Category: Pediatrics
Keywords: sedation, pain management (PubMed Search)
Posted: 7/3/2013 by Mimi Lu, MD
(Updated: 7/26/2013)
Click here to contact Mimi Lu, MD
Cringing at the thought of sewing up another screaming 2 year old?
Consider intranasal fentanyl.
Who: Young, otherwise healthy pediatric patients undergoing minor procedures (laceration repair, fracture reduction/splinting, etc...)
What: Fentanyl (2mcg/kg)
When: 5 minutes pre-procedure
Where: Intranasal
Why: More effective than PO, less invasive than IV while being equally efficacious.
How: Use an atomizer, splitting the dose between each nostril.
Category: International EM
Posted: 7/24/2013 by Walid Hammad, MD, MBChB
Click here to contact Walid Hammad, MD, MBChB
General Information:
· Caused by the ameboflagellate Naegleria Fowleri
· Case fatality rate is estimated at 98%
· Commonly found in warm freshwater environments such as hot springs, lakes, natural mineral water, especially during hot summer months
· Incubation period 2-15 days
Relevance to the EM Physician:
· Clinical presentation: resembling bacterial meningitis/encephalitis
· Final diagnostic confirmation is not achieved until trophozoites are isolated and identified from CSF or brain tissue
· Treatment: Amphotericin B
Bottom Line:
· History of travel to tropical areas or exposure to warm or under-chlorinated water during summer time should raise the suspicion for Naegleria Fowleri. The amoeba is not sensitive to the standard meningitis/encephalitis therapy and amphotericin B must be added to the treatment regimen.
University of Maryland Section of Global Emergency Health
Su MY, Lee MS, Shyu LY, Lin WC, Hsiao PC, Wang CP, Ji DD, Chen KM, Lai SC. A fatal case of Naegleria fowleri meningoencephalitis in Taiwan. Korean J Parasitol. 2013 Apr
Naegleria fowleri, Kelly Fero , ParaSite, February 2010 retrieved from http://www.stanford.edu/group/parasites/ParaSites2010/Katherine_Fero/FeroNaegleriafowleri.htm
Category: Critical Care
Posted: 7/23/2013 by Mike Winters, MBA, MD
(Updated: 2/3/2026)
Click here to contact Mike Winters, MBA, MD
HIV, ART, and the ICU
Tan DHS, Walmsley SL. Management of persons infected with human immunodeficiency virus requiring admission to the intensive care unit. Crit Care Clin 2013; 29:603-20.
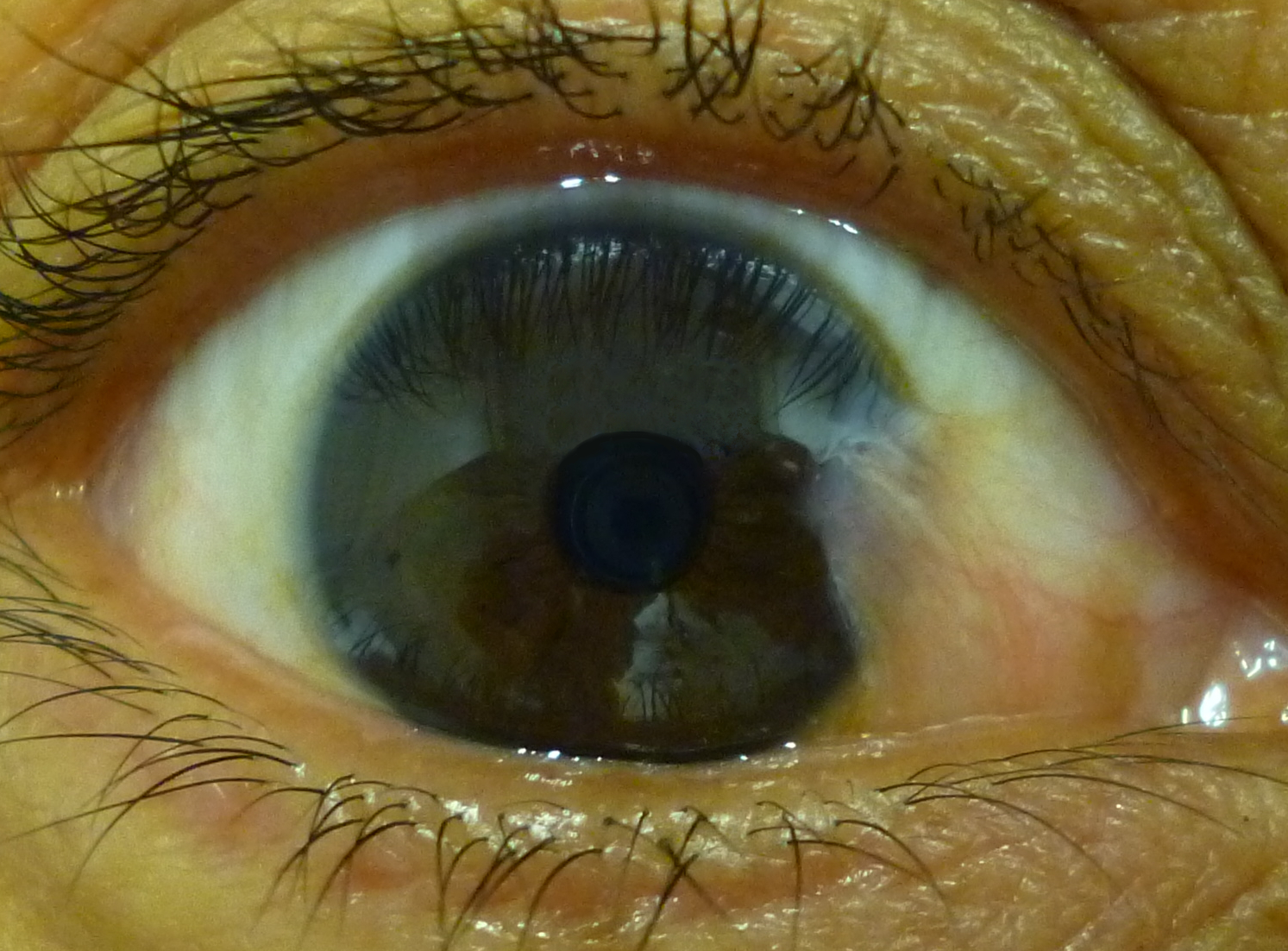
Category: Visual Diagnosis
Posted: 7/22/2013 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
A 3 year-old boy was attacked by a dog and sustained the injury below. Name one injury that should be strongly considered (Hint: there are several)

Important injuries to consider (image below):
This patient had only a corneal abrasion on fluorescein exam.

Bonus Pearl: #Foam4yrDome
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Cardiology
Posted: 7/21/2013 by Semhar Tewelde, MD
Click here to contact Semhar Tewelde, MD
Westfall M, Krantz S, Mullin C, Kaufman C. Mechanical versus manual chest compressions in out-of-hospital cardiac arrest. Crit Care Med 2013 Jul; 41(7):1782-9
Category: Endocrine
Keywords: Hypothyroidism, treatment (PubMed Search)
Posted: 7/20/2013 by Michael Bond, MD
(Updated: 2/3/2026)
Click here to contact Michael Bond, MD
Treatment of Severe Hypothyroidism
We do not see patient's with severe hypothyroidism often, but it is important that they be treated aggressively. Some treatment pearls are
Category: Pediatrics
Keywords: lactate, sepsis, pediatric (PubMed Search)
Posted: 7/19/2013 by Jenny Guyther, MD
Click here to contact Jenny Guyther, MD
Lactate is commonly used in the adult ED when evaluating septic patients, but there is a lack of literature validating its use in the pediatric ED. Pediatric studies have suggested that in the ICU population, elevated lactate is a predictor of mortality and may be the earliest marker of death.
A retrospective chart review over a 1 year period showed that one elevated serum lactate correlated with increased pulse, respiratory rate, white blood cell count and platelets. Serum lactate had a negative correlation with BUN, serum bicarbinate and age. Elevated lactate levels were higher for admitted patients. However, the mean serum lacate level was not statistically different between those diagnosed with sepsis and those that were not.
The study included 289 patients less then 18 years who had both blood cultures and lactate drawn. This community hospital had a sepsis protocol in place that automatically ordered a lactate with blood cultures. Only previously healthy children were included.
The study is limited by its small sample size and overall low lactate levels. Despite having a protocol in place, only 39% of patients who had blood cultures drawn had lactate levels available for analysis. The mean serum lacate in this study was 2.04 mM indicating that the study population may not have been sick enough to determine mortality implications. There were no serial measurements.
Bottom line: Consider measuring serum lacate in your pediatric patient with suspected sepsis. Pediatric ICU literature does suggest that an serum lactate as low as 3mM is associated with an increased mortality in the ICU.
Reed et al. Serum Lactate as a Screening Tool and Predictor of Outcome in Pediatric Patients Presenting to the Emergency Department With Suspected Infection. Pediatric Emergency Care. 2013; Vol 29: 787-791.
Category: Toxicology
Keywords: lsd, alpha-methyltryptamine, AMT (PubMed Search)
Posted: 7/18/2013 by Fermin Barrueto
(Updated: 2/3/2026)
Click here to contact Fermin Barrueto
The internet has become a wealth of information and some books have now gained internet noteriety. A chemist and author of the book - TIKHAL: Tryptamines I Have Known and Loved is an excellent example.
Tryptamines include drugs like LSD and alpha-methyltryptamine (AMT). Vivid visual hallucinations and serotonin agonism, these drugs were glamorized by this author. He would synthesize a tryptamine and then "taste it". Take a look at the link below where he first describes the biochemical synthesis he performed then describes his dose response effect when he tried the drug.
If you run into a drug or slang term in the ED you are not familiar with, the website www.erowid.org will likely have the translation.
http://www.erowid.org/library/books_online/tihkal/tihkal48.shtml
Category: Critical Care
Posted: 7/16/2013 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
COPD treatment guidelines (e.g., GOLD) recommend 10-14 days of steroid therapy following a COPD exacerbation to prevent recurrences; the supporting data is weak.
A recent noninferiority trial (here) compared patients with a severe COPD exacerbation who received either a 5-day course (n=156) or 14-day course (n=155) of prednisone 40mg.
The results were:
What you need to know:
Bottom-line: 5 days of prednisone may be as effective as 14-days for COPD exacerbations.
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Visual Diagnosis
Posted: 7/15/2013 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
46 year-old female presents with a headache. The following is seen on visual inspection of the eye. What's the diagnosis?
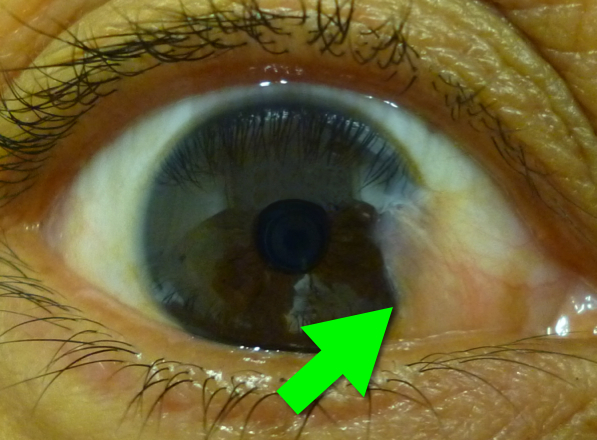
Pterygium
Six-word Summary: Cornea, benign, UV, supportive, surgery, and sunglasses
Bonus Pearl
As a new academic year begins, I will be sharing some amazing free educational online resources/links. These free materials are known as Free Open Access Meducation (or FOAMed) and for those familiar with FOAMed this is an emerging educational revolution. If you don't know what FOAMed is, read about it here and then read this. Updates will happen every Monday and will be known as #FOAM4yourDome
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Cardiology
Posted: 7/14/2013 by Semhar Tewelde, MD
Click here to contact Semhar Tewelde, MD
Radiation therapy is frequently utilized in the management of numerous thoracic malignancies
Cardiovascular disease is now the leading cause of nonmalignancy death in radiation-treated cancer survivors
The spectrum of radiation-induced cardiac disease is broad
The relative risk of CAD, CHF, pericardial/valvular disease, and conduction abnormalities is particularly increased
Early identification of potential cardiac complications w/cardiac MR and echocardiography provides an opportunity for regular assessment and potentially improved long term mortality
Jaworksi C, Mariani J, et al. Cardiac Complication of Thoracic Irradiation. JACC Vol 61, No 23, 2013.
Category: Orthopedics
Keywords: ulnar nerve, entrapment (PubMed Search)
Posted: 7/13/2013 by Brian Corwell, MD
(Updated: 2/3/2026)
Click here to contact Brian Corwell, MD
Tests for distal ulnar nerve entrapment
Ask patient to hold a piece of paper between the thumb and the index finger
Normally this is a fairly simple task.
With an unlar nerve palsy, the patient will substitute with the FPL (flexor pollicis longus - median nerve innervation). This causes flexion of the thumb in order to maintain the grip since the adductor pollicis cannot be used. This causes thumb flexion rather than extension.
http://www.mims.com/resources/drugs/common/CP0042.gif
http://www.youtube.com/watch?v=yJTIhm1VfSI
Category: Pediatrics
Posted: 7/12/2013 by Rose Chasm, MD
(Updated: 2/3/2026)
Click here to contact Rose Chasm, MD
Risk stratisfication score introducted by Maden Samuel in 2002.
The Pediatric Appendicitis Score had a sensitivity of 1, speciificity of 0.92, positive predictive value of 0.96, and negative predictive value of 0.99
Signs:
Symptoms:
Laboratory Values:
Scores of 4 or less are least likely to have acute appendicitis, while scores of 8 or more are most likely.
Pediatric Appendicits Score. Samuel, M. J Pedia Surg.37:877-888. 2002.
Category: Toxicology
Keywords: salicylate, aspirin, toxicity, sodium bicarbonate (PubMed Search)
Posted: 7/10/2013 by Bryan Hayes, PharmD
(Updated: 7/11/2013)
Click here to contact Bryan Hayes, PharmD
In June 2013 the American College of Medical Toxicology (ACMT) released a Guidance Document on the Management Priorities in Salicylate Toxicity. Here are some key highlights:
The full document can be accessed here.
The Poison Review blog by Dr. Leon Gussow discusses the guidance document here.
Follow me on Twitter (@PharmERToxGuy)
Category: Visual Diagnosis
Posted: 7/8/2013 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
3 year-old male develops rash 5 days after starting amoxicillin for acute otitis media. What's the diagnosis?

Erythema Multiforme
Erythema multiforme (EM) is a pruritic, erythematous, and blanchable maculopapular rash; it is serpiginous or targetoid in shape, with central clearing or pallor.
EM is generally symmetric, appearing on hands, feet, groin, and extensor aspects of legs and forearms.
It is classically associated with upper respiratory infections, medications, connective tissue diseases, and malignancies.
Treatment includes:
Habif, et al, Skin Disease, 3rd Ed. 2011
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Cardiology
Posted: 7/7/2013 by Semhar Tewelde, MD
(Updated: 2/3/2026)
Click here to contact Semhar Tewelde, MD
Barthwal SP, Agarwal R, Sarkari NB et al. Diagnostic Significance of TI < T III and TVI > TV6 signs in ischemic heart disease . J Assoc Phys India 1993;41:26-7
Category: Pharmacology & Therapeutics
Keywords: pain, hydromorphone (PubMed Search)
Posted: 7/3/2013 by Bryan Hayes, PharmD
(Updated: 7/6/2013)
Click here to contact Bryan Hayes, PharmD
A recent, randomized study evaluated two approaches for treating acute pain in an inner-city ED.
Application to clinical practice: For most patients with acute, severe pain in the ED, start with hydromorphone 1 mg. It may be all the patient needs and can potentially avoid giving them extra opioid they don't need.
Chang AK, et al. Randomized clinical trial of the 2 mg hydromorphone bolus protocol versus the "1 + 1" hydromorphone titration protocol in treatment of acute, severe pain in the first hour of emergency department presentation. Ann Emerg Med. 2013 May 16. [Epub ahead of print]. PMID 23694801
Follow me on Twitter (@PharmERToxGuy)
Category: Pharmacology & Therapeutics
Keywords: insulin, metformin, sulfonylureas, repaglinide (PubMed Search)
Posted: 7/4/2013 by Ellen Lemkin, MD, PharmD
Click here to contact Ellen Lemkin, MD, PharmD
Diabetes. Pharmacist's Letter March 2013;29(3):13-4.
Category: International EM
Keywords: Hepatits C, Infectious Disease, International, Liver (PubMed Search)
Posted: 7/3/2013 by Andrea Tenner, MD
(Updated: 2/3/2026)
Click here to contact Andrea Tenner, MD
Background:
Infection with the Hepatitis C virus can result in mild to severe liver disease. Morbidity and mortality from Hep C is increasing the US--many of the 2.7-3.9 million persons with Hep C are not aware of their infection.
Pertinent Information:
- Hepatitis C is now curable for many patients
- Current treatment recommendations are a combination of medications (pegylated interferon plus ribavirin plus a protease inhibitor).
- Research in this field is very active--treatment is likely to change in the next 3-5 years.
- Risk reduction strategies to protect the liver (i.e. eliminating alcohol and Hep A and B vaccination) are also recommended.
Critical New Recommendation
As much of the disease burden is in the “Baby Boomers,” the CDC now recommends one time testing of all persons born between 1945 and 1965.
Bottom Line:
While emergency department management is focused on the treatment of acute complications of liver disease, it is also important to have all age appropriate patients follow-up for testing and treatment of Hepatitis C with their primary care provider.
Treatment for Hepatitis C Virus Infection in Adults [Internet]. Editors: Chou R, Hartung D, Rahman B, Wasson N, Cottrell E, Fu R. Rockville (MD): Agency for Healthcare Research and Quality (US); 2012 Nov. Report No.: 12(13)-EHC113-EF. AHRQ Comparative Effectiveness Reviews.
Recommendations for the identification of chronic hepatitis C virus infection among persons born during 1945-1965. Smith BD, Morgan RL, Beckett GA, Falck-Ytter Y, Holtzman D, Teo CG, Jewett A, Baack B, Rein DB, Patel N, Alter M, Yartel A, Ward JW; Centers for Disease Control and Prevention. MMWR Recomm Rep. 2012 Aug 17;61(RR-4):1-32
Category: Critical Care
Posted: 7/2/2013 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
Hydroxyethyl starch (HES) is a colloid used for volume resuscitation in critically-ill patients.
Previous studies (click here) have compared crystalloids to HES during fluid resuscitation and have demonstrated that HES has an increased cost with more adverse effects. Adverse effects may include:
In the United States, the Federal Drug Administration published a warning on June 24th 2013 with respect to the use of HES in critically ill adult patients. Specifically, it warned about the use of HES in patients,
If a decision to use HES is made, the FDA warning advises to:
Bottom line: With an increased cost and evidence of harm compared to crystalloids, it appears the indications for use of HES are rapidly declining.
http://www.fda.gov/BiologicsBloodVaccines/SafetyAvailability/ucm358271.htm
Perner A., et al. Hydroxyethyl Starch 130/0.4 versus Ringer's Acetate in Severe Sepsis. NEJM. 2012 Jun 27.
MyBurgh, J. Hydroxyethyl Starch or Saline for Fluid Resuscitation in Intensive Care. N Engl J Med. 2012 Oct 17.
