Category: Critical Care
Keywords: delirium, dementia, ICU, (PubMed Search)
Posted: 10/25/2010 by Haney Mallemat, MD
(Updated: 2/3/2026)
Click here to contact Haney Mallemat, MD
Increasing literature demonstrates ICU delirium is bad. Delirium in mechanically ventilated patients is an independent predictor for long-term cognitive defects (e.g., managing money, following detailed instructions, reading maps, and developing dementia). The cited study found 80% of patients with ICU delirium had cognitive dysfunction at three months, and 70% had residual dysfunction at one year (33% had severe dysfunction).
You must be aggressive to prevent delirium:
- Implement daily assessment tools (e.g., CAM-ICU)
- Daily awakening and spontaneous breathing trials
- Early patient mobilization
- Aggressive pharmacological treatment of delirium
- For more information: www.icudelirium.org
Delirium as a predictor of long-term cognitive impairment in survivors of critical illness. Girard, T., et al. Crit Care Med. 2010 Jul;38(7):1513-20.
Category: Cardiology
Keywords: long QT, torsade, torsades, torsade de pointe, magnesium (PubMed Search)
Posted: 10/24/2010 by Amal Mattu, MD
Click here to contact Amal Mattu, MD
Magnesium is considered a mainstay of treatment of prolonged QT syndrome leading to torsade de pointe, including those cases caused by drugs. The exact mechanism of action is unknown, though it is thought to stabilize the myocardium. Interestingly, magnesium infusions will not necessarily change the heart rate or QT interval on ECG.
The dose is 2 g IV followed by an infusion (similar to treatment of eclampsia/preeclampsia). The bolus should be given slowly if the patient is relatively stable, but can be pushed over 1 minute in a patient with ongoing torsade that is not responding to electricity.
Charlton NP, Lawrence DT, Brady WJ, et al. Termination of drug-induced torsades de pointes with overdrive pacing. Am J Emerg Med 2010;28:95-102.
Category: Orthopedics
Keywords: EPIDURAL SPINAL CORD COMPRESSION, CAUDA EQUINA SYNDROME (PubMed Search)
Posted: 10/22/2010 by Brian Corwell, MD
(Updated: 2/3/2026)
Click here to contact Brian Corwell, MD
Epidural compression syndrome encompasses spinal cord compression, cauda equina syndrome, & conus medullaris syndrome.
Causes include:
Measurement of a post-void bladder residual volume tests for the presence of urinary retention with overflow incontinence (a common, though late finding) (sensitivity of 90%, specificity of 95%). Large post-void residual volumes (>100 mL) indicate a denervated bladder with resultant overflow incontinence and suggest significant neurologic compromise. The probability of cauda equina syndrome in patients without urinary retention is approximately 1 in 10,000.
Use this in your daily practice!!
The administration of glucocorticoids can minimize ongoing neurologic damage from compression & edema until definitive therapy can be initiated. The optimal initial dose and duration of therapy is controversial, with a recommended dose range of dexamethasone anywhere from 10 to 100 mg intravenously. Consider traditional dosing (dexamethasone 10 mg) for those with minimal neurologic dysfunction, & reserve the higher dose (dexamethasone 100 mg) for patients with profound or rapidly progressive symptoms, such as paraparesis or paraplegia.
1. Deyo RA, Rainville J, Kent DL. What can the history and physical examination tell us about low back pain? JAMA 1992;268:760–5.
2. Gregory D, Seto C, Wortley G, et al. Acute lumbar disk pain: navigating evaluation and treatment choices. Am Fam Physician 2008;78:835–42.
3. Loblaw DA, Laperriere NJ. Emergency treatment of malignant extradural spinal cord compression: an evidence-based guideline. J Clin Oncol 1998;16:1613–24.
Category: Pediatrics
Posted: 10/22/2010 by Rose Chasm, MD
Click here to contact Rose Chasm, MD
Colic
Category: Toxicology
Keywords: intralipid (PubMed Search)
Posted: 10/21/2010 by Fermin Barrueto
(Updated: 2/3/2026)
Click here to contact Fermin Barrueto
Category: Neurology
Keywords: concussion, traumatic brain injury, minor traumatic brain injury (PubMed Search)
Posted: 10/20/2010 by Aisha Liferidge, MD
(Updated: 2/3/2026)
Click here to contact Aisha Liferidge, MD
Category: Critical Care
Posted: 10/19/2010 by Mike Winters, MBA, MD
(Updated: 2/3/2026)
Click here to contact Mike Winters, MBA, MD
Ketamine for RSI in Hemodynamically Unstable ED Patients
Morris C, et al. Anaesthesia in haemodynamically compromised emergency patients: does ketamine represent the best choice of induction agent? Anaesthesia 2009; 64: 532-9.
Category: Cardiology
Keywords: early repolarization, ST segment elevation, STEMI, ST elevation (PubMed Search)
Posted: 10/17/2010 by Amal Mattu, MD
Click here to contact Amal Mattu, MD
ECG early repolarization (or sometimes referred to as "benign early repolarization" or BER) is a common finding on ECGs, especially in young patients. It is a common "confounding" pattern when trying to identify STEMI. Here are some pearls that help in distinguishing BER vs. true STEMI. Remember at the outset, though, nothing in medicine is 100%....and that getting old ECGs or getting serial ECGs can be incredibly helpful.
1. BER is ONLY allowed to have STE that is concave upwards. If you ever see STE that is convex upwards (like a tombstone) or horizontal, it MUST be a STEMI.
2. BER should not have ST-segment depression, except maybe in aVR and V1. If there is ST depression in any of the other 10 leads, it is almost definitely a STEMI.
3. If you see STE in the inferior leads, compare the STE in lead II vs. lead III. If the STE in lead III is greater than the STE in lead II, it rules out BER....gotta be STEMI.
4. STE from BER is usually maximal in the mid precordial leads. You CAN have STE in the inferior leads with BER also, but you really shouldn't have STE isolated to the inferior leads. In other words, BER can have (1) STE in the precordial leads alone, or (2) STE in the precordial + inferior leads, but it should never have STE isolated to the inferior leads, and also the STE in the precordial leads should be more prominent than the STE in the inferior leads.
5. BER should usually not have STE > 5 mm. However, I've seen some occasional exceptions when the patient has large voltage QRS complexes.
Category: Orthopedics
Keywords: Subungual Hematomas (PubMed Search)
Posted: 10/16/2010 by Michael Bond, MD
(Updated: 2/3/2026)
Click here to contact Michael Bond, MD
Subungual Hematomas:
Category: Pediatrics
Keywords: Ondansetron, Oral Rehydration, Therapy, vomiting, pediatrics (PubMed Search)
Posted: 10/15/2010 by Adam Friedlander, MD
(Updated: 10/16/2010)
Click here to contact Adam Friedlander, MD
You may already love ondansetron, but consider using it ORALLY followed by PO hydration in children with vomiting.
The size of the study that showed this: N of just under 35,000.
But don't skimp on dosing. The dose is 0.1 - 0.15mg/kg, and you don't reach a max until 8mg. To put this in perspective, a scrawny 115lb (about 53kg) middle school tennis player would get 8mg, an initial dose often reserved for chemo patients in the adult ED.
Sturm JJ, Hirsh DA, Schweickert A, Massey R, Simon HK. Ondansetron use in the pediatric emergency department and effects on hospitalization and return rates: are we masking alternative diagnoses? Ann Emerg Med. 2010 May;55(5):415-22. Epub 2010 Jan 19.
Category: Toxicology
Keywords: Intralipid, fat emulsion (PubMed Search)
Posted: 10/14/2010 by Bryan Hayes, PharmD
(Updated: 2/3/2026)
Click here to contact Bryan Hayes, PharmD
Emerging evidence supports using intravenous fat emulsion (Intralipid) therapy for various drug overdoses, particularly those that are lipophilic. Within seconds to minutes of administration, toxic cardiovascular effects are reversed, including return of spontaneous circulation in cardiac arrest patients. Central nervous system effects also tend to improve.
Lipophilic agents for which there has been success include:
Bottom line: Consider intralipid therapy early in the course of a hemodynamically unstable patient with suspected overdose. Give a bolus of 1.5 mL/kg of 20% lipid emulsion over 1-2 minutes.
Category: Neurology
Keywords: stroke, cerebral edema, tPA, hemorrhage, NIHSS (PubMed Search)
Posted: 10/13/2010 by Aisha Liferidge, MD
(Updated: 2/3/2026)
Click here to contact Aisha Liferidge, MD
--- High NIH Stroke Scale scores.
--- Large areas of infarct.
--- Cerebellar infarcts.
--- Extended time to tPA administration.
--- Previous stroke.
--- Older age.
Category: Critical Care
Keywords: asthma, heliox, airway (PubMed Search)
Posted: 10/12/2010 by Haney Mallemat, MD
(Updated: 2/3/2026)
Click here to contact Haney Mallemat, MD
Heliox is a mixture of oxygen and helium resulting in a gas less dense than air. In asthma, airway resistance causes turbulent airflow which increases the work of breathing. Heliox reduces airway resistance by increasing laminar airflow.
Benefits:
Better lung mechanics
Improved nebulizer delivery
Few known side-effects/complications
Drawbacks:
Expensive
Contraindicated in hypoxemic patients.
Paucity of large prospective randomized trials.
McGarvey JM, Pollack CV. Heliox in Airway Management. Emerg Med Clin North Am. 2008 Nov;26(4):905-20, viii.
Category: Orthopedics
Keywords: joint, documentation, physical examination (PubMed Search)
Posted: 10/9/2010 by Brian Corwell, MD
(Updated: 2/3/2026)
Click here to contact Brian Corwell, MD
Previous pearls have described tips for smart and safe documentation of typical ED complaints such as chest pain. Properly assessing and documenting orthopedic complaints is likewise very important. No evaluation or chart is complete if it does not include include the following 7 components:
The joint above
The joint below
Motor
Sensory
Vascular
Skin
Compartments
The joint above/below is important in cases of shoulder and hip pain actually being radicular pain (from the neck and back respectively). Also, hip pain from trauma may be due to a femur fracture for example.
For motor and sensory evaluation, test the most distal isolated innervation of a particular nerve (L5 - great toe dorsiflexion for example).
Note distal pulses and check ABIs for injuries with potential subtle vascular findings.
Note intact skin especially in cases where the joint will be covered by a splint.
Note "soft" compartments especially in cases of forearm and lower leg fractures.
Category: Critical Care
Keywords: endotracheal intubation, medication, acls, resuscitation (PubMed Search)
Posted: 10/7/2010 by Ellen Lemkin, MD, PharmD
Click here to contact Ellen Lemkin, MD, PharmD
EMS in Maryland has REMOVED endotracheal medication administration from its ADULT protocols
This is due to:
Category: Neurology
Keywords: diplopia, cranial nerve palsy, monocular diplopia, binocular diplopia (PubMed Search)
Posted: 10/6/2010 by Aisha Liferidge, MD
(Updated: 2/3/2026)
Click here to contact Aisha Liferidge, MD
Category: Critical Care
Posted: 10/5/2010 by Mike Winters, MBA, MD
(Updated: 2/3/2026)
Click here to contact Mike Winters, MBA, MD
Respiratory Distress in the Ventilated ED Patient
Santanilla JI, Daniel B, Yeow ME. Mechanical ventilation. Emerg Med Clin N Am 2008;26:849-862.
Category: Med-Legal
Keywords: chest pain (PubMed Search)
Posted: 10/4/2010 by Rob Rogers, MD
(Updated: 2/3/2026)
Click here to contact Rob Rogers, MD
Chest pain is a very high risk chief complaint in emergency medicine. And although we are told by the experts what we should write on the chart, we often struggle with finding time to do so.
Given that we can't pick up every MI, dissection, and PE, what things can we document in the chart that prove we are thorough and that we have thought about a diagnosis? And how can we document a "protective thought process" without taking too much time to do so?
Consider documenting these on your chest pain charts:
Documenting key pertinent negative comments in the chart shows that you are thinking (and considering MI, Aortic Dissection, and PE), and whenever this can be shown in a chart, there is more ammunition for the defense attorney.
Category: Cardiology
Keywords: oxygen, acute myocardial infarction (PubMed Search)
Posted: 10/3/2010 by Amal Mattu, MD
Click here to contact Amal Mattu, MD
The traditional teaching has always been to use supplemental high-flow oxygen routinely for patients with acute MI. I recall specifically being taught in residency by EM, IM, and cardiology attendings that every acute MI patient should receive a minimum of 6 liters of supplemental oxygen via nasal canula, if not 100% oxygen, regardless of the initial pulse oximetry.
Mounting evidence, however, is demonstrating that the use of supplemental oxygen in patients that are "normoxic" (i.e. the production of "hyperoxia") is detrimental. Studies are demonstrating that there is no improvement in mortality or prevention of dysrhythmias; and in fact a trend towards increased mortality when patients are hyperoxic. This detrimental effect is likely the result of coronary vasoconstriction which occurs through several different mechanisms, all induced by hyperoxia. Oxygen, it turns out, is a vasoactive substance.
The takeaway point is very simple: if an AMI patient is not hypoxic, don't go overboard with the supplemental oxygen!
[Moradkhan R, Sinoway LI. Revisiting the role of oxygen therapy in cardiac patients. J Am Coll Cardiol 2010;56:1013-1016.]
Category: Orthopedics
Keywords: Patellofemoral syndrome (PubMed Search)
Posted: 10/2/2010 by Michael Bond, MD
Click here to contact Michael Bond, MD
Patellofemoral Syndrome (Chondromalacia Patella)
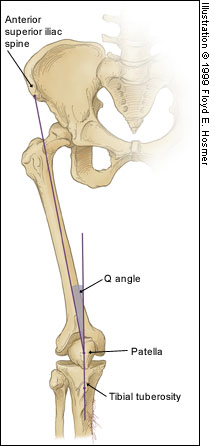
Juhn MS et al. Patellofemoral pain syndrome: a review and guidelines for treatment. Am Fam Physician. (1999)
