Category: Pediatrics
Posted: 4/26/2013 by Mimi Lu, MD
Click here to contact Mimi Lu, MD
An overweight 5 year old male presents with acute onset abdominal pain that localizes to the right lower quadrant. What are some causes of a limited or nondiagnostic ultrasound study in children?
Acute appendicitis is a time sensitive diagnosis. Ultrasound is frequently used as the initial diagnostic imaging in children. There are several reasons why the appendix may not be visualized, including retro-cecal location, normal appendix, perforation, and inflammation around the distal tip. An additional clinical predictor associated with poor or inconclusive ultrasound results in appendicitis is increased BMI (body mass index).
A study examining 263 pediatric patients found when BMI > 85th percentile and clinical probability of appendicitis was <50%, 58% of ultrasounds were nondiagnostic. Children with a BMI <85th percentile and clinical probability of appendicitis was <50%, had nondiagonstic scans 42% of the time. These trends were also mimicked in the patients with a higher clinical probability of appendicitis. In the child with a nondiagnostic ultrasound, options include observation and repeat ultrasound scan or CT scan, both of which have associated risks.
Category: Toxicology
Keywords: Kings College, apap, acetaminophen (PubMed Search)
Posted: 4/25/2013 by Fermin Barrueto
(Updated: 2/3/2026)
Click here to contact Fermin Barrueto
If you are working in a community hospital and have an acetaminophen overdose, one of the criteria to transfer the patient to a tertiary care center is presence of the King's College Criteria.
The below is taken from mdcalc.com - http://www.mdcalc.com/kings-college-criteria-for-acetaminophen-toxicity/
Each one is assigned points and can be prognostic for severe toxicity and need for transplant. The lactate and phosphorus are new ones and have modified the criteria. Phosphorus is utilized to create glycogen. If the liver is injured and trying to heal, your phosphorus will be low (good). If the liver is injured and unable to repair itself the phosphorus will be high (bad). This single test has an excellent prognostic ability.
| Lactate > 3.5 mg/dL (0.39 mmol/L) 4 hrs after early fluid resuscitation? | |
| pH < 7.30 or lactate > 3 mg/dL (0.33 mmol/L) after full fluid resuscitation at 12 hours | |
| INR > 6.5 (PTT > 100s) | |
| Creatinine > 3.4 mg/dL (300 µmol/L) | |
| Grade 3 or 4 Hepatic Encephalopathy? | |
| Phosphorus > 3.75 mg/dL (1.2 mmol/L) at 48 hours |
Category: International EM
Keywords: international, laboratory, lab values, SI, conventional (PubMed Search)
Posted: 4/24/2013 by Andrea Tenner, MD
Click here to contact Andrea Tenner, MD
General Information:
The two main units used by medical laboratories are "conventional (used in the US) and SI (used by most other countries).
Pearls to know:
Relevance to the EM Physician:
These tips will help you convert labs to familiar values when reading medical literature, when working in another country, or when working with international colleagues.
University of Maryland Section of Global Emergency Health
Author: Andi Tenner, MD, MPH
Iverson C, Christiansen S, Flanagin A, et al. AMA Manual of Style: A Guide for Authors and Editors. 10th ed. New York, NY: Oxford University Press; 2007.
Ruschin, H and LoRusso J. Normal Values for Selected Blood and Urine Tests. Wiley. http://www.wiley.com/college/bio/tortora366927/resources/faculty/pdf/appb.pdf
Category: Critical Care
Posted: 4/23/2013 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
Necrotizing fasciitis (NF) is a rapidly progressive bacterial infection of the fascia with secondary necrosis of the subcutaneous tissue. In severe cases, the underlying muscle (i.e., myositis) may be affected.
Risk factors for NF include immunosuppression (e.g., transplant patients), HIV/AIDS, diabetes, etc.
There are three categories of NF:
In the early stage of disease, diagnosis may be difficult; the physical exam sometimes does not reflect the severity of disease. Labs may be non-specific, but CT or MRI is important to diagnose and define the extent of the disease when planning surgical debridement.
Treatment should be aggressive and started as soon as the disease is suspected; this includes:
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Pediatrics
Keywords: antibiotics, wait and see (PubMed Search)
Posted: 4/19/2013 by Mimi Lu, MD
Click here to contact Mimi Lu, MD
2013 AAP AOM Guidelines UPDATE
Category: Toxicology
Keywords: Ricin (PubMed Search)
Posted: 4/18/2013 by Fermin Barrueto
(Updated: 2/3/2026)
Click here to contact Fermin Barrueto
With recent events, a few notes about ricin seems appropriate:
CDC website: http://www.bt.cdc.gov/agent/ricin/
Category: International EM
Posted: 4/17/2013 by Walid Hammad, MD, MBChB
Click here to contact Walid Hammad, MD, MBChB
General Information:
A parasitic infection caused by the tissue-dwelling filarial nematode worm Wuchereria bancrofti; a wide range of mosquitoes transmit the infection. When the worm is mature, it inhabits lymph nodes and produces sheathed microfilarial larvae that circulate in the peripheral blood.
Clinical Presentation:
- Infection with the adult worms produces painless subcutaneous nodules that are usually less than 2 cm in diameter, typically over bony prominences.
- Symptoms depend on where the microfilariae migrate to, and vary accordingly. They include: pruritus, papular dermatitis, dermal atrophy and depigmentation or hyperreactive skin disease (Sowda), keratitis, iritis, chorioretinitis, optic atrophy and eventually blindness, orchitis, hydrocele, chyluria, elephantiasis, pulmonary eosinophilia, cough, wheezing, and splenomegaly.
Diagnosis:
- Peripheral blood smear taken between 11pm and 1am or after provocation using diethylcarbamazine (DEC).
- Filarial antigen test.
- Eosinophilia, and specific antiflarial IgG and IgE antibodies.
Treatment:
- DEC which must be obtained directly from the CDC.
- Alternatively Doxycycline. Both drugs are effective against both macro and micro-filaria.
Bottom Line:
One billion people globally are at risk for infection with filaria. 120 million already have the infection. Suspect the infection in patients that have been to Africa, Asia, especially India, Western pacific, Haiti, the Dominican Republic, Guyana and Brazil.
University of Maryland Section of Global Emergency Health
Author: Walid Hammad, MD
James AG Whitworth. Filariasis. Medicine. 2005;33:61
Category: Critical Care
Posted: 4/16/2013 by Mike Winters, MBA, MD
Click here to contact Mike Winters, MBA, MD
Massive Transfusion Pearls
Elmer J, et al. Massive transfusion in traumatic shock. J Emerg Med 2013; 44:829-838.
Category: Visual Diagnosis
Posted: 4/15/2013 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
35 year-old female presents with fever and hypotension. Bedside ultrasound is performed and is shown here. What's the diagnosis?
Answer: Aortic valve vegetation secondary to infective endocarditis.
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Cardiology
Posted: 4/14/2013 by Semhar Tewelde, MD
(Updated: 2/3/2026)
Click here to contact Semhar Tewelde, MD
Category: Orthopedics
Keywords: MRI, spinal cord compression (PubMed Search)
Posted: 4/13/2013 by Brian Corwell, MD
Click here to contact Brian Corwell, MD
You have a patient with a spinal cord syndrome and you order the MRI. Have you ever had that conversation with radiology where you have to "choose" what part of the spine you want imaged?
The entire spine needs to be imaged!
The reason: False localizing sensory levels.
For example: The patient has a thoracic sensory level that is caused by a cervical lesion.
A study of 324 episodes of malignant spinal cord compression (MSCC) found that clinical signs were very unreliable indicators of the level of compression. Only 53 patients (16%) had a sensory level that was within 3 vertebral levels of the level of compression demonstrated on MRI.
Further, pain (both midline back pain and radicular pain) was also a poor predictor of the level of compression.
Finally, of the 187 patients who had plain radiographs at the level of compression at referral, 60 showed vertebral collapse suggesting cord compression, but only 39 of these predicted the correct level of compression (i.e. only 20% of all radiographs correctly identified the level of compression).
The authors note that frequently only the lumbar spine was XR at the time of clinical presentation (usually at the referring hospital), presumably due to false localizing signs and a low awareness on the part of clinicians that most MSCC occurs in the thoracic spine (68% in this series).
Summers D, et al. Assessment of MSCC using MRI Br J Radiol 2001;74:977-8.
Category: Visual Diagnosis
Posted: 4/8/2013 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
64 year-old female presents with chest pain following an argument with her husband. Her echocardiogram (apical four-chamber view) and ECG are shown. Her initial troponin is 10. What's the diagnosis?
Answer: Takotsubo (a.k.a Stress) cardiomyopathy (TC)
TC is left ventricular dysfunction (hypokinesia, akinesia, or dyskinesia) secondary to catecholamine surge (e.g., physical / emotional stress) causing myocardial stunning; it is not due to acute coronary occlusion. TC disproportionately affects postmenopausal women, occurring in up to 90% of cases.
Patients often present with chest pain or dyspnea; 85% of patients will have an abnormal ECG (e.g., ST elevation or T wave inversions), making diagnosis difficult to differentiate between TC and acute coronary syndrome (ACS). TC has been found to be the diagnosis in 2.5% of patients initially worked up for ACS.
Diagnosis can usually be confirmed with echocardiography but cardiac catheterization (with ventriculogram) is sometimes performed if ACS is strongly suspected. Catheterization demonstrates normal coronary arteries with an abnormal ventriculogram (click for video), typically in mid-to apical portion of the left ventricle.
Treatment is symptomatic and similar to congestive heart failure (e.g., diuretics, beta-blockers, etc.); 95% of patients have full recovery within one month.
Refer to this prior PEARL by Dr. Tewelde for additional information
Reference
T Pilgrima, T Wyss, Takotsubo cardiomyopathy or transient left ventricular apical ballooning syndrome: A systematic review, Int J Card 2008 Mar 14;124(3):283-92
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Cardiology
Posted: 4/7/2013 by Semhar Tewelde, MD
Click here to contact Semhar Tewelde, MD
Weiss P, et al. Pediatric vasculitis. The Pediatric clinics of North America. April 2012:59;2:407-423.
Category: Critical Care
Keywords: Resuscitation, ventricular fibrillation, cardiac arrest, emergency, cardiology (PubMed Search)
Posted: 4/6/2013 by Ben Lawner, MS, DO
(Updated: 2/3/2026)
Click here to contact Ben Lawner, MS, DO
Recent advances in resuscitation science have enabled emergency physicians to identify factors associated with good neurologic and survival outcomes. Cases of persistent ventricular dysrhythmia (VF or VT) present a particular challenge to the critical care provider. The evidence base for interventions in shock refractory ventricular VF mainly consists of case reports and retrospective trials, but such interventions may be worth considering in these difficult resuscitation situations:
1. Double sequential defibrillation
-For shock-refractory VF, 2 sets of pads are placed (anterior/posterior and on the anterior chest wall). Shocks are delivered as "closely as possible."1,2
2. Sympathetic blockade in prolonged VF arrest
-"Eletrical storm," or incessant v-fib, can complicate some arrests in the setting of VF. An esmolol bolus and infusion may be associated with improved survival.3 Left stellate ganglion blockade has been identified as a potential treatment for medication resistant VF.4
3. Don't forget about magnesium!
-May terminate VF due to a prolonged QT interval
4. Invasive strategies
-Though resource intensive, there is limited experience with intra-arrest PCI and extracorporeal membrane oxygenation. Preestablished protocols are key to selecting patients who may benefit from intra-arrest PCI and/or ECMO. 5
5. Utilization of mechanical CPR devices
-Though mechanical CPR devices were not officially endorsed by the AHA/ECC 2010 guidelines, there's little question that mechanical compression devices address the complication of provider fatigue during ongoing resuscitation.
Category: Pharmacology & Therapeutics
Keywords: alteplase, tPA, dabigatran, anticoagulant, apixaban, rivaroxaban (PubMed Search)
Posted: 4/3/2013 by Bryan Hayes, PharmD
(Updated: 4/5/2013)
Click here to contact Bryan Hayes, PharmD
A new recommendation in the 2013 Ischemic Stroke Guidelines provides guidance on what to do in patients taking new oral anticoagulants who are deemed eligible for IV fibrinolysis. Here is what the guidelines say:
Until further data are available, a history consistent with recent use of new oral anticoagulants generally precludes use of IV tPA.
Jauch EC, et al. Guidelines for the early management of patients with acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 2013;44(3):870-947. PMID 23370205
Follow me on Twitter (@PharmERToxGuy)
Category: Pediatrics
Keywords: Conjunctivitis (PubMed Search)
Posted: 4/5/2013 by Jenny Guyther, MD
Click here to contact Jenny Guyther, MD
Children frequently present with "pink eye" to the ED. When they do, parents often expect antibiotics. How many of these kids actually need them? Previous studies have shown approximately 54% of acute conjunctivitis was bacterial, but antibiotics were prescribed in 80-95% of cases.
A prospective study in a suburban children's hospital published in 2007, showed that 87% of the cases during the study period were bacterial. The most common type of bacteria was nontypeable H. influenza followed by S. pneumoniae.
Topical antibiotic treatment has been shown to improve remission rates by 6-10 days.
Patel et al. Clinical Features of Bacterial Conjunctivitis in Children. Academic Emergency Medicine 2007; 14:1-5.
Category: Pharmacology & Therapeutics
Keywords: Status epilepticus, Keppra, seizures, valproic acid, levetiracetam (PubMed Search)
Posted: 4/4/2013 by Ellen Lemkin, MD, PharmD
(Updated: 2/3/2026)
Click here to contact Ellen Lemkin, MD, PharmD
Trinka E. What is the evidence to use new intravenous AED in status epilepticus? Epilepsia 2011 52(Suppl 8):35-8.
Zelano J, Kumlien E. Levetiracetam as alternative stage two antiepileptic drug in status epilepticus: A systematic review. Seizure 2012. 21:233-6.
Category: International EM
Posted: 4/3/2013 by Walid Hammad, MD, MBChB
Click here to contact Walid Hammad, MD, MBChB
Spring is in the air... and so is rotavirus.
Area of the world affected:
· Diarrheal illnesses were responsible for 1.6 million deaths for children under 5 globally in 2002.
· This number has improved over the years, in part due to oral rehydration salts (ORS) which were developed for cholera.
Relevance to the US physician:
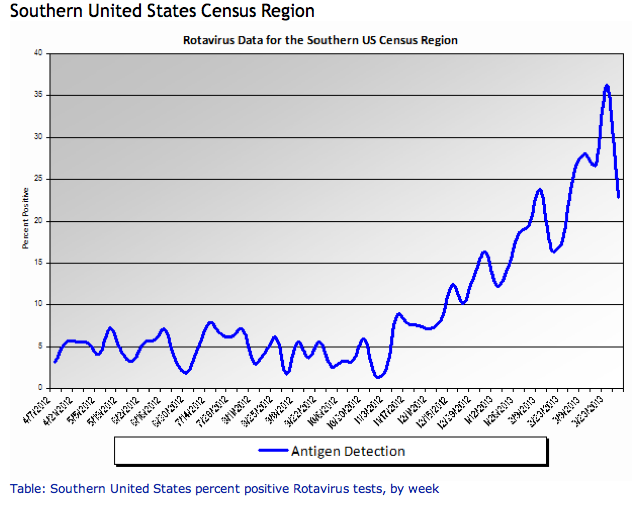
http://www.cdc.gov/surveillance/nrevss/rotavirus/region.html#top
· ORS are also important for rotavirus treatment and uncomplicated gastroenteritis in children and adults.
· Commercially prepared solutions have different concentrations of ingredients, but all will work as better treatment and rehydration than common household products like sports drinks and juice.
Bottom line:
Consider ORS in patients with uncomplicated acute gastroenteritis.
University of Maryland Section of Global Emergency Health
Author: Jennifer Reifel Saltzberg, MD, MPH
Atia AN, Buchman AL. Oral rehydration solutions in non-cholera diarrhea: a review. Am J Gastroenterol 2009;104(10):2596-604.
Sentongo, TA. The Use of Oral Rehydration Solutions in Children and Adults. Current Gastroenterology Reports 2004; 6:307–313.
Category: Critical Care
Posted: 4/2/2013 by Mike Winters, MBA, MD
(Updated: 2/3/2026)
Click here to contact Mike Winters, MBA, MD
Hormonal Dysfunction in Neurologic Injury
Vespa PM. Hormonal dysfunction in neurocritical patients. Curr Opin Crit Care 2013; 19:107-12.
Category: Visual Diagnosis
Posted: 4/1/2013 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
What's the Diagnosis?

Answer: Normal CXR...April Fool's Day ;)
Our international friends can learn more about April Fool'sDay here
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
