Category: Orthopedics
Keywords: Knee Dislocation, Prosthetic (PubMed Search)
Posted: 4/9/2011 by Michael Bond, MD
(Updated: 2/3/2026)
Click here to contact Michael Bond, MD
Knee dislocations are uncommon, and prosthetic knee dislocations even rarer. Some general facts about prosthetic knee dislocations are:
Wang CJ, Wang HE. Dislocation of total knee arthroplasty: a report of 6 cases with 2 patterns of instability. Acta Orthop Scand 1997;68:282-285.
Stiehl JB, Komistek RD, Dennis DA, et al. Fluoroscopic analysis of kinematics after posterior-cruciate-retaining knee arthroplasty. J Bone Joint Surg Br 1995;77:884-889.
Category: Pediatrics
Keywords: magnesium toxicity, neonatal hypotonia, neonate, intubation, neonatal resuscitation (PubMed Search)
Posted: 4/8/2011 by Adam Friedlander, MD
Click here to contact Adam Friedlander, MD
So the magnesium didn't work, and the baby is on the way! You're prepared with everything you need for the delivery from bulb suction to a tripod for Dad's camera... But what is going to special about this baby?
Babies born to mothers who received magnesium therapy for any reason are at risk for hypotonia and severe respiratory depression.
Special thanks to Dr. Mimi Lu for the reference above
Category: Toxicology
Keywords: radiation, iodide, KI, thyroid, iodine-131 (PubMed Search)
Posted: 4/7/2011 by Ellen Lemkin, MD, PharmD
Click here to contact Ellen Lemkin, MD, PharmD
· In the event a nuclear power plant accident, people may be exposed to a mixture of radioactive products. The main radionuclides representing health risk are radioactive caesium and radioactive iodine.
· Iodine-131 is concentrated in the thyroid gland and may eventually lead to development of thyroid nodules and thyroid cancer.
· Radioiodine uptake by the thyroid can be blocked by taking potassium iodide (KI) pills or solution, preventing these effects.
· KI should not be taken in the absence of a clear risk of exposure to a potentially dangerous level of radioactive iodine because KI can cause allergic reactions, skin rashes, salivary gland inflammation, hyperthyroidism or hypothyroidism.
· Since radioactive iodine decays rapidly, current estimates indicate there will not be a hazardous level of reaching the United States from this accident.
· There are three FDA approved KI products: Iosat, Thyrosafe and ThyroShield.
http://www.who.int/hac/crises/jpn/faqs/en/index2.html
briefs.com/briefs/ATAORG/ATAORG031611.php
Pharmacist's Letter April 2011 Vol 27(4) 19-20.
Category: Neurology
Keywords: trigeminal neuralgia, headaches (PubMed Search)
Posted: 4/6/2011 by Aisha Liferidge, MD
(Updated: 2/3/2026)
Click here to contact Aisha Liferidge, MD
Category: Infectious Disease
Keywords: infection, cirrhosis (PubMed Search)
Posted: 4/4/2011 by Rob Rogers, MD
(Updated: 2/3/2026)
Click here to contact Rob Rogers, MD
Hemorrhagic bullae in an ill-appearing patient with underlying cirrhosis should prompt consideration for an invasive infection due to Vibrio vulnificus.
V. Vulnificus is a gram negative rod and causes a highly lethal infection in patients with cirrhosis.
Antibiotics for these patients should include coverage for this organism. This should include doxycycline and a third genaration cephalosporin.
1. Evidence-Based Medicine: 500 Clues to Diagnosis and Treatment, Ellerin and Diaz
2. CDC
Category: Cardiology
Keywords: prosthetic, valve, paravalvular leak, hemolysis (PubMed Search)
Posted: 4/3/2011 by Amal Mattu, MD
Click here to contact Amal Mattu, MD
Severe hemolysis/hemolytic anemia in a patient with a prosthetic cardiac valve suggests a paravalvular leak. In this condition, a portion of the valve becomes dislodged from the valve annulus. It can occur immediately after surgery or delayed if from endocarditis. Paravalvular leaks are more common with mechanic valves. Patients may also present with sudden pulmonary edema.
The treatment will focus on management of the pulmonary edema and prompt surgical repair.
Category: Pharmacology & Therapeutics
Keywords: enoxaparin, VTE, obese, low molecular weight heparin (PubMed Search)
Posted: 4/1/2011 by Bryan Hayes, PharmD
(Updated: 4/2/2011)
Click here to contact Bryan Hayes, PharmD
For patients with normal renal function, enoxaparin dosing for treatment of VTE is 1 mg/kg subcut every 12 hours OR 1.5 mg/kg subcut every 24 hours.
Studies have evaluated dosing for patients weighing up to 190 kg and found the 1 mg/kg q 12 hours dose to be safe and effective. It can even be used for patients heavier than 190 kg, but anti-Xa monitoring is recommended.
Nutescu EA, Spinler SA, Wittkowsky A, et al. Low-molecular-weight heparins in renal impairment and obesity: available evidence and clinical practice recommendations across medical and surgical settings. Ann Pharmacother 2009;43(6):1064-83.
Category: Toxicology
Keywords: phenytoin, vinca alkaloids, (PubMed Search)
Posted: 3/31/2011 by Fermin Barrueto
(Updated: 2/3/2026)
Click here to contact Fermin Barrueto
Extravasation from radiocontrast, phenytoin and promethazine have resulted in significant tissue necrosis sometimes requiring surgical debridement and reconstructive plastic surgery.
Pearl: Keep the infiltrated peripheral IV in and inject hyaluronidase 3-5mL (150U/mL) into the same subcutaneous pocket of medication. Hyaluronidase will increase the systemic absorption of the drug, decreasing its time in the SQ tissue. Extremely safe drug (we have the enzyme in our body) and has been used in neonates as well as adults. Also used for SQ hydration in palliative care and pediatrics.
Controversy: Hot vs Cold - Heat will cause vasodilation and hopefully increase systemic absorption but will likely also increase SQ spread possibly increasing the surface area of injury. Cold will cause vasoconstriction and decrease size of injury however will concentrate drug and possibly worsen the local injury.
1: Sokol DK, Dahlmann A, Dunn DW. Hyaluronidase treatment for intravenous phenytoin extravasation. J Child Neurol. 1998 May;13(5):246-7. 2: Cochran ST, Bomyea K, Kahn M. Treatment of iodinated contrast material extravasation with hyaluronidase. Acad Radiol. 2002 Aug;9 Suppl 2:S544-6. 3: Few BJ. Hyaluronidase for treating intravenous extravasations. MCN Am J Matern Child Nurs. 1987 Jan-Feb;12(1):23. 4: Kuensting LL. Treatment of intravenous infiltration in a neonate. J Pediatr Health Care. 2010 May-Jun;24(3):184-8. Epub 2010 Mar 20. 5: Raszka WV Jr, Kueser TK, Smith FR, Bass JW. The use of hyaluronidase in the treatment of intravenous extravasation injuries. J Perinatol. 1990 Jun;10(2):146-9.
Category: Neurology
Keywords: myasthenia graves, mg, intubation (PubMed Search)
Posted: 3/30/2011 by Aisha Liferidge, MD
(Updated: 2/3/2026)
Click here to contact Aisha Liferidge, MD
Category: Critical Care
Keywords: bilevel ventilation, bipap, cpap, respiratory failure, respiratory distress, copd, acute pulmonary edema (PubMed Search)
Posted: 3/29/2011 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
Emergency Medicine physicians are gaining experience with non-invasive ventilation (i.e., Bi-level ventilation and continuous positive-pressure ventilation) in managing respiratory distress and failure. Although NIV is commonly used across a variety of pathologies, the best data exists for use with COPD exacerbation and cardiogenic pulmonary edema (CHF, not an acute MI)
Although other indications for NIV have been studied, the data is less robust (eg., smaller study size, weak control groups, etc.). If there are no contraindications, however, many experts still support a trial of NIV in the following populations:
Failure to clinically improve during a NIV trial should prompt invasive mechanical ventilation.
Keenan, S. et al. Clinical practice guidelines for the use of noninvasive positive-pressure ventilation and noninvasive continuous positive airway pressure in the acute care setting. CMAJ. 2011 Feb 22;183(3):E195-214. Epub 2011 Feb 14.
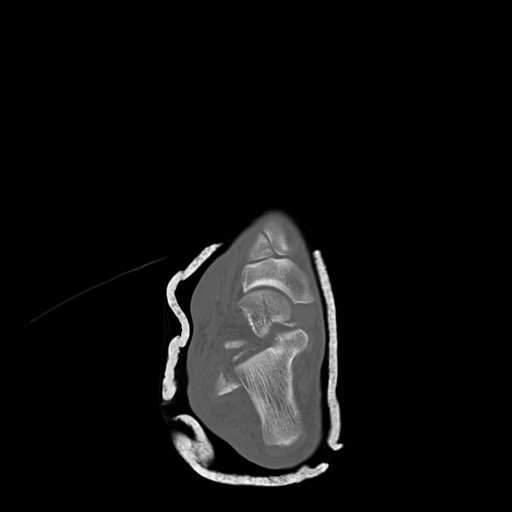
Category: Visual Diagnosis
Posted: 3/27/2011 by Haney Mallemat, MD
(Updated: 3/28/2011)
Click here to contact Haney Mallemat, MD
25 year old male presents after falling from 10 feet and landing on right shoulder. Diagnosis?

Yes...the shoulder is dislocated, but did you notice anything else? (see figure 1)
Glenoid Fossa Fracture: (Image submitted by Dr. George Kochman)
Fractures of the glenoid fossa occur when the head of the humerus collides with the glenoid margin; classically, by a laterally directed force. Although less than 10% of glenoid fossa fractures result in significant displacement, surgical repair is indicated if:

Schmidt, J. Scapular Fracture. eMedicine. January 12, 2011.
http://emedicine.medscape.com/article/826084-overview
Category: Cardiology
Keywords: C-section, perimortem, cardiac arrest (PubMed Search)
Posted: 3/28/2011 by Amal Mattu, MD
(Updated: 2/3/2026)
Click here to contact Amal Mattu, MD
Aortocaval compression occurs often when gestational age is > 20 weeks. This compression significantly compromises the chances of maternal survival in cardiac arrest. Because it is often difficult to know the exact gestational age, it is commonly recommended that emergency C-section in maternal cardiac arrest be performed when the fundus extends above the level of the umbilicus.
Vanden Hoek TL, et al. Part 12: Cardiac arrest in special situations: 2010 American Heart Association guidelines for cardiopulumonary resuscitation and emergency cardiovascular care. Circulation 2010;122[suppl 3]:S829-S861.
Category: Orthopedics
Keywords: Gout, uric acid (PubMed Search)
Posted: 3/26/2011 by Brian Corwell, MD
(Updated: 2/3/2026)
Click here to contact Brian Corwell, MD
GOUT part 1
Gout is an inflammatory arthritis that classically affects the first metatarsal phalangeal joint
Gout prefers cool ambient temperature hence gouty tophi prefer the great toe (one of the coldest parts of the body) and avoids "warmer" joints such as the hip and shoulder.
Remember that gout can affect other joints as well (elbow, wrist, knee and ankle) and can cause painful bursitis and tendonitis
Multiple joints can be involved simultaneously (leading to confusing with RA and OA)
The involved joint will often be red, hot, swollen and very painful leading to easy confusion with cellulitis and or a septic arthritis
Diagnose gout by demonstrating monosodium urate crystals in the synovial fluid.
**Remember previous pearl by Dr. Bond regarding the coexistence of gout with septic joint**
Serum uric acid levels are commonly elevated but can be normal or even low
Use caution with this test because asymptomatic hyperuricemia is much more common than gout
Category: Pediatrics
Posted: 3/25/2011 by Rose Chasm, MD
(Updated: 2/3/2026)
Click here to contact Rose Chasm, MD
Pediatrics Board Review Core Curriculum, 1st edition
MedStudy
Category: Neurology
Keywords: correction, NMS, neuroleptic malignant syndrome (PubMed Search)
Posted: 3/24/2011 by Aisha Liferidge, MD
(Updated: 2/3/2026)
Click here to contact Aisha Liferidge, MD
Note that yesterday's Neurology pearl should have read as follows -
Amongst others, diagnostic criteria for NMS includes:
Exposure to a dopamine ANTAGONIST (NOT AGONIST) or dopamine agonist withdrawal within past 72 hours.
Apologies for the type-o.
Category: Toxicology
Keywords: antipsychotics, thromboembolism (PubMed Search)
Posted: 3/24/2011 by Fermin Barrueto
Click here to contact Fermin Barrueto
Could this be another risk factor for DVT/PE. Maybe not yet but it is worth mention. A recent observatioal study in BMJ showed that there was an associated increase with DVT or PE. From a database of 25,532 patients over a 3 year period of time and finding match controls, the results were:
Limitations were this is was an observational study with missing data. BMI was missing in these records and it is always difficult to tease out the multiple medications these patients are on. Also don't have a great biological mechanism (yet). Still makes you go hmm....
Antipsychotic drugs and risk of venous thromboembolism, Parker, BMJ, 2010.
Category: Neurology
Keywords: NMS, neuroleptic malignant syndrome (PubMed Search)
Posted: 3/23/2011 by Aisha Liferidge, MD
Click here to contact Aisha Liferidge, MD
- Exposure to dopamine agonist or dopamine agonist withdrawal within past 72 hours
- Hyperthermia
- Rigidity
- Mental status alteration
- Elevated creatinine phosphokinase
- Sympathetic nervous system lability (2 or more of the following: elevated blood pressure, fluctant blood pressure, urinary incontinence, diaphoresis)
- Tachycardia and tachypnea
- Negative work-up for infectious, metabolic, neurologic, or toxic etiologies.
Category: Critical Care
Posted: 3/22/2011 by Mike Winters, MBA, MD
Click here to contact Mike Winters, MBA, MD
Aspiration Pneumonitis and Pneumonia
Ragavendran K, Nemzek J, Napolitano LM, Knight PR. Aspiration-induced lung injury. Crit Care Med 2011; 39:818-26.
Category: Geriatrics
Keywords: geriatric, elderly, rib fractures (PubMed Search)
Posted: 3/20/2011 by Amal Mattu, MD
Click here to contact Amal Mattu, MD
Rib fractures are associated with significant morbidity and mortality in the elderly, and the risk increases dramatically with each successive rib fractured. An elderly patient with 3 rib fractures has a mortality of 20% and risk of pneumonia is 31%. As a general rule, you should really think twice about discharging home any elderly patients with rib fractures.
[credit to Dr. Joe Martinez for bringing forth this information]
Bulger EM, Arneson MA, Mock CN, et al. Rib fractures in the elderly. J Trauma 2000;48:1040-1046.
Category: Orthopedics
Posted: 3/12/2011 by Michael Bond, MD
(Updated: 3/19/2011)
Click here to contact Michael Bond, MD
Talar Neck Fractures
Have a high rate of avascular necrosis (AVN), nonunion, and arthritis. Almost all require ORIF