Category: International EM
Keywords: Zika, flavivirus, travel, infectious diseases (PubMed Search)
Posted: 1/20/2016 by Jon Mark Hirshon, MPH, MD, PhD
Click here to contact Jon Mark Hirshon, MPH, MD, PhD
Zika virus is a mosquito-borne flavivirus.
While outbreaks have been previously reported in Africa, Asia and the islands of the Pacific, it was first reported in the Western Hemisphere in May 2015.
Clinical Disease:
Diagnosis and Treatment
Prevention
http://emergency.cdc.gov/han/han00385.asp
Category: Critical Care
Keywords: Pulmonary Embolism, PE, submassive PE, thrombolysis, catheter-directed thromblysis, thrombectomy, echo (PubMed Search)
Posted: 1/19/2016 by Daniel Haase, MD
(Updated: 2/10/2016)
Click here to contact Daniel Haase, MD
What classifies "submassive PE"?
Submassive PE has early benefit from systemic thrombolysis at the cost of increased bleeding [1].
Ultrasound-accelerated, catheter-directed thrombolysis (USAT) [the EKOS catheters] has been shown to be safe, with low mortality and bleeding risk, as well as immediately improved RV dilation and clot burden [2-4]. USAT may improve pulmonary hypertension [4].
USAT is superior to heparin/anti-coagulation alone for submassive PE at reversing RV dilation at 24 hours without increased bleeding risk [5].
Long-term studies evaluating chronic thromboembolic pulmonary hypertension (CTEPH) need to be done, comparing USAT with systemic thrombolysis and surgical thombectomy.
Take-home: In patients with submassive PE, USAT should be considered over systemic thombolysis or anti-coagulation alone.
1. PEITHO Investigators. Fibrinolysis for patients with intermediate-risk pulmonary embolism. N Engl J Med. 2014 Apr 10;370(15):1402-11.
2. Engelhardt TC, Taylor AJ, et al. Catheter-directed ultrasound-accelerated thrombolysis for the treatment of acute pulmonary embolism. Thromb Res. 2011 Aug;128(2):149-54
3. Bagla S, Smirniotopoulos JB, et al. Ultrasound-accelerated catheter-directed thrombolysis for acute submassive pulmonary embolism. J Vasc Interv Radiol. 2015 Jul;26(7):1001-6.
4. SEATTLE II Investigators. A Prospective, Single-Arm, Multicenter Trial of Ultrasound-Facilitated, Catheter-Directed, Low-Dose Fibrinolysis for Acute Massive and Submassive Pulmonary Embolism: The SEATTLE II Study. JACC Cardiovasc Interv. 2015 Aug 24;8(10):1382-92.
5. Kucher N, Boekstegers P,et al. Randomized, controlled trial of ultrasound-assisted catheter-directed thrombolysis for acute intermediate-risk pulmonary embolism. Circulation. 2014 Jan 28;129(4):479-86.
Category: Visual Diagnosis
Posted: 1/18/2016 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
23 year-old female presents complaining of progressive right lower quadrant pain after doing "vigorous" exercise. CT abdomen/pelvis below. What’s the diagnosis? (Hint: it’s not appendicitis)

Rectus sheath hematoma
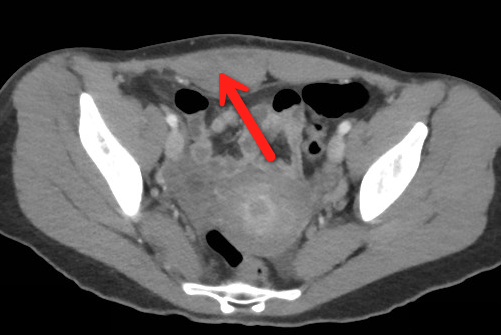
Rectus Sheath Hematoma (RSH)
Rectus muscle tear causing damage to the superior or inferior epigastric arteries with subsequent bleeding into the rectus sheath; uncommon cause of abdominal pain but mimics almost any abdominal condition.
Diagnose with CT, but try using ultrasound (thanks Dr. Joseph Minardi)
May occur spontaneously, but suspect with the following risk factors:
Typically a self-limiting condition, but hypovolemic shock may result from significant hematoma expansion.
Hemodynamically stable (non-expanding hematoma): conservative treatment (rest, analgesia, and ice)
Hemodynamically unstable (expanding hematoma): treat with fluid resuscitation, reversal of coagulopathy, and transfusion of blood products.
Follow me on Twitter (@criticalcarenow)
Category: Orthopedics
Keywords: Salter Harris, pediatric, fracture (PubMed Search)
Posted: 1/16/2016 by Michael Bond, MD
(Updated: 1/19/2016)
Click here to contact Michael Bond, MD
The Salter Harris Classification System is used in pediatric epiphyseal fractures. The higher the type of fracture the greater the risk of complications and growth disturbance.
Some common exam facts about Salter Harris Fractures are:
The Classification system as listed by Type:
For Maite, a helpful mnemonic is SALTR , Slipped (Type I), Above (Type II), Lower (Type III), Through (Type IV), and Ruined or Rammed (Type V)
A image of the fractures can be found on FP Notebook at http://www.fpnotebook.com/ortho/fracture/ephyslfrctr.htm
Category: Pediatrics
Keywords: etomidate, sedation (PubMed Search)
Posted: 1/15/2016 by Jenny Guyther, MD
Click here to contact Jenny Guyther, MD
ED study of 60 pediatric patients for procedural sedation
Bottom line: Etomidate can achieve effective sedation in children for a short procedure. Although respiratory effects were noted, none of them required assisted ventilation.
Mandt MJ, Roback MG, Bajaj L, Galinkin JL, Gao D, Wathen JE. Etomidate for short pediatric procedures in the emergency department. Pediatr Emerg Care. 2012 Sep;28(9):898-904.
Category: Toxicology
Keywords: acetaminophen, acetylcysteine (PubMed Search)
Posted: 1/7/2016 by Bryan Hayes, PharmD
(Updated: 1/14/2016)
Click here to contact Bryan Hayes, PharmD
The three-bag IV acetylcysteine regimen for acetaminophen overdose is complicated and can result in medication/administration errors. [1] Two recent studies have attempted simplifying the regimen using a two-bag approach and evaluated its effect on adverse effects. [2, 3]
Study 1 [2]
Prospective comparison of cases using a 20 h, two-bag regimen (200 mg/kg over 4 h followed by 100 mg/kg over 16 h) to an historical cohort treated with the 21 h three-bag IV regimen (150 mg/kg over 1 h, 50 mg/kg over 4 h and 100 mg/kg over 16 h).
The two-bag 20 h acetylcysteine regimen was well tolerated and resulted in significantly fewer and milder non-allergic anaphylactic reactions than the standard three-bag regimen.
Study 2 [3]
Prospective observational study of a modified 2-phase acetylcysteine protocol. The first infusion was 200 mg/kg over 4-9 h. The second infusion was 100 mg/kg over 16 h. Pre-defined outcomes were frequency of adverse reactions (systemic hypersensitivity reactions or gastrointestinal); proportion with ALT > 1000 U/L or abnormal ALT.
The 2-phase acetylcysteine infusion protocol resulted in fewer reactions in patients with toxic paracetamol concentrations.
Final word: Two-bag regimens seem to offer advantages compared to the traditional three-bag regimen with regard to reduced adverse drug reactions. Look for more data, particularly on effectiveness, and a potential transition to a two-bag approach in the future.
Follow me on Twitter (@PharmERToxGuy)
Category: Neurology
Keywords: Traumatic brain injury, psychiatric disorders, anxiety, depression (PubMed Search)
Posted: 1/13/2016 by WanTsu Wendy Chang, MD
Click here to contact WanTsu Wendy Chang, MD
Bottom Line:
Scholten AC, Haagsma JA, Cnossen MC, et al. Prevalence and risk factors of anxiety and depressive disorders following traumatic brain injury: a systematic review. J Neurotrauma. 2016 Jan 5. [Epub ahead of print]
Follow me on Twitter @EM_NCC
Category: Critical Care
Posted: 1/12/2016 by Haney Mallemat, MD
(Updated: 1/16/2016)
Click here to contact Haney Mallemat, MD
There are so many variables to monitor during CPR; speed and depth of compressions, rhythm analysis, etc. But how much attention do you give to the ventilations administered?
The right ventricle (RV) fills secondary to the negative pressure created during spontaneously breathing. However, during CPR we administer positive pressure ventilation (PPV), which increase intra-thoracic pressure thus reducing venous return to the RV, decreasing cardiac output, and coronary filling. PPV also increases intracranial pressure by reducing venous return from the brain.
So our goal for ventilations during cardiac arrest should be to minimize the intra-thoracic pressure (ITP); we can do this by remembering to ventilate "low (tidal volumes) and slow (respiratory rates)"
Follow me on Twitter (@criticalcarenow)
Category: Visual Diagnosis
Posted: 1/11/2016 by Haney Mallemat, MD
(Updated: 3/10/2016)
Click here to contact Haney Mallemat, MD
What’s the name of this CT finding and name two potential causes?

Pneumobilia (air in the biliary tree). Be careful, this must be distinguished from portal venous gas.
Diagnoses to consider when pneumobilia is present:
Category: Orthopedics
Keywords: Heel pain (PubMed Search)
Posted: 1/9/2016 by Brian Corwell, MD
Click here to contact Brian Corwell, MD
Sever's disease also known as calcaneal apophysitis, is the most common cause of heel pain in the young adolescent (ages 8 to 12).
It can be thought of as the Achilles tendon equivalent of Osgood-Schlatter's disease (patellar tendon insertion pain).
It is a non inflammatory chronic repetitive injury.
Commonly seen bilaterally in up to two -thirds of cases.
Patients will complain of activity related pain to the heel.
There may be tenderness and local swelling at the Achilles tendon insertion.
Radiographs are not necessary for acute cases.
Treat with activity modification, heel raise, physical therapy.
Category: Toxicology
Keywords: Caffeine, Energy drinks (PubMed Search)
Posted: 1/7/2016 by Kathy Prybys, MD
(Updated: 1/8/2016)
Click here to contact Kathy Prybys, MD
Caffeine is the most commonly used psychoactive substance in the world. It is widely available in coffee, tea, chocolate,soft drinks, OTC medicines, and energy drinks. The vast majority of people consuming caffeine appear to suffer no harm while enjoying it's stimulating effects. This has led to the widely held perspective that caffeine is a completely benign substance with no adverse health effects exists.
Although, children and adolescents are at particular risk, many caffeine containing products are specifically marketed at them. Alarmingly, statistics demonstrate that caffeine intake among children and adolescents has increased by 70% in the last 30 years. Energy drinks are of special concern as they represent the fastest growing component of the beverage industry, contain significant quantities of caffeine as well as high levels of sugar, and can place children at high risk for caffeine intoxication.
There are many negative health consequences documented with caffeine use which occur in a dose dependent manner with individuals differing in their susceptibility to caffeine-related adverse effects:
Chronic Effects:
Category: International EM
Keywords: Burns, low- and middle-income countries, disease burden (PubMed Search)
Posted: 1/6/2016 by Jon Mark Hirshon, MPH, MD, PhD
(Updated: 1/16/2016)
Click here to contact Jon Mark Hirshon, MPH, MD, PhD
Every year approximately 265,000 people die from burns
· The vast majority occur in low- and middle-income countries
o The rate of child death from burns is 7 times worse in low- and middle-income countries compared to high income countries
· Almost half of all fatal burns occur in the WHO South-East Asia Region
Non-fatal burns are a leading cause of global morbidity
· In 2004, almost 11 million individuals worldwide were burned badly enough to require medical attention
Unlike many other unintentional injuries, burns occur:
· Mainly in the home and workplace
o Women are at greater risk secondary to open fire cooking
· Approximately equally among men and women
o Most other injuries occur more frequently in men
Most burns are preventable. Developing an effective burn prevention plan involving multiple sectors is important. Per the WHO, the plan should be broad with efforts to:
· improve awareness
· develop and enforce effective policy
· describe burden and identify risk factors
· set research priorities with promotion of promising interventions
· provide burn prevention programmes
· strengthen burn care
· strengthen capacities to carry out all of the above.
http://www.who.int/mediacentre/factsheets/fs365/en/
Category: Critical Care
Keywords: antibiotics, drug resistance, (PubMed Search)
Posted: 1/5/2016 by Feras Khan, MD
Click here to contact Feras Khan, MD
Happy New Year!!!
My new year's resolution is to use less antibiotics (and eat more Cap'n Crunch Berries)
Will I be successful?
A multi-center, ICU, observational study looking at over 900 patients from 67 ICUs showed that half of all empiric antibiotics ordered in patients are continued for at least 72 hours in the abscence of adjudicated infection.
Things to consider:
The same way we try and limit central line use, we should try and decrease antibiotic usage on a daily basis
Tips to decrease use: daily clinical pharmacist input, ID specialist involvement, automated stop dates, 72 hour vancomycin cessation protocols, incentives for de-escalation, educational resources
Thomas, Zachariah PharmD
Category: Pharmacology & Therapeutics
Keywords: sugammadex, rocuronium, NMBA, vecuronium (PubMed Search)
Posted: 12/29/2015 by Bryan Hayes, PharmD
(Updated: 1/2/2016)
Click here to contact Bryan Hayes, PharmD
After three failed attempts, the FDA finally granted approval for Merck's non-depolarizing neuromuscular blocker reversal agent sugammadex (Bridion). Though the product has been used in Europe and Asia for several years, hypersensitivity concerns led to the delayed approval in the U.S.
Important points
Application to Clinical Practice
The EM PharmD blog discusses sugammadex's approval in more detail.
Follow me on Twitter (@PharmERToxGuy)
Category: Pediatrics
Keywords: Pediatrics, Venipuncture, J-Tip, Jet-Injected, Local anesthesia, Topical anesthesia (PubMed Search)
Posted: 1/2/2016 by Christopher Lemon, MD
(Updated: 2/2/2026)
Click here to contact Christopher Lemon, MD
Many providers may not be familiar with the "J-Tip" (National Medical Products Inc, Irvine, CA) which is a needle-free jet injection system that uses air to push buffered lidocaine into the skin. In theory, it provides quick local anesthesia without a needle, making it an ideal tool to reduce the pain of pediatric venipuncture. Maybe you will consider giving it a try?...but what is the data for it?
Category: International EM
Keywords: alcohol, hangover (PubMed Search)
Posted: 12/30/2015 by Jon Mark Hirshon, MPH, MD, PhD
Click here to contact Jon Mark Hirshon, MPH, MD, PhD
In many countries, alcohol is commonly drunk for special occasions, such as New Year’s. What can be the consequences of drinking too much?
As noted in an article on the validation of the Dutch version of the brief young adult alcohol consequences questionnaire, the most common consequences were:
According to the Alcohol Hangover Research Group Consensus Statement on Best Practice in Alcohol Hangover Research, items 1, 2, 4, 6 and 9 are or may be related to hangovers.
Have an enjoyable, but safe New Year.
Validation of the Dutch version of the brief young adult alcohol consequences questionnaire (B-YAACQ). Verster JC, van Herwijnen J, Olivier B, Kahler CW. Addict Behav. 2009 May;34(5):411-4. Epub 2007 Sep 29.
The alcohol hangover research group consensus statement on best practice in alcohol hangover research. Verster JC, Stephens R, Penning R, Rohsenow D, McGeary J, Levy D, McKinney A, Finnigan F, Piasecki TM, Adan A, Batty GD, Fliervoet LA, Heffernan T, Howland J, Kim DJ, Kruisselbrink LD, Ling J, McGregor N, Murphy RJ, van Nuland M, Oudelaar M, Parkes A, Prat G, Reed N, Slutske WS, Smith G, Young M; Alcohol Hangover Research Group. Curr Drug Abuse Rev. 2010 Jun;3(2):116-26.
Category: Critical Care
Posted: 12/29/2015 by Mike Winters, MBA, MD
(Updated: 2/2/2026)
Click here to contact Mike Winters, MBA, MD
Acute Chest Syndrome
Cecchini J, Fartoukh M. Sickle cell disease in the ICU. Curr Opin Crit Care 2015; 21:569-75.
Category: Visual Diagnosis
Posted: 12/28/2015 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
79 year-old male with headaches, ataxia, falls, and difficulty urinating. What's the diagnosis?
Diagnosis: Ventriculomegaly secondary to Normal Pressure Hydrocephalus
An approach to ventriculomegaly
Ventriculomegaly is due to cerebral atrophy (e.g., Parkinson disease) or increased cerebrospinal fluid (CSF) within the ventricles. Increased CSF is due to:
Congenital causes of ventriculomegaly:
Acquired causes of ventriculomegaly:
Follow me on Twitter (@criticalcarenow)
Category: Orthopedics
Keywords: Adolescent, head injury (PubMed Search)
Posted: 12/26/2015 by Brian Corwell, MD
Click here to contact Brian Corwell, MD
Protracted Recovery from Concussion
Age and sex may influence concussion recovery time frame
Methods: 266 adolescent athletes presenting to a sports medicine concussion clinic
Female athletes had a longer recovery course (P=0.002) and required more treatment interventions (p<0.001).
Female athletes were more likely to require academic accommodations (p<0.001), vestibular therapy (P<0.001) and medications (P<0.001).
Be aware that not all concussion patient subgroups with concussions recover in the same manner. Further study is needed to support whether female adolescent athletes require unique management and treatment guidelines.
Category: Neurology
Keywords: CSF, LP, HSV, infection (PubMed Search)
Posted: 12/22/2015 by Danya Khoujah, MBBS
(Updated: 1/16/2016)
Click here to contact Danya Khoujah, MBBS
HSV infection of the CNS is one of few treatable viral diseases. HSV encephalitis of older children and adults is almost always caused by herpes simplex virus type 1 (HSV-1), and in individuals older than 20, is due to HSV reactivation.
Temporal lobe localization is characteristic for HSV encephalitis in individuals older than 3 months, and is responsible for its characteristic presentation, namely bizarre behavior and expressive aphasia.
CSF analysis will usually reveal an elevated protein level, and a lymphocytic cellular predominance.
CSF protein concentration is a function of disease duration, and will continue to rise even with administration of treatment (acyclovir) and may remain elevated after the completion of therapy.
5% of CSF samples will be totally normal, and the diagnosis will only be revealed with positive PCR detection of viral DNA in the CSF, which is the gold standard for diagnosis.
The sensitivity of MRI is similar to CSF analysis, with 5% of patients with HSV encephalitis having a normal MRI on presentation, and subsequently developing abnormalities.
Of note, HSV-2 tends to cause aseptic meningitis rather than encephalitis in adults, and has a benign course.
Bottom Line? Keep a high index of suspicion for HSV encephalitis, and treat the patient empirically despite a normal CSF/MRI pending PCR results.
Whitley RJ. Herpes Simplex Virus Infections of the Central Nervous System. Continuum 2015;21(6):1704 13
