Category: Pharmacology & Therapeutics
Keywords: Tranexamic acid, trauma, CRASH-2 (PubMed Search)
Posted: 1/2/2014 by Ellen Lemkin, MD, PharmD
Click here to contact Ellen Lemkin, MD, PharmD
Tranexamic acid (TXA) is an antifibrinolytic that prevents clot breakdown by inhibiting plasminogen activation and plasmin activity
The CRASH-2 trial enrolled 20,211 adult trauma patients with significant hemorrhage (SBP <90 or HR 110) or at significant risk of hemorrhage
Patients were randomized to 1 gram TXA over 10 minutes followed by an infusion of 1 gm over 8 hours vs placebo
There was a significant reduction in the relative risk off all cause mortality of 9% (14.5% vs 16%, RR 0.91, CI 0.85-0.97, p = 0.0035)
The patients that benefited most were those most severely injured, and in those treated in less than 3 hours of injury.
1. CRASH-2 Trial collaborators. Effects of tranexamic acid on death, vascular occlusive events, and blood transfusion in trauma patients with significant haemorrhage (CRASH-2): a randomized, placebo controlled trial. The Lancet. 2010; 376:23-32.
2. Cap AP, Baer DG, Orman JA, Aden J, Ryan K, Blackbourne LH, Ryan K. Tranexemic Acid for Trauma Patients: A Critical Review of the Literature. Journal of Trauma, Injury, Infection and Critical Care. July 2011 Vol 71(1):S9-S14.
Category: International EM
Keywords: International, health systems, acute care, services (PubMed Search)
Posted: 12/31/2013 by Andrea Tenner, MD
(Updated: 1/1/2014)
Click here to contact Andrea Tenner, MD
Background Information: While the concept of Emergency Medicine is fairly well understood in the United States, it is less clear in countries where the concept is not as well established. This has caused quite a bit of confusion and hindered progress and collaboration.
Pertinent Study Design and Conclusions: In a recent consensus conference held at SAEM several definitions were standardized.
Bottom Line:
It is imperative that the same terminology be used when discussing the delivery of care on a time-sensitive basis.
University of Maryland Section of Global Emergency Health
Author: Andi Tenner, MD, MPH, FACEP
Calvello EJB, Broccoli M, Risko N et al. Emergency care and health systems: consensus-based recommendations and future research priorities. Academic Emergency Medicine. 2013. 20(12): 1278-1288.
Hirshon JM, Risko N, Calvello EJ, et al. Health systems and services: the role of acute care. Bull World Health Organ. 2013. 91:386-388.
Category: Critical Care
Keywords: Left Ventricular Assist Device, LVAD, Critical Care, Cardiology, Heart Failure, Thrombosis, LVAD Complications (PubMed Search)
Posted: 12/31/2013 by John Greenwood, MD
Click here to contact John Greenwood, MD
VAD thrombosis: A Must Know VAD Complication
The HeartMate left ventricular assist device (LVAD) is one of the most frequently placed LVADs today. Originally, it was thought to have a lower incidence of thrombosis due to its mechanical design. However, a recent multi-center study published in the NEJM reported a dramatic increase in the rate of thrombosis since 2011 in the HeartMate II device. The report found:
An increase in pump thrombosis at 3 months after implantation from 2.2% to 8.4%
The median time from implantation to thrombosis was 18.6 months prior to March 2011, to 2.7 months after.
Pump thrombosis is a major cause of morbidity and mortality (up to almost 50%!!) and is a can't miss diagnosis. It's important to keep thrombosis on the differential for any VAD patient presenting with:
Power spikes or low pump flow alarms on the patient's control box
Pump (VAD) failure
Recurrent/new heart failure
Altered mental status
Hypotension (MAP < 65)
Signs of peripheral emboli (including acute CVA)
Useful lab findings suggestive of thrombosis include:
Evidence of hemolysis
LDH > 1,500 mg/dL or 2.5-3 times the upper limit of normal
Hemoglobinuria
Elevated plasma free hemoglobin
Bottom Line: In the patient with suspected VAD thrombosis, it is important to contact the patient's VAD team immediately (CT surgeon, VAD coordinator/nurse, VAD engineer). Treatment should begin with a continuous infusion of unfractionated heparin, while other treatment options can be discussed with the VAD team.
Starling RC, Moazami N, Silvestry SC, et al. Unexpected Abrupt Increase in Left Ventricular Assist Device Thrombosis. N Engl J Med. 2013.
Follow Me on Twitter: @medicalgraffiti
Email: johncgreenwood@gmail.com
Category: Visual Diagnosis
Posted: 12/30/2013 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
68 year-old male presents with weakness after surgical repair of his abdominal aorta. What’s the diagnosis and name at least one eponym for the signs displayed (there are five total)?
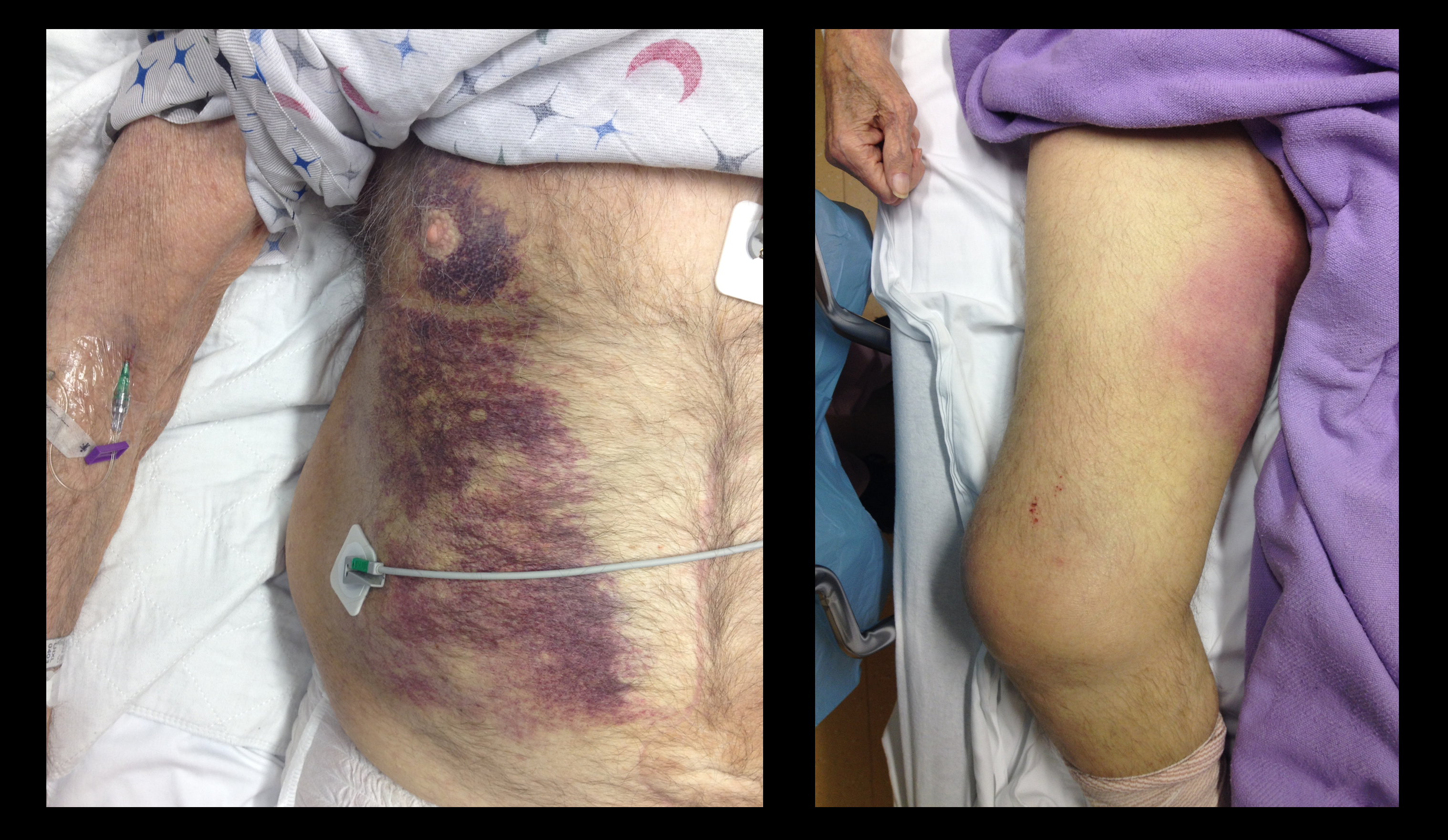
Grey-Turner and Fox's sign; these signs indicate retroperitoneal hemorrhage.

There are five signs suggesting retroperitoneal bleeding. They generally appear 24 hours after bleeding starts, occurring when blood extravasates along ligamentous connections between the retroperitoneal space and skin surface.
1. Grey-Turner Sign: Named for the surgeon who identified it in 1920; a bluish hematoma across the lateral abdominal wall when blood from the pararenal space leaks along the quadratus lumborum.
2. Fox’s Sign: Described by Dr. Fox in 1966 in two patients, (ruptured AAA and pancreatitis); ecchymosis over anteromedial thigh secondary to blood seeping along the fascia of psoas and iliacus.
3. Cullen’s Sign: Dr. Cullen (gynecologist), described this in 1918 as a sign of a ruptured ectopic pregnancy; bruise around the umbilicus from retroperitoneal blood tracking along falciform ligament.
4. Bryant’s Sign: Dr. Bryant initially described this sign; ecchymosis of the scrotum from blood tracking down the spermatic cord.
5. Stabler’s sign: Ecchymosis over the inguinal ligament
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Cardiology
Keywords: ST-elevation, Cardiology, MI (PubMed Search)
Posted: 12/29/2013 by Ali Farzad, MD
(Updated: 3/10/2014)
Click here to contact Ali Farzad, MD
There is debate and confusion regarding where and how to measure ST elevation (STE). Do you measure the STE at the J-point? Or at 40 msec after the J-point? And how much STE is considered significant? The current guidelines have clarified this issue.
- STE should be measured at the J-point.
- STEMI is defined by STE ≥ 1 mm in at least 2 contiguous leads, with the exception of leads V2-V3.
- STEMI is defined by STE ≥ 2 mm in leads V2-V3 in men.
- STEMI is defined by STE ≥ 1.5 mm in leads V2-V3 in women.
For more cardiology pearls from the 2013 literature , check out Amal Mattu's Articles You've Gotta Know!
Want more emergency cardiology pearls? Follow me @alifarzadmd
2013 ACCF/AHA Guideline for the Management of ST-Elevation Myocardial Infarction
O'Gara PT, Kushner FG, Ascheim DD, et al; American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines Circulation. 2013;127:e362-e425 Pubmed Link
Category: Orthopedics
Keywords: Diabetes, osteomyelitis (PubMed Search)
Posted: 12/29/2013 by Brian Corwell, MD
(Updated: 2/3/2026)
Click here to contact Brian Corwell, MD
No single feature of the history of physical examination reliably rules out ostemyelitis
Aids in making the diagnosis include:
An ulcer area larger than 2 cm2 (LR 7.2),
A positive probe to bone test (LR 6.4),
An ESR greater than 70 mm/h (LR 11)
Butalia S, Palda VA, Sargeant RJ, Detsky AS, Mourad O. Does this patient with diabetes have osteomyelitis of the lower extremity? JAMA. 2008 Feb 20;299(7):806-13.
Category: Pediatrics
Posted: 12/27/2013 by Mimi Lu, MD
(Updated: 12/28/2013)
Click here to contact Mimi Lu, MD
Category: Toxicology
Keywords: mercury (PubMed Search)
Posted: 12/26/2013 by Fermin Barrueto
(Updated: 2/3/2026)
Click here to contact Fermin Barrueto
Though an uncommon exposure, it can occur from chronic mercury exposure. One mode of exposure that I have seen is with elemental mercury thermometers that were broken to collect the beads of mercury - for entertainment. This occurred in a child's room and were forgotten. One child presented with personality changes and pink hands and feet. The patient suffered from severe mercury poisoning and acrodynia due to prolonged exposure to the mercury vapor.
Acrodynia or Pink Disease includes:
Irritability, shyness, photophobia, pink discoloration of the hands and feet and polyneuritis.
Category: International EM
Keywords: rabies, vaccine, immunoglobulin, infectious disease, international (PubMed Search)
Posted: 12/25/2013 by Andrea Tenner, MD
Click here to contact Andrea Tenner, MD
Case Presentation:
A 10 year old boy presents with a dog bite sustained 3 days ago, during a family trip to India. He has no prior history of vaccination and, at the time, he was taken to a local clinic where the wound was irrigated and he received a rabies vaccine.
Clinical Question:
Now that his has come to your ED 3 days later, is there anything further to be done?
Answer:
This patient should also receive rabies immunoglobulin (RIG) and complete his post-exposure prophylaxis. Post-exposure prophylaxis is a combination of rabies vaccine and rabies immunoglobulin (RIG).
RIG:
Vaccine:
Bottom Line:
University of Maryland Section of Global Emergency Health
Author: Jenny Reifel Saltzberg
http://www.cdc.gov/rabies/index.html
Gautret P, Shaw M, Gazin P, et al. Rabies postexposure prophylaxis in returned injured travelers from France, Australia, and New Zealand: a retrospective study. J Travel Med. 2008 Jan-Feb;15(1):25-30.
Hatz CF, Kuenzli E, Funk M. Rabies: relevance, prevention, and management in travel medicine. Infect Dis Clin North Am. 2012 Sep;26(3):739-53.
Category: Critical Care
Posted: 12/24/2013 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
The morbidity and mortality from pseudomonas aeruginosa infections is high and empiric double-antibiotic coverage (DAC) is sometimes given; quality evidence for this practice is lacking.
Although there is little supporting data, the following reasons have been given for DAC:
The potential harm of antibiotic overuse cannot be ignored, however, and include adverse reaction, microbial resistance, risk of super-infection with other organisms (e.g., Clostridium difficile), and cost.
There may be a signal in the literature demonstrating a survival benefit when using DAC for patients with shock, hospital-associated pneumonia, or neutropenia. The IDSA guidelines, however, do not support DAC for neutropenia alone; only with neutropenia plus pneumonia or gram-negative bacteremia.
Bottom line: Little data supports the routine use of DAC in presumed pseudomonal infection. It may be considered in patients with shock, hospital-associated pneumonia, or neutropenia (+/- pneumonia), but consult your hospital’s antibiogram or ID consultant for local practices.
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Visual Diagnosis
Posted: 12/23/2013 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
Patient with a history of osteogenesis imperfecta presents with right lateral chest pain following a sneeze. The ultrasound of his chest is shown (hint: arrow points to a rib). What's the diagnosis?
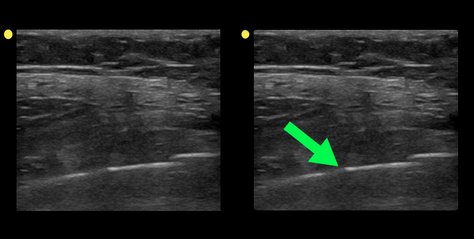
Rib fracture
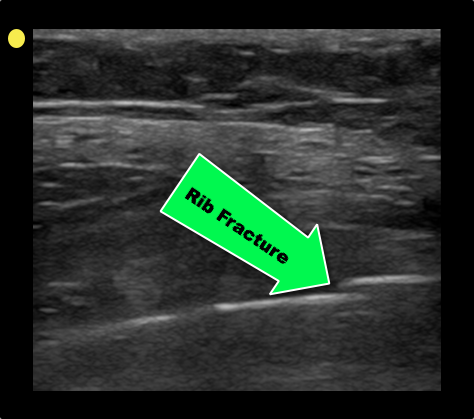
Turk F. et al. Evaluation by ultrasound of traumatic rib fractures missed by radiography. Emerg Radiol. 2010 Nov;17(6):473-7. doi: 10.1007/s10140-010-0892-9
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Cardiology
Posted: 12/22/2013 by Semhar Tewelde, MD
(Updated: 2/3/2026)
Click here to contact Semhar Tewelde, MD
Metoprolol Usage Cardioprotective
Ibanez B, Sanchez-Brunete V, Pizarro G, et al. Effect of early metoprolol on infarct size in ST-segment-elevation myocardial infarction patients undergoing primary percutaneous coronary intervention: the Effect of Metoprolol in Cardioprotection During an Acute Myocardial Infarction (METOCARD-CNIC) trial. Circulation. 2013 Oct 1; 128(14):1495-503.
Category: Pharmacology & Therapeutics
Keywords: Hypertension, treatment (PubMed Search)
Posted: 12/21/2013 by Michael Bond, MD
(Updated: 2/3/2026)
Click here to contact Michael Bond, MD
JNC8 (the Eigth Joint National Commission) released their recommendations for blood pressure management this week. The full article as published in JAMA can be found at http://jama.jamanetwork.com/article.aspx?articleid=1791497
Highlights from this report are
General Pearl: Remember to be cautious in acutely lowering the blood pressure in asymptomatic patients. Acute lowerings can cause watershed ischemia leading to strokes.
Category: Pediatrics
Posted: 12/20/2013 by Jenny Guyther, MD
(Updated: 2/3/2026)
Click here to contact Jenny Guyther, MD
Category: Toxicology
Keywords: ketamine, methoxetamine (PubMed Search)
Posted: 12/19/2013 by Fermin Barrueto
(Updated: 2/3/2026)
Click here to contact Fermin Barrueto
A new drug is coming onto the drug scene with some case reports beginning to build. The internet appears to have been a major driver or mode of distribution for this particular drug.
One study of users showed that this ketamine analog has more vivid hallucinations that would liken it to LSD. It has been theorized that this drug has the dissociative effects of ketamine but also has prominent serotninergic effects making additions more likely and hallucinations possible.
If you see a case in your ED, you can say you heard it here first!
Kjellgren A, Jonsson K. Methoxetamine (MXE)--a phenomenological study of experiences induced by a "legal high" from the internet. J Psychoactive Drugs. 2013 Jul-Aug;45(3):276-86.
Category: International EM
Keywords: Polio, Viral, Infectious, Outbreak (PubMed Search)
Posted: 12/18/2013 by Andrea Tenner, MD
Click here to contact Andrea Tenner, MD
In November 2013, the CDC issued multiple Alerts on various polio outbreaks in Asia and Africa. Countries currently with the heaviest burden are Syria, Pakistan, Somalia, Kenya, and Cameroon. Nigeria and Afghanistan have also had persistent epidemics.
General Information:
Relevance to the EM Physician:
The diagnosis can be made by detecting:
The CSF analysis results will resemble that of aseptic meningitis.
Bottom Line:
Have a high suspicion for travellers to affected regions and recognize the high prevalence of asymptomatic infection (and thus importable epidemic potential). Pre-travel vaccination is essential.
University of Maryland Section of Global Emergency Health
Author: Walid Hammad, MB ChB
McFee RB. Polio. Dis Mon. 2013 Dec;59(12):445-7. doi:10.1016/j.disamonth
Center for disease control and prevention, Travellers health http://wwwnc.cdc.gov/travel/
Category: Critical Care
Keywords: Hepatic encephalopathy, HE, liver failure, cirrhosis (PubMed Search)
Posted: 12/17/2013 by Feras Khan, MD
(Updated: 2/3/2026)
Click here to contact Feras Khan, MD
Hepatic Encephalopathy (HE)
Pathogenesis: Several theories exist that include accumulation of ammonia from the gut because of impaired hepatic clearance that can lead to accumulation of glutamine in brain astrocytes leading to swelling in patients with hepatic insufficiency from acute liver failure or cirrhosis.
Clinical Features:
Diagnostic tests: Ammonia levels are routinely drawn but must be drawn correctly without the use of a tourniquet, transported on ice, and analyzed within 20 minutes to get an accurate result. Severity of HE does not correlate with increasing levels.
Management:
1. Airway protection as needed
2. Correct precipitating factors (GI bleed, infection-SBP, hypovolemia, renal failure)
3. Consider neuro-imaging if new focal neurologic findings are found on exam
4. Correct electrolyte imbalances
5. Lactulose by mouth (PO/Naso-gastric tube or Rectally)
a. 10-30 g every 1-2 hours until bowel movement or lactulose enema (300 mL in 1 L water)
b. Facilitates conversion of NH3 to NH4+, decreases survival of urease-producing bacteria in the gut
6. Rifaximin 550 mg by mouth BID (minimally absorbed antibiotic with broad-spectrum activity)
7. Do not limit protein intake acutely
8. TIPS reduction in certain patients with recurrent HE
9. Transplant referral as needed
10. Consider other causes if patient does not improve within 24-48hrs.
Med Clin North Am. 2014 Jan;98(1):119-52. doi: 10.1016/j.mcna.2013.09.006. Epub 2013 Oct 30.
Management of End-stage Liver Disease.
Category: Visual Diagnosis
Posted: 12/16/2013 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
46 year-old female found unresponsive at a party. EMS transports the patient in cardiac arrest. A parasternal-long axis view of the heart is obtained during the pulse check. What's the diagnosis?
Hemopericardium
The heterogeneous appearance of the pericardial fluid indicates that is likely a complex pericardial effusion; the fluid could be blood, pus, or a malignant effusion.
Differential diagnosis of hemopericardium includes:
Based on this initial ECHO, a pericardiocentesis was performed and blood was aspirated.
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Orthopedics
Keywords: Osteoarthritis, treatment (PubMed Search)
Posted: 12/14/2013 by Brian Corwell, MD
(Updated: 2/3/2026)
Click here to contact Brian Corwell, MD
Treating knee osteoarthritis - from the American College of Rheumatology
Exercise whether it be aquatic, aerobic (land -based) or resistance can decrease pain and improve functional capacity. Exercise should be performed 3 to 5 times a week. Effects are usually noted after 3 to 6 months.
Weight loss of 5% or greater body weight is associated with a small improvement in pain and physical function. The main benefit of weight loss has more to do to effects on co-morbid conditions.
Walking aids: A single crutch or cane should be held on the side contralateral to the affected knee and should be advanced with the affected limb when walking to reduce the load on the affected joint.
Cane sizing: The distance from the floor to the patient's greater trochanter (brings the elbow to 15º to 20º of flexion.
Chronic OA Management, Marc C. Hochberg. Volume 3 December 2013
Category: Pediatrics
Posted: 12/13/2013 by Rose Chasm, MD
(Updated: 2/3/2026)
Click here to contact Rose Chasm, MD
Wang CJ, et al. Quality-of-care indicators for children with sickle cell disease. Pediatrics. 2011;128:484.
Berini JC, et al. Fatal hemolysis induced by Ceftriaxone in a child with sickle cell anemia. 1995;126:813.
