Category: Pediatrics
Keywords: laceration, suture, absorbable (PubMed Search)
Posted: 8/17/2013 by Jenny Guyther, MD
(Updated: 2/3/2026)
Click here to contact Jenny Guyther, MD
A facial laceration on a child can present a unique challenge which is not limited to the initial visit. The traditional teaching has been to use nonabsorbable sutures and have the patient return in 5 days for removal. A recent study compared the cosmetic outcome of linear facial lacerations 1 to 5 cm that were closed with either Ethicon fast absorbing surgical gut or monocryl nonabsorbable sutures. Patients were randomized and returned to the ED in 4-7 days and 3-4 months. Scars were assessed by caregivers and blinded physicians. Results showed that caregivers preferred absorbable sutures. Visual analog scores as given by caregivers were not statistically different between the 2 groups at the 3 month mark. The blinded physicians did give better cosmetic outcome scores to the absorbable suture group which differs from previous studies that had shown equivocal results. Of note, all absorbable sutures were no longer visible after 14 days.
Bottom line: Try absorbable sutures the next time you are suturing a child and the parents may be happier and you will not have to try and take out your sutures from a squirming, screaming child.
Luck et al. Comparison of Cosmetic Outcomes of Absorbable Versus Nonabsorbable Sutures in Pediatric Facial Lacerations. Pediatric Emergency Care. Vol 29. No 6. 2013.
Category: Toxicology
Keywords: sulfonamide, antibiotic, cross-reactivity (PubMed Search)
Posted: 8/15/2013 by Bryan Hayes, PharmD
(Updated: 1/29/2014)
Click here to contact Bryan Hayes, PharmD
There is minimal evidence of cross-reactivity between sulfonamide antibiotics and non-antibiotics [1-4]. Despite this, the U.S. FDA-approved product information for many non-antibiotic sulfonamide drugs contains warnings concerning possible cross-reactions.
Key Findings from a New Review Article [5]:
Bottom line: You can feel safe prescribing furosemide, glyburide, and hydrochlorothiazide to your patient with an allergy to sulfamethoxazole/trimethoprim.
Other blog reference on this topic: http://lifeinthefastlane.com/2011/04/sulfa-drug-discombobulation/
Follow me on Twitter (@PharmERToxGuy)
Category: International EM
Keywords: XDR, tuberculosis, international, Eastern Europe, Russia (PubMed Search)
Posted: 8/14/2013 by Andrea Tenner, MD
Click here to contact Andrea Tenner, MD
General Information:
XDR TB is “extensively drug resistant tuberculosis”—resistant to isoniazid, rifampin, any fluoroquinolone, and at least one of the 3 injectable 2nd line drugs
Clinical Presentation:
- Identical to regular TB (weight loss, fevers, night sweats, cough, hemoptysis)
- Suspect in patients who are failing usual treatment
-Exposure in Eastern Europe or Russia (highest prevalence, although 84 countries have had documented XDR, including the US.)
Diagnosis:
- Plating on agar or liquid media for drug susceptibility testing
Treatment:
- Should be guided by susceptibility testing
- Isolate the patient!
Bottom Line:
XDR TB is increasing in prevalence, have a high index of suspicion in patients with persistent symptoms who are receiving treatment and isolate if any concerns.
University of Maryland Section of Global Emergency Health
Author: Andi Tenner, MD, MPH
Abubakar I, Zignol M, Falzon D, et al. Drug-resistant tuberculosis: time for visionary political leadership. The Lancet. 2013. Accessed online at http://dx.doi.org/10.1016/S1473-3099(13)70030-6 on August 14, 2013.
http://www.cdc.gov/tb/publications/factsheets/drtb/xdrtb.htm
Category: Critical Care
Posted: 8/14/2013 by Mike Winters, MBA, MD
Click here to contact Mike Winters, MBA, MD
Clostridium Difficile Associated Diarrhea and The Elderly Patient
Heppner HJ, et al. Infections in the Elderly. Crit Care Clin 2013; 29:757-774.
Category: Visual Diagnosis
Posted: 8/10/2013 by Haney Mallemat, MD
(Updated: 8/12/2013)
Click here to contact Haney Mallemat, MD
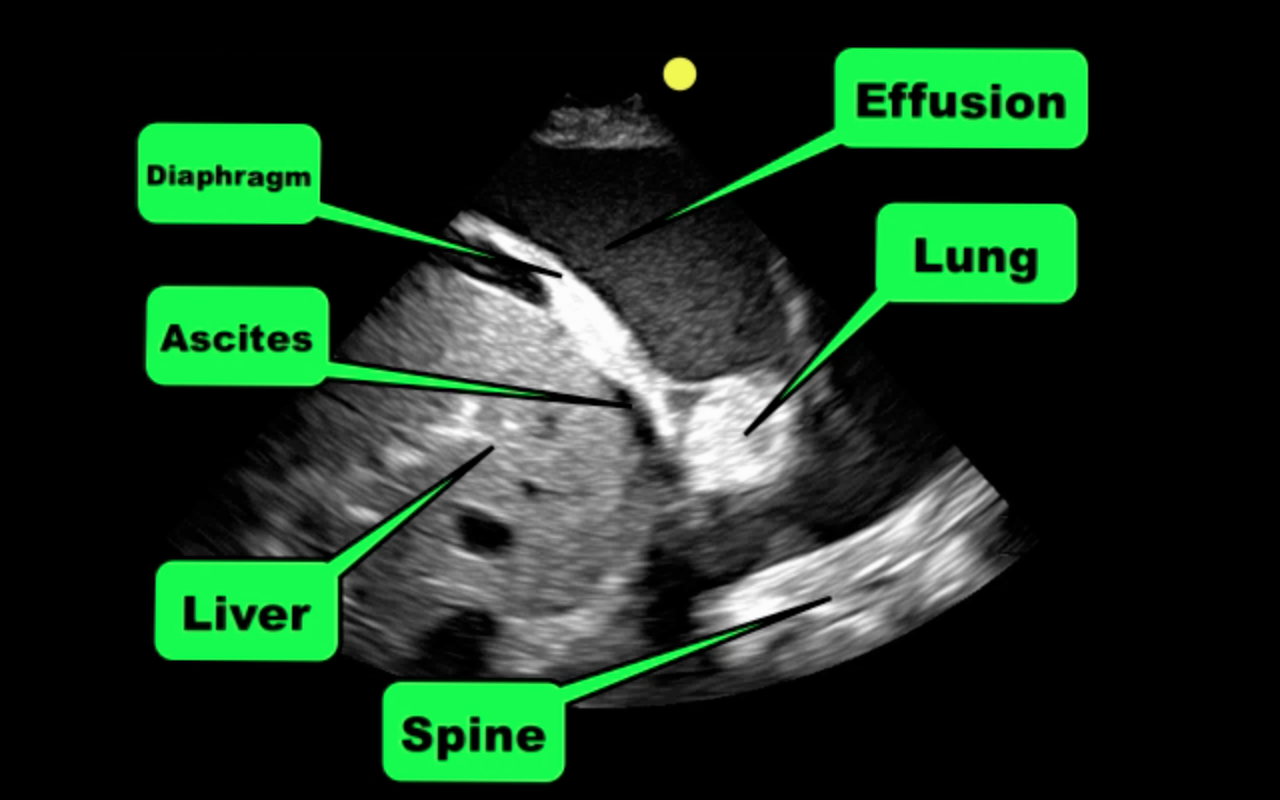
Patient with liver disease presents with dyspnea, fever, and the following ultrasound? What's the diagnosis? (Hint: there are two)?
Answer: Complex pleural effusion and ascites
The take away point from this case is to always place the diaphragm in the center of the screen in order to distinguish peritoneal from thoracic fluid. Fluid in both compartments will sometimes be present (as in this case).
Complex pleural effusions
Follow me on Twitter (@criticalcarenow) or Google+(+criticalcarenow)
Category: Orthopedics
Keywords: Trigger finger, flexor tendon, locked finger (PubMed Search)
Posted: 8/8/2013 by Brian Corwell, MD
(Updated: 2/3/2026)
Click here to contact Brian Corwell, MD
The flexor tendons of the finger may become thickened and narrowed from chronic inflammation and irritation.
- Causes limitation in range of motion and snapping or locking during flexion
- Can involve any digit but usually the ring and the long finger
CC: pain, "catching" May awake to finger being "locked" with spontaneous resolution during the day
Stenosis occurs at the MCP level
PE: Distal flexor crease tender to palpation and may have a painful nodule
Full finger flexion is sometimes not possible
Tx: NSAIDs and steroid injection in tendon sheath. If this fails - surgical release.
Category: Pediatrics
Posted: 8/10/2013 by Rose Chasm, MD
(Updated: 2/3/2026)
Click here to contact Rose Chasm, MD
Clinically important traumatic brain injuries are rare in children. The PECARN study provides decision rules for when to avoid unnecessarily obtaining a CT for children who have suffered head trauma.
For children < 2 years old: <0.02% risk of clinically important TBI
For children > 2 years old: <0.05% risk of clinically important TBI
Kuppermann N, et al. Pediatric Emergency Care Applied Research Network. Identification of childrent at very low risk of clinically-important brain injuries after head trauma: a prospective cohort study. Lancet 2009 Oct 3;374(9696):1160-70.
Category: Toxicology
Keywords: naloxone, nebulized, opioid (PubMed Search)
Posted: 7/30/2013 by Bryan Hayes, PharmD
(Updated: 8/8/2013)
Click here to contact Bryan Hayes, PharmD
Naloxone can be administered via pretty much any route. One that has gained popularity in the past several years is nebulized naloxone. Although anecdotal reports tout the benefits of nebulized naloxone, what does the literature say?
Bottom Line: Many of the studied patients may not have needed naloxone in the first place (initial respiratory rate 13-14), with a few developing withdrawal symptoms. Nebulized naloxone may have a role in the not-too-sick opioid overdose in whom you want to prove your diagnosis and wake the patient up enough to obtain a history. It is not a therapy for the apneic opioid overdose.
1. Mycyk MB, et al. Nebulized naloxone gently and effectively reverses methadone intoxication. J Emerg Med 2003;24(2):185-7. [PMID 12609650]
2. Weber JM, et al. Can nebulized naloxone be used safely and effectively by emergency medical services for suspected opioid overdose? Prehosp Emerg Care 2013;16(2):289-92. [PMID 22191727]
3. Baumann BM, et al. Use and efficacy of nebulized naloxone in patients with suspectd opioid intoxication. Am J Emerg Med 2013;31(3):585-8. [PMID 23347721]
Follow me on Twitter (@PharmERToxGuy)
Category: International EM
Posted: 8/8/2013 by Walid Hammad, MD, MBChB
Click here to contact Walid Hammad, MD, MBChB
General Information:
·You must know the diagnosis to deliver effective and high quality care to patients; likewise for health systems to be effective, it is necessary to understand what the global burden of disease is.
·In 1991, the World Bank and World Health Organization launched the Global Burden of Disease Study which as of 2010 evaluates 291 disease and injuries as well as 1160 sequelae of these causes.
·In order to compare the burden of one disease with that of another, you must consider death and life expectancy of persons affected by the disease as well as disability imposed by the condition.
·The combined composite summary metric is termed disability adjusted life years (DALYs).
·There have been three major worldwide studies to date (1990, 2005, 2010) attempting to quantify the burden of disease yet no study to date has ever attempted to quantify the burden of disease requiring emergent intervention.
Bottom Line:
DALYs are a useful tool for quantifying the burden of disease and provides essential input into health policy dialogues to identifies conditions and risk factors that may be relatively neglected and others for which progress is not what was expected. To date, there has been no rigorous scientific effort to quantify the burden of disease worldwide that requires emergent intervention to avoid death and disability.
University of Maryland Section of Global Emergency Health
Author: Emilie J. B. Calvello, MD, MPH
Christopher J.L. Murray, M.D., D.Phil., and Alan D. Lopez, Ph.D. Measuring the Global Burden of Disease. N Engl J Med 2013; 369:448-45
Category: Critical Care
Keywords: Neurocritical care, Ventilator Strategies, ARDS, Intracranial hemorrhage (PubMed Search)
Posted: 8/5/2013 by John Greenwood, MD
(Updated: 8/6/2013)
Click here to contact John Greenwood, MD
Bad brain, good lungs.... Right?
A recent retrospective study reviewed the incidence of acute respiratory distress syndrome (ARDS) in patients presenting with spontaneous intracerebral hemorrhage over a 10-year period. After reviewing 1,665 patients, the authors found that:
It's of particular importance to note that high tidal volume ventilation (>8cc/kg) was the single greatest modifiable factor for the development of ARDS.
Bottom line: Try and use lung-protective ventilation strategies (6-8cc/kg ideal body weight) and avoid excessive volume resuscitation in your critically-ill patients whenever possible. Even in cases of isolated intracerebral hemorrhage - where the patient's lungs may appear to be completely normal - traditional tidal volume settings may be harmful.
Category: Visual Diagnosis
Posted: 8/5/2013 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
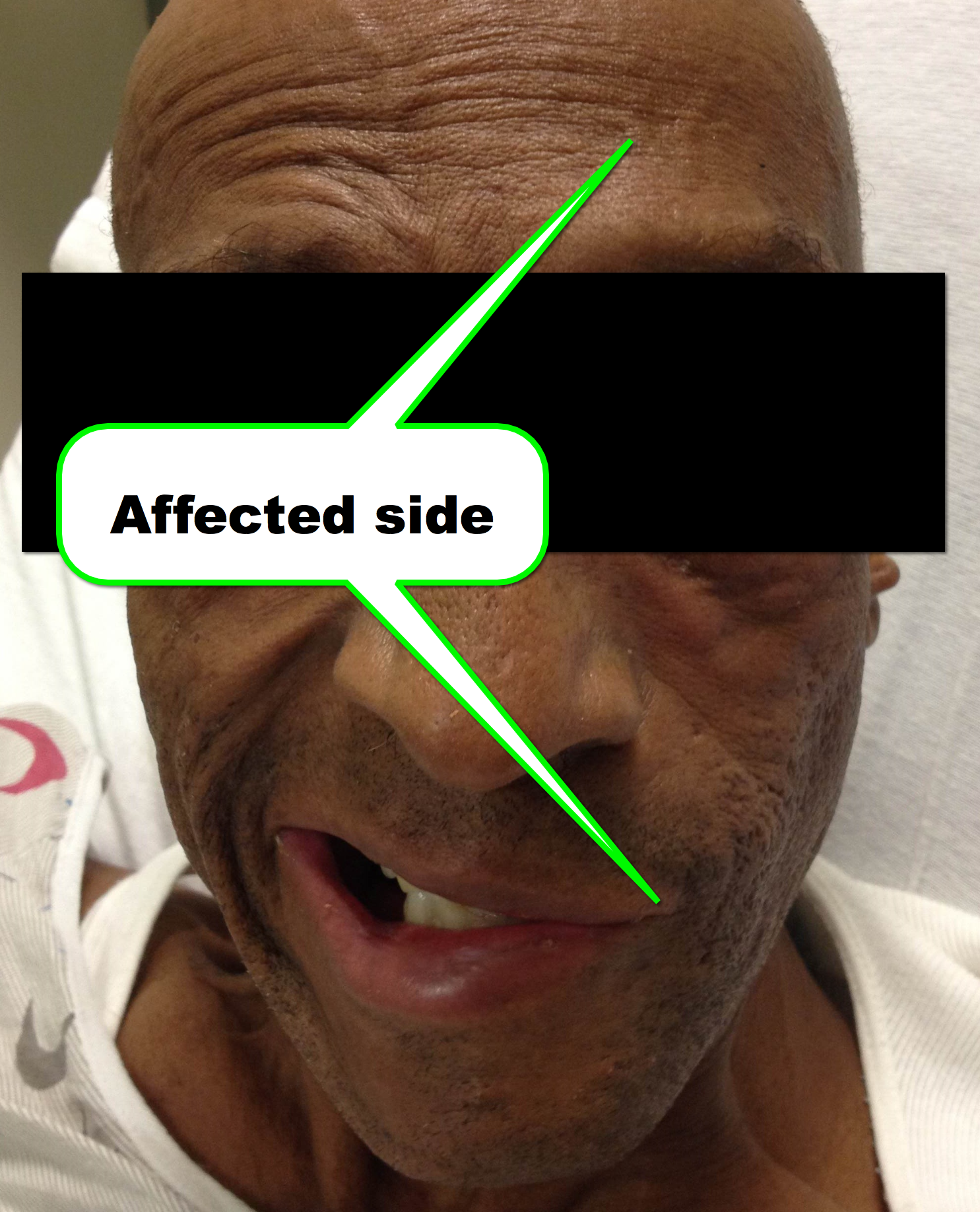
45 year-old man presents after he cannot close his left eye. In the photo below, he is trying to simultaneously raise his forehead and smile. Of note, he was also started on doxycycline recently for Lyme disease. What two medications should he receive?

Bell Palsy
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Cardiology
Posted: 8/5/2013 by Semhar Tewelde, MD
Click here to contact Semhar Tewelde, MD
Category: Pharmacology & Therapeutics
Keywords: fluid, saline, chloride (PubMed Search)
Posted: 7/22/2013 by Bryan Hayes, PharmD
(Updated: 8/2/2013)
Click here to contact Bryan Hayes, PharmD
A recent review identified 5 key points to consider when prescribing fluids.
Raghunathan K, et al. Fluids are drugs: type, dose and toxicity. Curr Opin Crit Care 2013;19(4):290-8. [PMID 23817025]
Follow me on Twitter (@PharmERToxGuy)
Category: Airway Management
Keywords: ALTE, life threatening, child abuse, GERD (PubMed Search)
Posted: 8/2/2013 by Joey Scollan, DO
Click here to contact Joey Scollan, DO
Definition: An episode that is characterized by some combination of apnea, color change, change in muscle tone, choking, gagging, or a fear in the observer that the infant has died.
DDx: VAST!
- GERD is by far the most common underlying etiology
- Do NOT forget about child abuse
Workup: Dependent on your Hx/PE (Take into account the child’s age (<30 days or h/o prematurity), existence of prior ALTE episodes, general appearance, etc.)
One study showed the concordance of initial working to discharge diagnosis of GERD was 96%, and non-concordant diagnoses evolved within 24 hours
Dispo: The easy part! ADMIT!
Even well-appearing children with a “benign” diagnosis like GERD have been shown to benefit from admission. And there is a high likelihood that ALTE’s from a serious cause are likely to recur within 24hours.
A recent study looked at 176 infants who presented to the ED with an ALTE over a 5 year period. Essentially all were admitted.
Conclusion: The risk of subsequent mortality in infants presenting ALTE is substantial, and we should consider routine admission for all of these patients.
Doshi A, Bernard-Stover L, Kuelbs C, Castillo E, Stucky E. Apparent life-threatening event admissions and gastroesophageal reflux disease: The value of hospitalization. Pediatr Emerg Care, January 2012. 28(1): p. 17-21.
Shruti Kant, Jay D. Fisher, David G. Nelson, Shehma Khan. Mortality after discharge in clinically stable infants admitted with a first-time apparent life-threatening event. AJEM, April 2013. 31(4): p 17-21. 730-733 (DOI: 10.1016/j.ajem.2013.01.002)
Zuckerbraun NS, Zomorrodi A, Pitetti RD. Occurrence of serious bacterial infection in infants aged 60 days or younger with an apparent life-threatening event. Pediatr Emerg Care, January 2009. 25(1): p. 19-25.
Category: Toxicology
Keywords: bicarbonate, acetate, TCA, salicylate, poisoning, alkalinization (PubMed Search)
Posted: 8/1/2013 by Ellen Lemkin, MD, PharmD
Click here to contact Ellen Lemkin, MD, PharmD
A recent article was published in the Journal of Medical Toxicology reviewing the use of sodium acetate for treatment of overdoses and poisonings.
Acetate is metabolized to bicarbonate, causing a net increase in cations; this increased strong anion difference leads to alkalemia.
It has been used to treat acidosis in uremia, diarrhea, and in trauma patients.
Although no studies have been conducted using sodium acetate as an antidote, if bicarbonate is unavailable this is a viable option for management of salicylate overdose, and for qrs widening or arrhythmias due to overdoses.
Sodium acetate, if given rapidly (in animals and hemodialysis patients), causes myocardial depression, hypotension, and hypopnea.
The bolus dose should be given as 1-2 mEq/L given over 15-20 minutes. For the maintenance infusion, dilute 150 mEq diluted to 1 L in dextrose 5%, infuse at 2X the maintenance rate.
It must be diluted in dextrose 5% and NOT normal saline.
Neavyn MJ, Boyer EW, Bird SB, Babu KM. Sodium Acetate as a Replacement for Sodium Bicarbonate in Medical Toxicology: a Review. Published online 30 April 2013. J. Med. Toxicol.
Category: International EM
Keywords: cyclospora, outbreak, international, tropical, infectious disease (PubMed Search)
Posted: 7/31/2013 by Andrea Tenner, MD
Click here to contact Andrea Tenner, MD
General Information:
As of July 30th, 2013, there have been 378 cases of Cyclospora infection from multiple states in the US. Cyclospora is most common in tropical and sub-tropical regions, and is spread via fecal-oral route. While the cause of the most recent outbreak is unknown, outbreaks in the US are generally foodborne.
Clinical Presentation:
- Symptoms usually begin 7 days after exposure
- Watery diarrhea, cramping, bloating, nausea, fatigue, increased gas, vomiting, low grade temperature
- Can persist several weeks to > 1 month
Diagnosis:
- Concentrated Stool Ova and Parasites— viewed under modified acid fast or fluorescence microscopy (labs can submit photos to the CDC for “telediagnosis”)
Treatment:
- TMP-SMX DS one tab po bid x7-10 days
- No effective alternate for failed treatment or sulfa allergy
- Most will recover without treatment but S/S can persist for weeks to months
Bottom Line:
Consider Cyclospora as a cause of prolonged diarrheal illness, treat with TMP-SMX.
University of Maryland Section of Global Emergency Health
Author: Andi Tenner, MD, MPH
www. cdc. gov/parasites/cyclosporiasis/outbreaks/investigations-2013.html
www.cdc.gov/parasites/cyclosporiasis
Category: Critical Care
Posted: 7/30/2013 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
Elderly patient who originally presented for severe pancreatitis now intubated for worsening hypoxemia. CXR is shown below, what's the diagnosis?

Acute Respiratory Distress Syndrome (ARDS)
Acute Respiratory Distress Syndrome (ARDS) is defined as hypoxemia secondary to increased pulmonary capillary permeability and non-hydrostatic (i.e., non-cardiogenic) leakage of fluid into the interstitial lung tissue and alveoli. Lung radiographs diffuse and symmetric infiltrates (see below)
ARDS may occur secondary to a primary (or pulmonary) insult (e.g., aspiration, pneumonia) or secondary (or systemic) insult (e.g., pancreatitis, trauma, etc.)
The newest classification system for ARDS no longer includes the previously known category of acute lung injury; there are three categories of ARDS determined by the PaO2 (on ABG) divided by administered FiO2 (as a fraction of 100%):
A number of interventions have been demonstrated to improve outcomes for patients with ARDS:
Follow me on Twitter (@criticalcarenow) or on Google+ (+criticalcarenow)
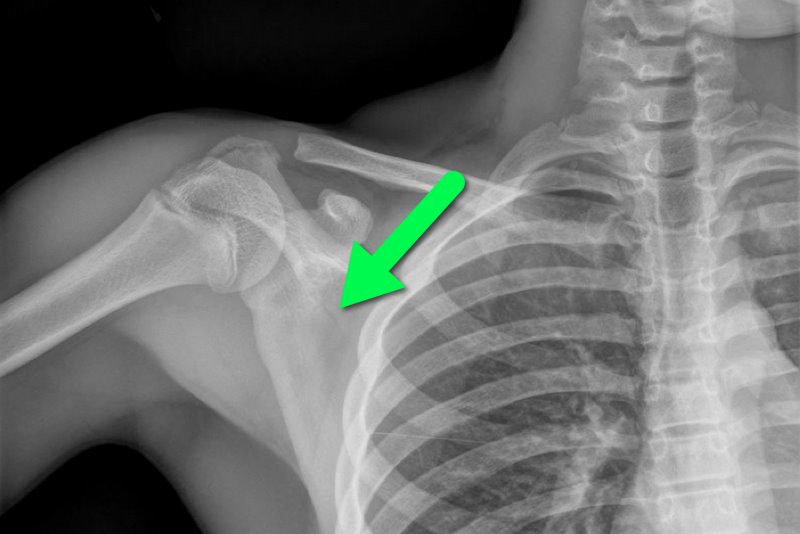
Category: Visual Diagnosis
Posted: 7/29/2013 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
13 year-old female fell on right shoulder while catching a rebound during a basketball game. The patient is holding her arm in adduction and has exquisite scapular tenderness on exam. What’s the next step in management? …oh, and what’s the diagnosis?
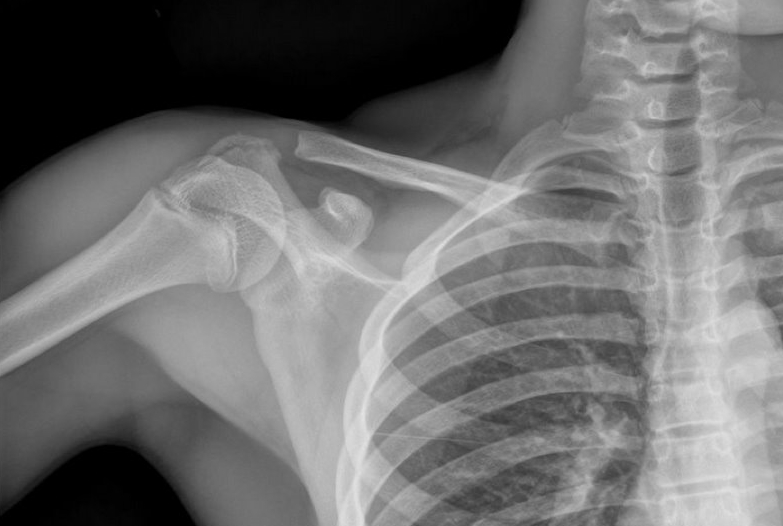
Answer: Non-displaced scapular fracture
Treatment:
Bonus Pearls: #foam4yrdome
This installment of #foam4yrdome will focus on freeemergencytalks.net which is quite possibly the best Critical Care and Emergency Medicine FREE lecture website.
The website was founded and is maintained by Professor Joe Lex (@joelex5); the website hosts hundreds of free talks.
Check out talks from all the major conferences featuring the best speakers in Emergency and Critical care medicine today.
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Cardiology
Posted: 7/29/2013 by Semhar Tewelde, MD
(Updated: 2/3/2026)
Click here to contact Semhar Tewelde, MD
Tight glycemic control (HbA1C<7%) has previously been recommended in CAD based on data from the United Kingdom Prospective Diabetes Study (UKPDS)
A recent study (JACC) evaluated the relationship between glycemic control, cardiovascular disease (CVD) risk, and all-cause mortality
Patients with a mean HbA1C 7-7.4% were compared to those with mean HbA1C <6%; tight glycemic control had a 68% increased risk of CVD hospitalization
Lenient HbA1C>8.5% also had significantly higher risk
CVD risk and all-cause mortality is greater with both aggressive and lax glycemic control and the optimal reference range may lie between 7-7.4%
| Nichols G, Joshua-Gotlib S, Parasuraman. Glycemic Control and Risk of Cardiovascular Disease Hospitalization and All-Cause Mortality. JACC. 62: 2; 121-127. |
Category: Orthopedics
Keywords: Hand nodules, contactures (PubMed Search)
Posted: 7/28/2013 by Brian Corwell, MD
(Updated: 2/3/2026)
Click here to contact Brian Corwell, MD
Dupuytren disease is a nodular thickening and resultant contraction of the palmer fascia.
Increased in those of Northern European dissent.
One or more painful nodules located near the distal palmer crease.
Over time may result in flexion at the MCP joint.
Most commonly affects the ring finger.
Sensation is normal.
Over time affects ADLs
Tx: night splints and surgery
