Category: Neurology
Keywords: nihss, nih stroke scale, posterior stroke, anterior stroke (PubMed Search)
Posted: 1/5/2011 by Aisha Liferidge, MD
(Updated: 2/3/2026)
Click here to contact Aisha Liferidge, MD
Category: Critical Care
Keywords: PRES, hypertensive crisis, seizures, visual loss, ecclampsia, hypertensive emergency, cyclopsporine, tacrolimus (PubMed Search)
Posted: 1/4/2011 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
Posterior reversible encephalopathy syndrome (PRES) is a syndrome of visual loss, headache, altered mental status, and seizures, typically with severe hypertension. PRES usually occurs with hypertensive encephalopathy or ecclampsia, although cyclosporin and tacrolimus use have been implicated.
PRES is due to a combination of endothelial damage, impaired auto-regulation and increased cerebral perfusion pressure. Classic CT and MRI findings are parietal-occipital, cerebellar, or brainstem cortical and subcortical edema.
Early recognition and symptomatic treatment is key; IV anti-hypertensives (hypertensive encephalopathy), anti-epileptics (seizures), IV magnesium and emergent delivery (ecclampsia), and discontinuing offending medications (cyclosporin and tacrolimus).
With treatment, partial to complete recovery is normal, although residual neurological and visual deficits may persist.
Pula, J. Posterior reversible encephalopathy syndrome. Current Opinion in Ophthalmology. 2008 vol. 19 (6) pp. 479-84
Category: Vascular
Posted: 1/3/2011 by Rob Rogers, MD
(Updated: 2/3/2026)
Click here to contact Rob Rogers, MD
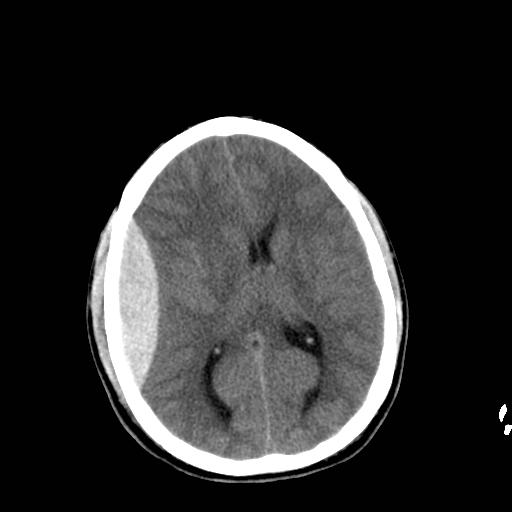
60 year-old male s/p assault. + LOC. Awake and normal neuro examination on arrival. Deteriorates in the ED after about an hour....
Diagnosis: Epidural Hematoma
Category: Cardiology
Keywords: therapeutic hypothermia, hypothermia, hypokalemia, cardiac arrest (PubMed Search)
Posted: 1/2/2011 by Amal Mattu, MD
(Updated: 2/3/2026)
Click here to contact Amal Mattu, MD
Induced hypothermia is associated with a decline in serum potassium levels. The cold myocardium is already mildly predisposed to arrhythmias, and the combination of hypokalemia + hypothermia appears to increase the risk of polymorphic ventricular tachycardia. Two simple measures should be taken during post-arrest therapeutic hypothermia:
1. Correct hypokalemia before and during cooling.
2. Monitor the patient's potassium level and QT interval during cooling, and correct as needed.
Mirzoyev SA, McLeod CJ, Bunch TJ, et al. Hypokalemia during the cooling phase of therapeutic hypothermia and its impact on arrhythmogenesis. Resuscitation 2010;81:1632-1636.
Category: Orthopedics
Keywords: peroneal, tendon, subluxation (PubMed Search)
Posted: 1/1/2011 by Michael Bond, MD
Click here to contact Michael Bond, MD
Peroneal Tendon Subluxation: The Other Ankle Sprain
Roth et al. Peroneal tendon subluxation: the other lateral ankle injury. Br J Sports Med (2010) vol. 44 (14) pp. 1047-53
Category: Toxicology
Keywords: naloxone, opioids (PubMed Search)
Posted: 12/30/2010 by Fermin Barrueto
(Updated: 2/3/2026)
Click here to contact Fermin Barrueto
Naloxone is the epitomy of an antidote with complete reversal of opioid toxicity within 60 seconds of administration. Remember your clinical endpoint should be respiratory effort. If you utilize "the vial" of either 0.4mg or 2mg and there is a higher probability of withdrawal and for acute lung injury. Here are some tips for administration:
1) IV Access: Try 0.1 mg or even 0.05 mg - anesthesiology typically doses naloxone in micrograms. Reversal is slower so you have to be patient. It is also not as dramatic so closely monitor respirations to see if you have improvement, that may be all that you get. These are probably patients that you don't want that awake anyways.
2) No IV Access: advantage of naloxone is it is bioavailable IV, intranasal and even by nebulizer. Here you want the dose to be 0.4mg to start for intranasal. Nebulizer is difficult to measure and probably safe to start with 2mg in the nebulizer container.
There is a difference when you know it is an opioid overdose and are reversing apnea versus a diagnostic administration to determine if it is opioid toxicity. In the latter instance you can rationalize the large dose - just be ready and be sure you are not in line of the possible projectile vomiting.
Category: Neurology
Keywords: seizure, seizure disorder, felbamate, antiepileptics (PubMed Search)
Posted: 12/29/2010 by Aisha Liferidge, MD
(Updated: 2/3/2026)
Click here to contact Aisha Liferidge, MD
Category: Critical Care
Posted: 12/28/2010 by Mike Winters, MBA, MD
Click here to contact Mike Winters, MBA, MD
Vancomycin Dosing in the Critically Ill Obese Patient
Medico CJ, Walsh P. Pharmacotherapy in the critically ill obese patient. Crit Care Clin 2010; 26:679-88.
Category: Cardiology
Keywords: isoproterenol, bradycardia, torsades de pointes (PubMed Search)
Posted: 12/26/2010 by Amal Mattu, MD
Click here to contact Amal Mattu, MD
Isoproterenol is a non-selective beta-1 and beta-2 agonist. The beta-1 effect produces an increase in heart rate, and the beta-2 effect produces mild vasodilation. Two times to consider its use are the following:
1. For overdriving pacing in cases of intermittent torsades de pointes when magnesium is ineffective.
2. For intractable bradycardia, this is another option besides dopamine or epinephrine. Because of the vasodilation, isoproterenol might be preferred to these other drugs when the bradycardia is accompanied by severe hypertension or when vasoconstrictors are not desired.
The drug is not commonly used anymore but is effective in treating persistent bradycardia or for overdrive pacing in patients with intermittent torsades de pointes when magnesium is ineffective. Be wary, though, that the beta-2 effect produces vasodilation so there may be a mild reduction in blood pressure when the drug is used.
Category: Orthopedics
Keywords: Sports medicine, Sudden cardiac death, Commotio Cordis, Defibrillation (PubMed Search)
Posted: 12/25/2010 by Brian Corwell, MD
(Updated: 2/19/2011)
Click here to contact Brian Corwell, MD
Commotio Cordis
Emergency medicine & sports medicine physicians often cover sporting events where athletes are at risk of commotio cordis
Palacio LE, Link MS. Commotio Cordis. 2009.
Category: Pediatrics
Posted: 12/25/2010 by Rose Chasm, MD
Click here to contact Rose Chasm, MD
Pediatrics Board Review
MedStudy
Category: Toxicology
Keywords: HF (PubMed Search)
Posted: 12/23/2010 by Fermin Barrueto
(Updated: 2/3/2026)
Click here to contact Fermin Barrueto
When you think of an acid or base causing a burn, you usually think of the local damage but there is one particular acid that causes systemic illness. Hydrofluoric Acid, found in your local Home Depot in brick/stone cleaning products, can cause severe illness despite a small total body surface area burn and exposure. A recent case report came out that illustrates how deadly HF can be. The reason is that this acid enters the body and chelates cations like calcium and potassium. The abstract is below but essentially hypocalcemia, hypokalemia leading to asystole 16hrs after exposure all from a 3% TBSA Burn - very impressive.
Wu ML, Deng JF, Fan JS.Survival after hypocalcemia, hypomagnesemia, hypokalemia and cardiac arrest following mild hydrofluoric acid burn. Clin Toxicology 2010
Category: Neurology
Keywords: lacunar infarct, stroke (PubMed Search)
Posted: 12/22/2010 by Aisha Liferidge, MD
(Updated: 2/3/2026)
Click here to contact Aisha Liferidge, MD
Category: Critical Care
Keywords: thrombocytopenia, critically0ill, sepsis, death, mortality, prognosis (PubMed Search)
Posted: 12/21/2010 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
The incidence and prevalence of thrombocytopenia in the ICU is poorly defined however, it has been found to be an independent predictor of death in the critically-ill. Increased mortality does not appear to be related to bleeding complications. On the other hand, survivors of critical illness tend to recover platelet faster as compared to non-survivors.
Thrombocytopenia in the critically-ill is a marker for systemic inflammation/infection although the exact mechanisms are unknown. Common risk factors associated with thrombocytopenia in the ICU population are:
Sepsis
Renal failure
High-illness severity
Organ dysfunction
Bottom line: Thrombocytopenia in the critically-ill is associated with increased mortality.
Hui, P., The Frequency and Clinical Significance of Thrombocytopenia Complicating Critical Illness: A Systematic Review. Chest. 2010 Nov 11. [Epub ahead of print]
Category: Cardiology
Keywords: Procainamide, ventricular tachycardia, amiodarone (PubMed Search)
Posted: 12/19/2010 by Amal Mattu, MD
(Updated: 2/3/2026)
Click here to contact Amal Mattu, MD
The September 5 2006 issue of Circulation contained a guideline, based on collaboration between the American Heart Assn, the American College of Cardiology, and the European Society of Cardiology, indicating that procainamide was preferable to amiodarone for the treatment of stable monomorphic ventricular tachycardia.
The 2010 AHA Guidelines have now also listed procainamide as the preferred drug for stable monomorphic ventricular tachycardia, giving it a Class IIa ("probably helpful") rating vs. amiodarone which has a Class IIb ("possibly helpful") rating. [thanks to Dr. Mike Abraham for pointing this out]
Procainamide is also the safest drug for use in tachydysrhythmias when an accessory pathway (e.g. Wolff-Parkinson-White syndrome) is present.
The caveat is that neither procainamide nor amiodarone should be used in the presence of a prolonged QTc.
Acute care physicians should (re-)familiarize themselves with the use of procainamide, and emergency departments should maintain quick access to this drug to stay up-to-date with current national and international guidelines.
ACC/AHA/ESC 2006 Guidelines for Management of Patients With Ventricular Arrhythmias and the Prevention of Sudden Cardiac Death — Executive Summary (many many authors) Circulation 2006;114:1088-1132.
Neumar RW, et al. Part 8: Adult Advanced Cardiovascular Life Support: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation 2010;122:S729-767.
Category: Orthopedics
Keywords: Septic Arthritis, Diagnosis (PubMed Search)
Posted: 12/18/2010 by Michael Bond, MD
(Updated: 12/19/2010)
Click here to contact Michael Bond, MD
Septic Arthritis
It is generally taught that if the synovial fluid white blood count (WBC) is less than 50,000 it is not septic, however, there is growing evidence that a clear delineation in the WBC between septic arthritis and inflammatory arthritis is not possible. In fact, inflammatory arthritis (rheumatoid and gout) actually increases your risk for septic arthritis and the two can coexist. Gram stains of the fluid only show organisms in 50% of those with septic arthritis so you also can not rely on them either. Inflammatory markers (CRP, ESR) can be elevated with inflammatory or septic arthritis so they too can not differentiate between the two.
In the end, because of the risk of permanent joint dysfunction, it is important to make the diagnosis on clinical grounds and treat empirically if you are unsure. Err on the sound of treatment. Serial joint aspirations to drain synovial fluid have the same outcomes as operative washout.
A recent article that discusses the concerns with making the diagnosis of septic arthritis is:
Mathews et al. Bacterial septic arthritis in adults. Lancet (2010) vol. 375 (9717) pp. 846-55
Mathews et al. Bacterial septic arthritis in adults. Lancet (2010) vol. 375 (9717) pp. 846-55
Category: Toxicology
Keywords: fomepizole, disulfiram (PubMed Search)
Posted: 12/17/2010 by Fermin Barrueto
(Updated: 2/3/2026)
Click here to contact Fermin Barrueto
The answer was fomepizole would be the treatment for life-threatening disulfiram reaction. Blocks Alcohol Dehydrogenase and ironically prevent metabolism of ethanol and prolong intoxication.
I forgot how many see the pearls and the response was overwhelming. That was great and cost a me a little more. There were two winners:
Katie Baugher, PGY-1
Ari Keslter
Please email me how to best send you the gift certificate.
Category: Toxicology
Keywords: disulfiram reaction (PubMed Search)
Posted: 12/16/2010 by Fermin Barrueto
(Updated: 2/3/2026)
Click here to contact Fermin Barrueto
There are medications, if taken with ethanol, will cause a disulfiram reaction. This reaction results from inhibition of aldehyde dehydrogenase, the enzyme in ethanol metabolism that breaks acetaldehyde to acetic acid. The increase in acetaldehyde results in nausea, vomiting, diarrhea, flushing, palpitations and orthostatic hypotension. So if you prescribe a patient with any of these medications you must make certain to tell them NOT to drink any ethanol - that includes cough/cold preparations that have ethanol:
Antibiotics: Metronidazole(Flagyl), Trimethoprim-sulfamethoxazole (Bactrim)
Sulfonylureas: Chlorpropamide and tolbutamide
These have possible reactions: griseofulvin, quinacrine, procarbazine, phentolamine, nitrofurantoin
Bonus Question: $10 Starbuck's Gift Card for first person that emails me with the answer to this question
What treatment could you give to someone suffering from a life threatening disulfiram reaction that biochemically should cure him?
Category: Neurology
Keywords: MS, multiple sclerosis, lhermitte's phenomenon, sensory symptom (PubMed Search)
Posted: 12/15/2010 by Aisha Liferidge, MD
Click here to contact Aisha Liferidge, MD
Category: Critical Care
Posted: 12/15/2010 by Mike Winters, MBA, MD
(Updated: 2/3/2026)
Click here to contact Mike Winters, MBA, MD
The Importance of Antibiotic Timing for Sepsis and Septic Shock
Funk DJ, Kumar A. Antimicrobial therapy for life-threatening infections: Speed is life. Crit Care Clin 2011; 27:53-76.
