/14/2015 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
35 year-old female presents to the Emergency Room with cough and chest tightness. She was discharged from the hospital yesterday for an asthma exacerbation that was secondary to pneumonia. What's the diagnosis?
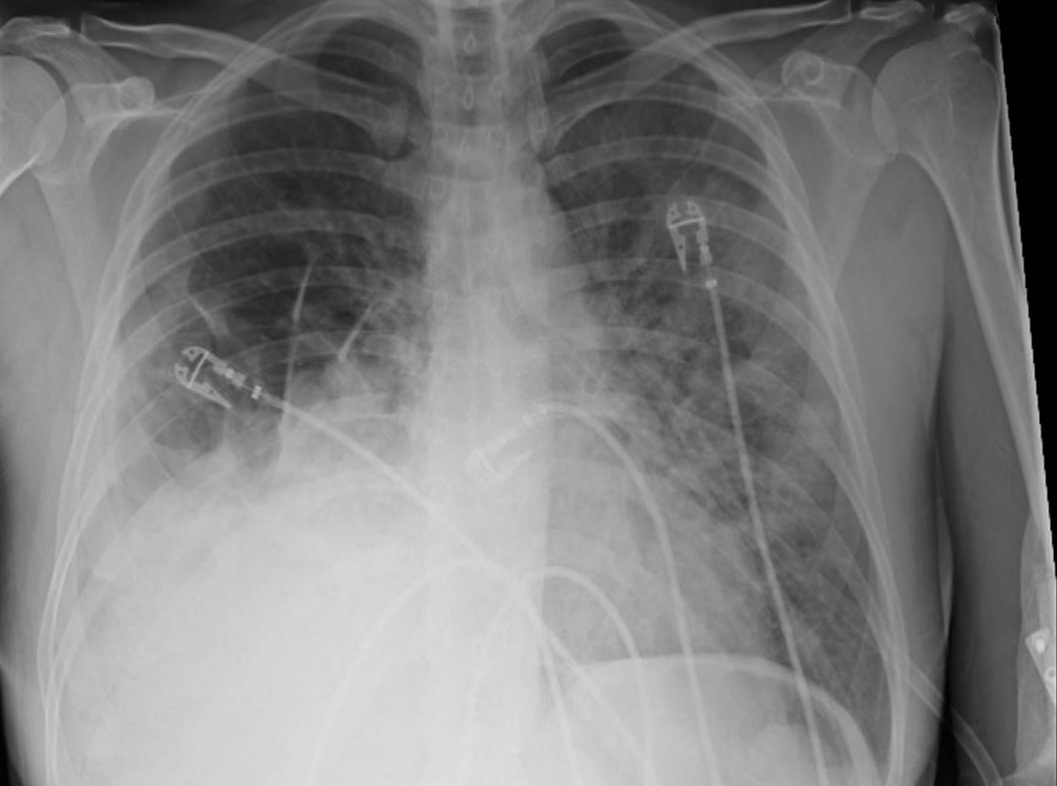
Diaphragmatic hernia
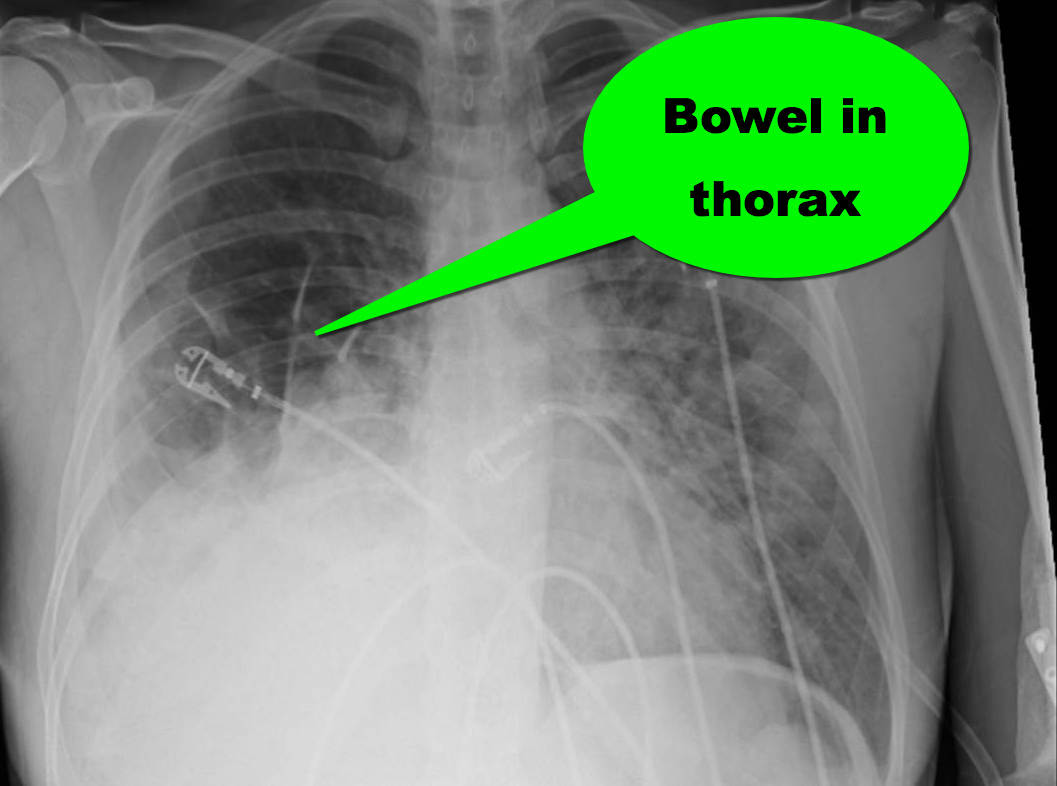
Follow me on Twitter (@criticalcarenow)
Category: Toxicology
Keywords: eye drops, pupil size, ophthalmic (PubMed Search)
Posted: 9/8/2015 by Bryan Hayes, PharmD
(Updated: 9/11/2015)
Click here to contact Bryan Hayes, PharmD
In the evaluation of ED patients, it may be important to understand the effect on pupil size from the ophthalmic medications they use. Here is a summary chart of common eye drops and their effect on pupil size.
Follow me on Twitter (@PharmERToxGuy)
Category: Neurology
Keywords: serotonin syndrome, SSRI, autonomic hyperactivity, hyperreflexia, clonus, Hunter Criteria (PubMed Search)
Posted: 9/9/2015 by WanTsu Wendy Chang, MD
Click here to contact WanTsu Wendy Chang, MD
Serotonin Syndrome - What is It?
** Stay tuned for part 2 on what causes serotonin syndrome **
Follow me on Twitter @EM_NCC
Category: Critical Care
Posted: 9/8/2015 by Mike Winters, MBA, MD
(Updated: 2/2/2026)
Click here to contact Mike Winters, MBA, MD
Hyperoxia in the Critically Ill
Helmerhorst HJF, et al. Association between arterial hyperoxia and outcomes in subsets of critical illness: A systematic review, meta-analysis, and meta-regression of cohort studies. Crit Care Med 2015; 43:1508-19.
Category: Visual Diagnosis
Posted: 9/6/2015 by Haney Mallemat, MD
(Updated: 9/7/2015)
Click here to contact Haney Mallemat, MD
68 year-old man presents with a new-onset seizure. What's the diagnosis and what's in your differential diagnosis?
Ring-enhancing lesion
Differential diagnosis of a ring-enhancing lesion
| Neoplasm | Infectious | Neurologic |
| Primary brain tumor | Pyogenic Abscess | Multiple Sclerosis |
| Primary CNS lymphoma | Tuberculoma | Sarcoidosis |
| Metastatic disease | Syphilis | Vasculitis |
| Neurocysticercosis | Aneurysm | |
| Toxoplasmosis | Resolving hematoma | |
| Nocardiosis | Cerebral infarct | |
| Cyptococcocus | Post-op changes | |
| Aspergillosis |
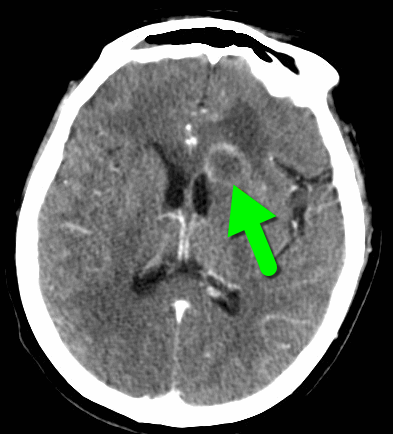
Follow me on Twitter (@criticalcarenow)
Category: Pharmacology & Therapeutics
Keywords: ketamine, analgesia, morphine, pain (PubMed Search)
Posted: 8/30/2015 by Bryan Hayes, PharmD
(Updated: 9/5/2015)
Click here to contact Bryan Hayes, PharmD
A new prospective, randomized, double-blind trial compared subdissociative ketamine to morphine for acute pain in the ED.
What they did
What they found
Motov S, et al. Intravenous subdissociative-dose ketamine versus morphine for analgesia in the emergency department: a randomized controlled trial. Ann Emerg Med 2015;66:222-9. [PMID 25817884]
Follow me on Twitter (@PharmERToxGuy)
Category: International EM
Keywords: Injuries, travel (PubMed Search)
Posted: 9/3/2015 by Jon Mark Hirshon, MPH, MD, PhD
Click here to contact Jon Mark Hirshon, MPH, MD, PhD
Injuries are a leading cause of morbidity and mortality globally
Injuries are the leading cause of preventable death in travelers
Bottom Line: Stay safe while travelling. The same safety habits used in the US, such as wearing your seatbelt or not drinking and driving, are important patterns while traveling.
http://wwwnc.cdc.gov/travel/yellowbook/2016/the-pre-travel-consultation/injury-prevention
Category: Critical Care
Keywords: Paracentesis, cirrhosis, ascites, critical care (PubMed Search)
Posted: 9/1/2015 by Daniel Haase, MD
Click here to contact Daniel Haase, MD
Your ESLD patient is hypotensive with a tense abdomen, and he needs a paracentesis!
--ALWAYS use ultrasound to localize a fluid pocket [Fig 1]! Take the time to use color Doppler to look for underlying abdominal wall varices [Fig 2]. Cirrhotic patients frequently have abnormal abdominal wall vasculature [1-2].
--Hemorrhage from paracentesis is exceedingly rare, and reversal of mild coagulopathy probably isn't that important [3-4].
--In hypotensive patients, consider placement of a small pigtail catheter for slow, continuous drainage (e.g. 8.3F pericardiocentesis catheter) instead of large-volume paracentesis. Non-tunneled catheter infection risk goes up after 72h [5].
--Albumin replacement improves mortality and incidence of renal failure in patients with SBP or other infection [6-7].
1. Hatch N, Wu TS, Barr L, Roque PJ. Advanced ultrasound procedures. Crit Care Clin. 2014 Apr;30(2):305-29, vi. doi: 10.1016/j.ccc.2013.10.005. Epub 2013 Dec 4. Review. PubMed PMID: 24606778.
2. Thomsen TW, Shaffer RW, White B, Setnik GS. Videos in clinical medicine. Paracentesis. N Engl J Med. 2006 Nov 9;355(19):e21. Erratum in: N Engl J Med. 2007 Feb 15;356(7):760. PubMed PMID: 17093242.
3. Pache I, Bilodeau M. Severe haemorrhage following abdominal paracentesis for ascites in patients with liver disease. Aliment Pharmacol Ther. 2005 Mar 1;21(5):525-9. PubMed PMID: 15740535.
4. McVay PA, Toy PT. Lack of increased bleeding after paracentesis and thoracentesis in patients with mild coagulation abnormalities. Transfusion. 1991 Feb;31(2):164-71. PubMed PMID: 1996485.
5. Nadir A, Van Thiel DH. Frequency of peritoneal infections among patients undergoing continuous paracentesis with an indwelling catheter. J Ayub Med Coll Abbottabad. 2010 Jan-Mar;22(1):37-41.
6. Kwok CS, Krupa L, Mahtani A, Kaye D, Rushbrook SM, Phillips MG, Gelson W. Albumin reduces paracentesis-induced circulatory dysfunction and reduces death and renal impairment among patients with cirrhosis and infection: a systematic review and meta-analysis. Biomed Res Int. 2013;2013:295153. doi: 10.1155/2013/295153. Epub 2013 Oct 8. Review. PubMed PMID: 24222902; PubMed Central PMCID: PMC3816020.
7. Sort P, Navasa M, Arroyo V, Aldeguer X, Planas R, Ruiz-del-Arbol L, Castells L, Vargas V, Soriano G, Guevara M, Gin s P, Rod s J. Effect of intravenous albumin on renal impairment and mortality in patients with cirrhosis and spontaneous bacterial peritonitis. N Engl J Med. 1999 Aug 5;341(6):403-9. PubMed PMID: 10432325.
Category: Visual Diagnosis
Posted: 8/31/2015 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
Person presents following a fall on an outstretched hand and there is snuffbox tenderness. What's the diagnosis?
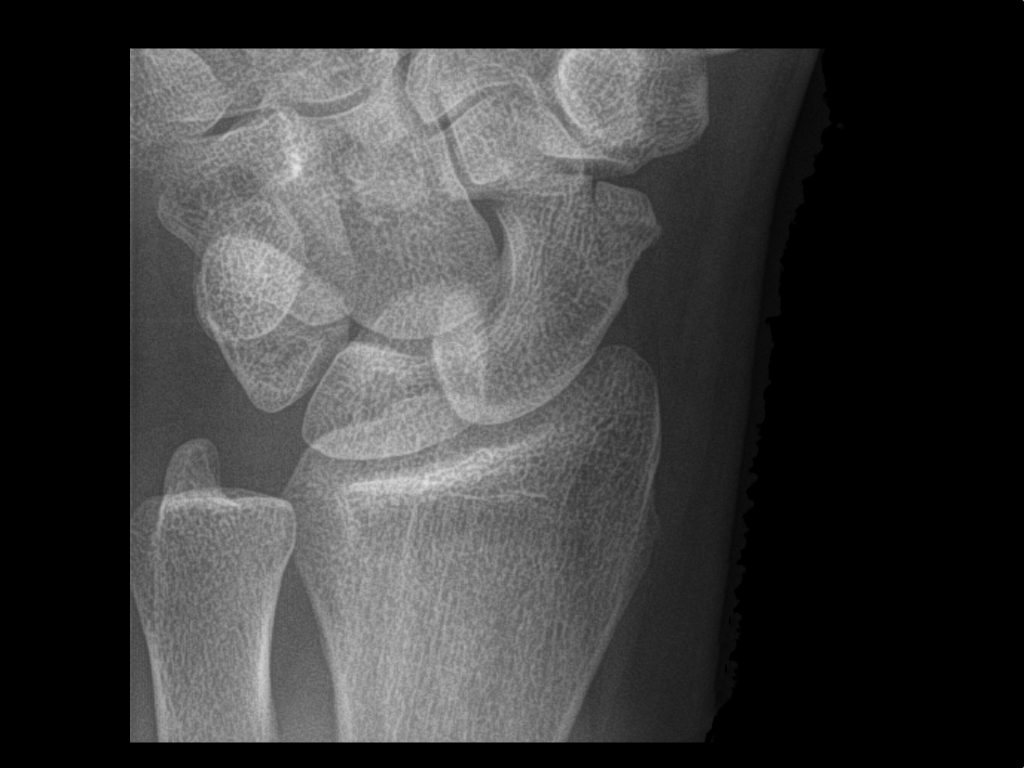
Scaphoid fracture

Follow me on Twitter (@criticalcarenow)
Category: Orthopedics
Keywords: policeman, heel, contusion (PubMed Search)
Posted: 8/29/2015 by Michael Bond, MD
(Updated: 2/2/2026)
Click here to contact Michael Bond, MD
Policeman's Heel:
When patient's present complaining of heel pain we often think immediately of plantar fascititis,and heel spurs. If they jumped and landed on the heel with are concerned for calcaneal fracture. However, a policeman's heel can occur from repetitive bounding of the heel or from landing on it as in a fall or jump.
Policeman's heel has been descirbed as a plantar calcaneal bursitis, inflammation of the sack of fluid (bursa) under the heel bone, or a contusion of the heel bone due to flattening and displacement of the heel fat pad, which leaves a thinner protective layer allowing the bone to get bruised.
Regardless of cause this responds well to NSAIDs, limiting weight bearing, or taping the foot. If the repetitive activity is not reduced this can easily become a chronic cause of heel pain. A short video showing how to tape the foot can be found at https://youtu.be/nQtkwfJrhXo
Category: Pediatrics
Keywords: UA, clean catch (PubMed Search)
Posted: 8/29/2015 by Mimi Lu, MD
Click here to contact Mimi Lu, MD
Making the wee patient pee – a non invasive urinary collection technique in the newborn
Obtaining a urinary sample in a neonate can be challenging and time consuming. The most commonly used non-invasive technique is urine collection using a sterile bag. This technique is limited by patient discomfort and contamination of the urinary sample. Catheterisation and needle aspiration are other options, but are more invasive.
A prospective feasibility and safety study enrolled 90 admitted infants aged under 30 days who needed a urine sample into the study [1]. They performed the following stimulation technique.
1. Feed the baby through breast-feeding or an appropriate amount of formula for their age and weight.
2. Wait twenty-five minutes. After twenty-five minutes clean the infant’s genitals thoroughly with warm water and soap. Dry with sterile gauze.
3. Have an assistant hold a sterile urine container near the infant
4. Hold the baby under their armpits with their legs dangling (if short handed, parents can do this)
5. Gently tap the suprapubic area at a frequency of 100 taps or blows per minute for 30 seconds
6. Massage the lumbar paravertebral zone lightly for 30 seconds
7. Repeat both techniques until micturition starts. Collect midstream urine in the sterile container
In the study, success was defined as obtaining a midstream urinary sample within 5 minutes after initiation of the stimulation procedure. There was a 86% success rate (n=69/80). Mean time to sample collection was 57 seconds. There were no complications, but controlled crying occurred in 100% of infants. The study was limited by the lack of a control group. Previous studies have described longer collection times with traditional non invasive techniques, up to over an hour [2].
Conclusion
Consider the above mentioned stimulation technique to obtain a urinary sample in the neonate.
1. Herreros Fernández ML, González Merino N, Tagarro García A, et al. A new technique for fast and safe collection of urine in newborns. Arch Dis Child. 2013 Jan;98(1):27-9. http://www.ncbi.nlm.nih.gov/pubmed/23172785
2. Davies P, Greenwood R, Benger J. Randomised trial of a vibrating bladder stimulator--the time to pee study. Arch Dis Child. 2008 May;93(5):423-4. http://www.ncbi.nlm.nih.gov/pubmed/18192318
Category: Neurology
Keywords: migraine, headache, opioids, dopamine antagonist (PubMed Search)
Posted: 8/26/2015 by Danya Khoujah, MBBS
Click here to contact Danya Khoujah, MBBS
Status migrainosus is a migraine that lasts more than 72 hours, and can be rather challenging to control. A few tips to tackle this are:
1. Adequately hydrate all patients (IV fluids are usually required, especially with severe nausea/vomiting)
2. Establish realistic expectations for the patient. A patient with chronic daily headaches will not be pain-free in the ED.
3. Use IV nonopioid medications for pain control
1st Line:
- Dopamine Antagonists: in increasing efficacy
- Metoclopramide
- Phenothiazines: prochlorperazine, promethazine and chlorpromazine
- Butyrophenones: droperidol and haloperidol
- NSAIDs: such as Ketorolac IV or IM
2nd Line:
- Corticosteroids: Do not treat the migraine in the ED, but prevent headache recurrence within 72 hours.
- Magnesium Sulfate: Has shown mixed efficacy. More likely to have a sustained benefit in patient with serum magnesium level of 1.3mg/dL or less.
- Valrpoic Acid: Be careful of combining it with Topiramate.
- Vasoconstrictors: Triptans, ergotamine, dihydroergotamine. Effective, but use is limited by contraindications.
- Opioids: Last resort
Category: Critical Care
Posted: 8/25/2015 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
The RV is a low-pressure chamber that doesn’t tolerate acute increases in pulmonary pressures (e.g., ARDS, pulmonary embolism, etc.); acute increases can lead to RV dysfunction / failure
Managing RV dysfunction requires a three-pronged approach:
Follow me on Twitter (@criticalcarenow)
Category: Visual Diagnosis
Posted: 8/24/2015 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
You find this interesting view while scanning a patient. Which view is this and why should you care about it?
This is the right ventricular inflow view
Follow me on Twitter (@criticalcarenow)
Category: Orthopedics
Keywords: Sodium Supplementation, Exercise-Associated Hyponatremia, Prolonged Exercise (PubMed Search)
Posted: 8/22/2015 by Brian Corwell, MD
Click here to contact Brian Corwell, MD
Sodium Supplementation and Exercise-Associated Hyponatremia (EAH) during Prolonged Exercise (ultramarathon running)
Weight loss of around 4% body weight (relative to pre race weight) can be anticipated to maintain euhydration in such a prolonged event
Those who become symptomatic with EAH have either gained weight or lost less that 3-4% body weight
Overhydration rather than inadequate supplemental sodium intake is a greater contributor to the development of EAH
There is a suggested link between EAH and rhabdomyolysis. The mechanism remains unknown and it is unclear which condition may augment the other. Further research is needed.
Take home: Avoid overhydration during prolonged exercise to prevent EAH.
Sodium Supplementation and Exercise-Associated Hyponatremia (EAH) during Prolonged Exercise (ultramarathon running) Hoffman and Stuempfle 2015.
